General Information about Zyrtec
Zyrtec belongs to a class of medicine referred to as antihistamines. Its primary mechanism of action is to block the results of histamine, a chemical released by the body throughout an allergic reaction. Histamine is liable for causing the symptoms of hay fever and hives, similar to sneezing, itching, and irritation. By blocking the consequences of histamine, Zyrtec helps to alleviate these symptoms and provide relief to those that suffer from allergies.
While Zyrtec is mostly well-tolerated, some people might experience mild unwanted effects such as drowsiness, dry mouth, and headache. These unwanted effects are often short-term and can subside after a couple of days of taking the medicine. However, in the occasion that they persist or turn into severe, it is important to communicate to a healthcare provider.
One of the main benefits of Zyrtec is its long-lasting effects. It is a once-a-day medicine, which means that a single dose can provide aid from symptoms for the complete day. This is beneficial for individuals who lead busy lives and do not have time to take multiple doses throughout the day. Zyrtec additionally has a quick onset of action, with many individuals experiencing relief from signs inside 20-30 minutes after taking the medicine.
Zyrtec, additionally known by its generic name cetirizine, is a popular antihistamine treatment used to treat hay fever and hives. Hay fever, also recognized as allergic rhinitis, is a standard situation during which the immune system overreacts to allergens in the air, inflicting symptoms similar to sneezing, itching, and a runny nostril. Hives, also known as urticaria, is a skin situation characterized by itchy, raised welts on the skin. Zyrtec is a highly efficient medication in relieving the signs of these situations and has been broadly used for many years.
Zyrtec is available in multiple forms, together with tablets, chewable tablets, and syrup, making it simple for individuals of all ages to take. The beneficial dosage for adults and youngsters over the age of 6 is 10mg as soon as every day, whereas kids between the ages of 2-6 should take 5mg as quickly as a day. Zyrtec can additionally be obtainable over the counter, making it simply accessible for those who do not have a prescription from their physician.
In conclusion, Zyrtec is a highly efficient treatment for the remedy of hay fever and hives. With its long-lasting results, quick onset of action, and numerous types of administration, it's a handy and in style choice for these affected by allergic reactions. If you expertise symptoms of hay fever or hives, seek the guidance of together with your healthcare supplier to see if Zyrtec may be an acceptable treatment option for you.
In rare cases, Zyrtec might work together with other medications, similar to sedatives, tranquilizers, and sure antidepressants. It is important to inform your doctor about all of the medications you're at present taking before beginning Zyrtec.
Zyrtec can also be protected for use in being pregnant and whereas breastfeeding. However, as with all medication, it may be very important consult with a doctor before taking Zyrtec during pregnancy or whereas breastfeeding to ensure it's protected for both the mother and the infant.
Nonossifying fibroma occurs less commonly in the upper extremity allergy testing worcester zyrtec 5 mg lowest price, where it may be found in the proximal humerus and distal radius. Occasionally the lesions may be multifocal, simultaneously involving several symmetric metaphyseal sites, most frequently in the long bones of the lower extremity. The radiographic findings are specific, and the diagnosis can be made with certainty if the lesion is present in a typical skeletal site and appropriate age group. The rarity of both fibrous cortical defects and nonossifying fibroma on radiographs of adults is indirect evidence of a natural history characterized by spontaneous regression of most of these lesions over time. The lesion is usually incidentally identified on radiographs obtained for other reasons such as trauma. There is no matrix mineralization, but in older patients evidence of bone sclerosis can accompany healing of the lesion. The distance from the growth plate usually increases with age and in older adolescents. Gross Findings When evaluated intact in its setting, nonossifying fibroma is an eccentric and cortically based lesion with an inner boundary that is scalloped and distinctly demarcated. There may be evidence of cystic change, hemorrhage, or extensive necrosis, particularly in association with pathologic fracture of larger lesions. Fresh hemorrhage and cystic change similar to that seen in aneurysmal bone cyst may be present. Secondary aneurysmal bone cyst formation can lead to rapid enlargement and a "blowout" expansion into the soft tissue. With low power magnification, it is possible to observe the localization of prominent giant cell reaction to areas of hemorrhage. Ghosts of giant cells and patterns demonstrating the storiform architecture of the lesion may be perceived in areas of necrosis. Necrosis, as well as the presence of occasional normal mitotic figures, are not worrisome features in otherwise typical nonossifying fibroma and should not be considered as microscopic features of malignancy. In fibula, nonossifying fibroma often involves the entire medullary cavity and does not show eccentric features. Scalloped borders and incomplete trabeculation are typical of nonossifying fibroma. A, Anteroposterior radiograph showing an eccentric lesion in the distal tibial diaphysis with sclerotic margins and expanded overlying cortex. D and E, Sagittal and coronal T1-weighted magnetic resonance images showing low density eccentric lesion of distal tibial metaphysis with well demarcated sclerotic scalloped margins. A, Anteroposterior radiograph showing an eccentric lytic lesion of the proximal tibial metaphysis with fine trabeculations and expanded overlying cortex. E, Low power microphotograph of nonossifying fibroma showing fibrohistiocytic proliferation with storiform pattern (E, ×100) (E, hematoxylin-eosin). A and B, Nonossifying fibroma in distal shaft of radius with pathologic fracture shown in anteroposterior and lateral views of forearm. C and D, Fracture healing with normal callus formation several months later in patient shown in A and B. A, Bisected fibular segment shows two separate cortically oriented lesions, one containing abundant lipid and the other with extensive hemosiderin deposits. B, Whole-mount section of fibular shaft shows cortical orientation of nonossifying fibroma and circumscription by a narrow zone of sclerotic bone on medullary aspect. C, Brown, gelatinous tissue excised from proximal tibial metaphysis reflects high content of hemosiderin pigment. D, Segmental resection of fibula contains fibrous lesion with focal brown discoloration in medullary cavity. A and B, Low and intermediate power photomicrographs show bundles of spindle cells with rare interspersed multinucleated giant cells. C and D, Low and intermediate power photomicrographs showing spindle cell proliferations with interspersed multinucleated giant cells. A-D, Low and intermediate power photomicrographs showing fibrohisticytic proliferation with storiform pattern and rare interspersed multinucleated giant cells and histiocytes. A and B, Low and intermediate power photomicrographs showing a proliferation of histiocytic cells with occasional vacuolated foamy cytoplasm and prominent multinucleated giant cells. C and D, Low and intermediate power photomicrographs showing spindle cells growing in a storiform pattern showing scattered multinucleated giant cells. Note an angulated cytoplasmic outline of multinucleated giant cells and their somewhat pyknotic nuclei, a frequent feature of giant cells in nonossifying fibroma. Such lesions may raise suspicion of malignancy but the true cytologic atypia and atypical mitosis are absent. In addition, correlation with radiographic features showing typical radiographic presentation of nonossifying fibroma with the absence of imaging features indicating an aggressive growth pattern, confirm the benign nature of such lesions. In summary, the lesion has microscopic features that overlap with those of the fibrohistiocytic reactive lesions commonly seen in extraskeletal sites and with the reactive changes superimposed on various preexisting skeletal conditions. As a consequence, nonossifying fibroma can be confused with many other conditions if its microscopic appearance is evaluated without clinicoradiologic correlation. Cytogenetically, nonossifying fibromas have a near-diploid chromosomal complement. The distinction is easily made on clinical and radiologic grounds because giant cell tumor occurs almost exclusively in adult patients at the ends of long bones, not in the metaphyses.
One of 79 patients with this disorder was reported to have lytic bone lesions; however allergy forecast austin tx zyrtec 10 mg purchase with visa, histologic features were not reported. The most common feature of H syndrome is skin hyperpigmentation with hypertrichosis, followed by flexion contractures of the fingers and toes. One study of comparative genomic hybridization in patients with concurrent sinus histiocytosis with massive lymphadenopathy and Langerhans cell histiocytosis detected genomic gains and losses in the Langerhans cells but detected no abnormalties in the histiocytes in areas with features of sinus histiocytosis with massive lymphadenopathy. The first description of this lesion was in 1853 by King, who used the term chloroma to describe the green color of the gross mass due to production of myeloperoxidase. Not all patients present with leukemic involvement of the blood and bone marrow; however, the majority go on to develop frank acute myeloid leukemia with a lag time ranging from 1 month to 4 years. In the absence of a history of a myeloid neoplasm, the radiographic findings may overlap with a variety of reactive and neoplastic processes. A, Lateral radiograph of distal femur showing a destructive lytic lesion with moth-eaten pattern. B, Sagittal magnetic resonance image of the same case as shown in A with destructive lesion of the distal femur of intermediate signal intensity. C, Anteroposterior radiograph of the proximal femur showing a destructive lytic lesion involving head, neck, and intertrochanteric region. D, Radioisotopic scan showing diffuse involvement of the axial and proximal appendicular skeleton with a high signal intensity corresponding to the destructive lesion of the left proximal femur. The cellular composition ranges from a homogeneous population of blasts to a mixed population of blasts and more mature myeloid precursors, ranging from promyelocytes to neutrophils. Occasional cases may show more than one line of myeloid differentiation, erythroid differentiation, or megakaryoblastic features. Immunohistochemical Stains and Differential Diagnosis If the diagnosis is suspected, fresh tissue may be submitted for flow cytometric immunophenotyping, cytogenetic studies, and molecular studies. If fresh tissue is not reserved, immunohistochemical studies will confirm the diagnosis in most cases. The diagnosis is aided by history in cases of known preceding acute myeloid leukemia. The diagnosis of primary myeloid sarcoma, however, may be quite difficult, with misdiagnosis rates ranging from 25% to 100%. Flow cytometric immunophenotyping, including lymphoid, myeloid, and blast markers, is performed in suspected cases. Often, however, a diagnosis of myeloid sarcoma is not considered at the time of biopsy. A generous panel of immunohistochemical stains is needed to confirm the diagnosis and rule out other diagnostic possibilities. Rare cases of myeloid sarcoma may exhibit erythroid differentiation, variably positive for E-cadherin, glycophorin A, or hemoglobin A. Extramedullary hematopoiesis may be a diagnostic consideration; however, myeloid sarcoma will form a mass, whereas the cells of extramedullary hematopoiesis will be present within normal or slightly expanded spaces of the preexisting architecture of the involved organ. Genetic Findings and Pathogenesis the normal cell counterpart is a myeloid blast, usually with monocytic or granulocytic features, and occasionally with megakaryocytic or erythroid features. The reasons for blast homing to extramedullary tissues are uncertain; however, interactions between adhesion molecules have been suggested as a possible mechanism. B, Higher power photomicrograph of myeloid sarcoma in A, showing myeloblasts with scant cytoplasm, open nuclear chromatin, and small nucleoli (×400). C, Photomicrograph of myeloid sarcoma with granulocytic differentiation, showing myeloblasts intermixed with more mature granulocytes, including neutrophils and eosinophil precursors (×400). D, Ultrastructure of myeloblasts, which exhibits cytoplasmic granules consistent with granulocytic myeloid differentiation (×3500). A, Photomicrograph of myeloid sarcoma showing myeloblasts with prominent nucleoli and intermixed eosinophil myelocytes (×200). Leukemia 21:340-350, 2007; Schwyzer R, et al: Granulocytic sarcoma in children with acute myeloblastic leukemia and t(8:21). Chronic myelogenous leukemia may progress to blast crisis as a granulocytic sarcoma. In addition, inv(16) and various trisomies and monosomies have been reported in myeloid sarcoma. Skeletal involvement occurs in systemic mastocytosis and not in localized cutaneous mastocytosis. Definition Systemic mastocytosis involves one or more organs in addition to the skin. A diagnosis of systemic mastocytosis requires the presence of mast cell aggregates of greater than or equal to 15 cells within the bone marrow or other noncutaneous site (major criterion) and the presence of one additional minor criterion. Bone changes can be the primary or only manifestations of the disorder and may play a critical role in the initial diagnosis. The World Health Organization classification of mast cell diseases is provided in Table 12-12. Systemic mastocytosis is further subclassified as indolent 12 Hematopoietic Tumors 891 Chr 8 23. In addition to these general, nonspecific symptoms, most patients with indolent forms of mast cell disease have skin changes typical of urticaria pigmentosa. In addition, gastrointestinal symptoms such as abdominal pain, diarrhea, vomiting, and steatorrhea are present in approximately 20% of patients. Patients with indolent systemic mastocytosis have overall survival similar to age-matched controls, with a median survival of 198 months. The median survival times of aggressive systemic mastocytosis, mast cell leukemia, and systemic mastocytosis associated with a hematologic non-mast cell disorder are 41 months, 2 months, and 24 months, respectively.
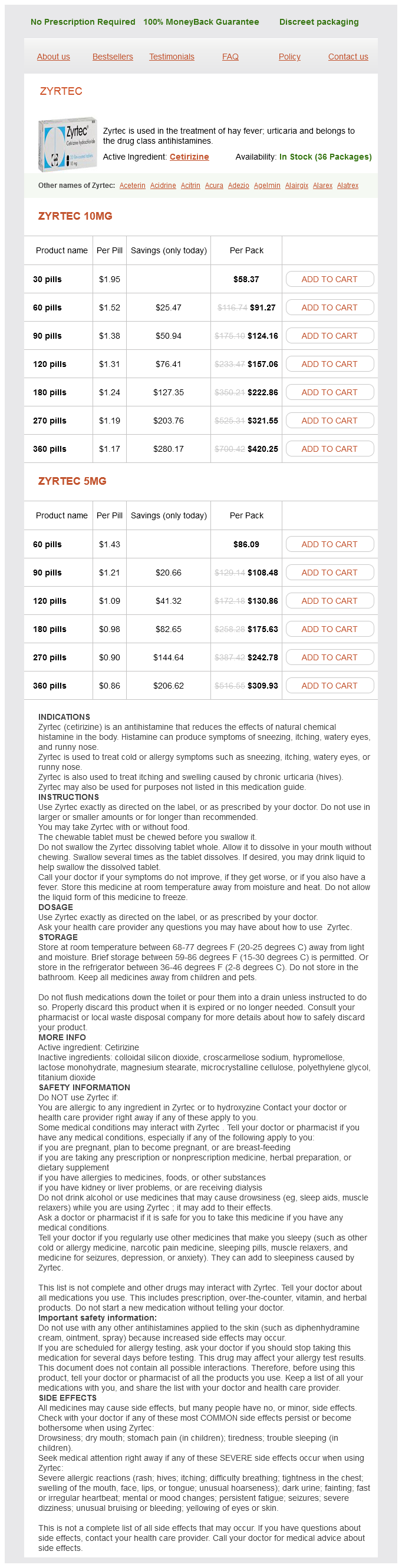
Zyrtec Dosage and Price
Zyrtec 10mg
- 30 pills - $58.37
- 60 pills - $91.27
- 90 pills - $124.16
- 120 pills - $157.06
- 180 pills - $222.86
- 270 pills - $321.55
- 360 pills - $420.25
Zyrtec 5mg
- 60 pills - $86.09
- 90 pills - $108.48
- 120 pills - $130.86
- 180 pills - $175.63
- 270 pills - $242.78
- 360 pills - $309.93
Although no fixed definition of these terms exists allergy symptoms wasp sting zyrtec 10 mg buy otc, the most common features of these various models of teamwork are described in this section. Specialist medical care Multidisciplinary Team the multidisciplinary team consists of a number of health professionals working individually within their specific professional boundaries, with some level of interaction or coordination. Often each team member assesses and manages the child separately, focusing of the aspect of the feeding difficulty traditionally managed by his or her profession. Team members usually share reports or contribute to a common report for the patient. Nutrition Swallowing, feeding Breastfeeding General development (motor and sensory skills) Cognition, learning, behavior Interdisciplinary Team training degrees and qualification required to work in this area. Some differences in facility practices also occur because of staffing levels and availability of various health professionals, as well as historical practices. Table 14-1 provides a summary of the various roles in a pediatric feeding team, and the most common health professionals who fulfill those roles. For additional information regarding the role of other health professionals in managing children with feeding difficulties, see their professional association websites (search pediatric feeding, dysphagia, and roles and responsibilities). The interdisciplinary team consists of a number of health professionals working together within their specific professional boundaries. Often team members assess and manage the child together, with each focusing of the aspect of the feeding difficulty traditionally managed by his or her profession. Transdisciplinary Team the transdisciplinary team consists of a number of health professionals working together across their specific professional boundaries. Usually, team members have worked together for some time and may have undertaken advanced training together. Team members are all aware of the aspects of the feeding difficulty traditionally managed by other members of the team. Often one team member is delegated to assess or manage the child, with input from and feedback to other members of the team as necessary. The primary team member for the child incorporates the goals of all the various team members into the assessment and management process. To assess swallow safety, the feeding therapist needs to observe and evaluate whether the child can protect the airway during feeds or mealtimes. This usually requires the feeding therapist to offer fluid or food trials and observe for any adverse clinical signs suggestive of laryngeal penetration or aspiration (Box 14-4). If adverse signs are observed to occur during oral preparation or swallowing, they may indicate that material is entering the airway on descent through the pharynx. If adverse clinical signs are observed during pauses in feeding or after feeds, they may indicate that material (reflux) is ascending into the pharynx or larynx from the gut. Imaging studies (as detailed later in this chapter) are used to confirm or allay clinical suspicions of aspiration and guide management practices. For young infants who are breastfed or bottle fed, the coordination of suckling, swallowing, and breathing is assessed by observing and listening to the ratio of sucks to swallows, as well as the timing and adequacy of respiratory efforts throughout the feed. The normal rhythmic suckling pattern during breastfeeding or bottle feeding consists of a series of bursts and pauses. Normally, full recovery in all respiratory parameters occurs within the suckling pauses. Even if the infant does not show clinical signs of aspiration during feeding, other adverse physiologic events during feeding (Box 14-5) can indicate a potential to affect feeding. The following webpages contain specific examples of combined case history and clinical assessment forms for infants and for older children. To start, a brief assessment should be performed of oral anatomy, oral reflexes, oral sensory processing, and oral motor control (see Box 14-6). Then the feeding therapist should try to observe how the child feeds at a typical meal. In addition, clinicians should have a range of developmentally appropriate feeding equipment. Note type of response, degree of response, and any change in response with repeated exposure. It should be noted that, although there are a number of formal feeding assessment tools available, most were developed to assist in classifying the feeding skills of children with cerebral palsy and other neurodevelopmental disorders. In clinical practice, many clinicians do not routinely use formal assessment tools when assessing children with feeding difficulties, but rather rely on informal checklists based on normal feeding development to guide their evaluation. It often helps to videotape the session to allow later playback for further analysis and parent training. In cases in which primary aspiration or respiratory compromise during feeding is suspected or in which the child is struggling to consume enough fluid or food, a number of different feeding therapy techniques and compensations may be trialed by the feeding therapist as part of the assessment process. Altering positioning or seating equipment; altering pace of delivery (pacing); trialing swallowing maneuvers. During this time, the role of the feeding therapist is to assess whether it is possible to introduce activities that can promote normal oral experiences. However, the therapist must resist pressure to clear a child for full oral feeding and discharge if the child or the family is not fully competent in the tasks that will be required for the child to manage full oral feeds at home. Medical Stability the feeding therapist needs to have a general awareness and understanding of the variety of health issues that may present in children with feeding difficulties and be sensitive in their interactions with patients, their family members, and other health professionals. In medically complex children, there are times when the greatest focus for medical staff and the family needs to be managing acute health complications. In contrast, there are times when care can become focused on supporting developmentally appropriate activities, such as feeding. In between these events, there are often times when feeding assessment and intervention can start to be introduced, provided they do not interfere with other essential health care activities (this is something that needs to be discussed and agreed on by medical and therapy staff). Some medically complex children undergo multiple cycles of acute illness and medical treatment, and frequent monitoring of feeding skills is required to track any progress or regression in these cycles.