General Information about Zyloprim
Benefits of Zyloprim for Cancer Chemotherapy
As with any medication, there are dangers related to taking Zyloprim. Common unwanted facet effects may embrace pores and skin rash, nausea, vomiting, diarrhea, and headache. In uncommon instances, extra serious side effects, such as liver or kidney injury, may happen. It is essential to report any unusual symptoms to a healthcare provider instantly.
Some types of cancer treatments, similar to chemotherapy, can cause a rise in uric acid levels in the body. This can lead to a condition known as tumor lysis syndrome, which might damage the kidneys and different organs. Zyloprim is commonly prescribed along with chemotherapy to stop or deal with excessive uric acid ranges and scale back the chance of problems.
Zyloprim, also known as allopurinol, is a drugs primarily used to treat gout, a type of arthritis that occurs when there's an excessive buildup of uric acid within the physique. It is also prescribed to deal with high levels of uric acid in the blood or urine caused by certain types of most cancers chemotherapy. Let's take a closer look at what Zyloprim is, the means it works, and its potential benefits and risks.
Gout is a painful and persistent situation that affects millions of people worldwide. It is characterized by episodes of intense joint ache, normally within the huge toe, brought on by the buildup of uric acid crystals within the joints. Gout attacks could be triggered by consuming meals high in purines, similar to pink meat, seafood, and alcohol. By decreasing uric acid manufacturing, Zyloprim can help prevent future gout attacks and reduce total ache and inflammation related to the condition.
Zyloprim is a widely prescribed medication for the therapy of gout and excessive uric acid levels within the body. It works by decreasing uric acid manufacturing and can present important reduction for individuals affected by gout attacks. It can additionally be commonly used in cancer patients undergoing chemotherapy to forestall issues from high uric acid levels. However, as with every medicine, it's essential to comply with the prescribed dosage and report any side effects to healthcare professionals immediately to ensure its secure and effective use.
Furthermore, Zyloprim must be used with warning in people with a history of kidney or liver disease, in addition to those taking certain drugs, corresponding to diuretics, blood thinners, and diabetes medicine.
Risks of Zyloprim
In Conclusion
Zyloprim is out there in tablet type and is often taken as soon as a day, or as directed by a healthcare skilled. The beneficial starting dose for most individuals is 100 mg per day, which may be adjusted primarily based on individual response and tolerability. It is important to observe the prescribed dosage and take Zyloprim with meals and loads of water to minimize the chance of developing unwanted side effects.
Zyloprim is a prescription medication that belongs to a category of drugs called xanthine oxidase inhibitors. It works by decreasing the production of uric acid within the physique, thereby stopping the formation of urate crystals within the joints that trigger the attribute ache and inflammation of gout. It additionally helps to dissolve existing urate crystals, reducing the danger of future gout attacks.
Benefits of Zyloprim for Gout
What is Zyloprim?
Dosage and Administration
Median visual acuity symptoms nasal polyps purchase zyloprim 100 mg without prescription, visual acuity improvement of 10 or more letters, median retinal thickness and need for photocoagulation were all better after 36 weeks of treatment with 0. Results of ongoing clinical trials will be necessary before enough is known about the efficacy and side effects of these new agents to assess their impact on the clinical care of diabetic eye disease. Vision can improve, although this improvement does not always occur, and the effect generally wears off necessitating repetitive injections. Eye Examination Schedule Type of Diabetes Mellitus Type 1 Diabetes Mellitus Type 2 Diabetes Mellitus During pregnancy Recommendation Time of First Examination 5 yr after onset or during puberty At time of diagnosis Prior to pregnancy for counseling Early in first trimester Each trimester or more frequently as indicated *Abnormal findings dictate more frequent follow-up examinations. Mean visual acuity was better in the ruboxistaurintreated patients from 12 months onward. In ruboxistaurintreated patients, visual improvement of 15 or more letters was twice as frequent (4. Ruboxistaurin treatment also reduced progression of macular edema to within 100 mm from the center of the macula and the need for initial laser treatment for macular edema was 26% less frequent in eyes of ruboxistaurin-treated patients. Ruboxistaurin therapy was very well tolerated and has had an excellent safety profile to date. Requirements for additional studies for full regulatory approval are currently under discussion. Such studies hold promise for eventually even more effective, more specific and safer therapies than are currently available. However, several years of further investigation will be required before any potential clinical impact is known. Ongoing research is addressing mechanisms contributing to altered retinal blood flow and retinal vascular complications in diabetes. A wide array of other targets are evolving from the studies of angiogenic agents and their mechanism of action over the past decade based on work initiated by Michelson nearly six decades ago. Proper care results in substantial reduction of personal suffering and substantial cost savings. Ocular telemedicine is one approach that has the potential to extend high quality diabetes eye care to patients who face socioeconomic, geographic, or other challenges to care. While some programs have demonstrated a high degree of reliability in identifying level of diabetic retinopathy compared to clinical examination and standard retinal photography, it is important for both patients and health care providers to recognize strengths and limitations of ocular telemedicine programs. Strict guidelines have been established for the ocular care of people with diabetes (Tables 133. All diabetic patients should be informed of the possibility of the development of retinopathy with or without symptoms and the associated threat of visual loss. The patient must understand that the risks of diabetes complications in the eye and elsewhere in the body may be reduced by diligent personalized health care and routine follow-up examinations, and that early efforts despite lack of symptoms can yield long term benefits that are lost if care is initiated late. Patients should be informed of the strong relationship between diabetes control and the subsequent development of ocular and other medical complications. Patients with permanent visual impairment, including legal or total blindness, should be informed of the availability of visual, vocational, and psychosocial rehabilitation programs. Diabetic women contemplating pregnancy should have a complete eye examination prior to conception if possible. Since pregnancy may dramatically exacerbate existing retinopathy and may be associated with hypertension, diabetic women should have their eyes examined early in the first trimester of pregnancy and generally at least each trimester thereafter and again 12 months post partum. Visual acuity may be excellent, and the patient may be completely unaware of even advanced retinopathy. Preservation of vision can be maximized by early initiation of a careful eye care program which includes patient education, close follow-up, and efficient communication between the entire team of health care providers. Optimal control of systemic factors such as blood glucose, blood pressure, and lipids is also critical. All members of the health team share the responsibility of assuring such care is offered to the patient. Faced with the current inability to prevent or cure diabetic retinopathy, the eye care for patients with diabetes must primarily focus on patient access, early detection, accurate retinopathy assessment, careful medical and ophthalmic followup, timely laser photocoagulation and appropriate use of novel therapies. With this approach, and the continuum of connected diabetes eye and medical care evolving from advances in information technology and telemedicine, our twenty-first century mission of preserving vision in patients with diabetes will become increasingly successful. Diabetic Retinopathy Study Report Number 1: Preliminary report on effects of photocoagulation therapy. Diabetic Retinopathy Study Report Number 2: Photocoagulation of proliferative diabetic retinopathy. Diabetic Retinopathy Study Report Number 3: Four risk factors for severe visual loss in diabetic retinopathy. Diabetic Retinopathy Study Report Number 5: Photocoagulation treatment of proliferative diabetic retinopathy. Diabetic Retinopathy Study Report Number 6: Design, methods, and baseline results. Diabetic Retinopathy Study Report Number 7: A modification of the Airlie House Classification of Diabetic Retinopathy. Diabetic Retinopathy Study Report Number 8: Photocoagulation treatment of proliferative diabetic retinopathy. Diabetic Retinopathy Study Report Number 9: Assessing possible late treatment effects in stopping clinical trials early: a case study. Diabetic Retinopathy Study Report Number 10: Factors influencing the development of visual loss in advanced diabetic retinopathy. Diabetic Retinopathy Study Report Number 11: Intraocular pressure following panretinal photocoagulation for diabetic retinopathy.
The trailing haptic rotates 180° during unfolding and is not advanced through the corneal wound until after the lens is unfolded in the eye treatment 3rd degree av block zyloprim 300 mg order mastercard. From Ahmet E: Knotless scleral fixation for implanting a posterior chamber intraocular lens. Prepare the eye in the usual fashion, including the removal of vitreous from the anterior chamber, iris plane, and anterior vitreous cavity. Pass the other needle of the double-armed suture on a similar path, but exit the eye ~1 mm lateral to the first exit site. Rotate the needles backward through the pupil and behind the iris so that they exit through the superior ciliary sulcus. After closing the corneoscleral limbal wound in the usual fashion, close the scleral flaps at their corners with an 80 or 9. However, significant improvements in lens design and materials as well as changes in surgical technique have made pars plana fixation an acceptable surgical approach. The pars plana is relatively avascular and lies anterior to the retina; thus, one can avoid hemorrhagic complications and retinal detachments by making incisions through the sclera and choroid into the vitreous at the level of the pars plana. Pass a double-armed suture on a long needle through the incision, the pupil, under the iris, through the ciliary sulcus, and out through the sclera 11. The other needle of the double-armed suture is passed in a similar manner, exiting 1 mm lateral to the first exit site. The diameter of the lens must be increased to ~17 mm, and the diameter of the biconvex optic to 7 mm. If the lens is in this position, the A constant should be in the same range as for in-the-bag placement. Alternative methods of burying the knots include covering them with scleral flaps or a scleral groove. Therefore, to enter the pars plana safely, the sclera should be entered 35 mm behind the limbus, keeping the needle path parallel to the iris plane. Alternatively, they could be placed in a limbus-parallel position; both at the same distance from the limbus, but 2 mm apart. In either case, it is important to place these double sutures exactly opposite each other relative to the center of the cornea to avoid lens tilt. Teichmann notes that for greater stability, the two sutures attached to the haptic can be secured with two eyelets inferotemporally, at a distance of ~3 or 3. The haptic should then be secured with the single eyelet and one suture by creating iris-parallel stitches inserted at 3 and 3. Suture ends are tied and cut at the paracentesis and the iris pushed back into place. The main incision is closed after removal of viscoelastic material Recent work by Benevento and colleagues82 have suggested the added step of a safety net suture that is temporarily fixed in the posterior chamber to act as a surrogate capsule. The addition of this one step prior to lens insertion would facilitate the remainder of the procedure while potentially rendering it safer. Anterior vitrectomy if necessary for any vitreous remnant in the anterior chamber 3. Haptics inserted into ciliary sulcus and optic capture by pupil is induced (injection of intracameral myotic will facilitate this step). The haptics will be outlined against the posterior surface of the iris Optic Suture Fixation to Iris this technique involves fixing the optic rather than the haptic to the iris. The sutures are hooked and tied through a paracentesis adjacent to the needle exit sites after the needles are cut off 9. The two curved needles are passed through superior iris adjacent to the incision and tied to anterior iris surface 10. Intraocular hemorrhage is another possible complication that can be reduced by minimizing iris manipulation and paying close attention to needle placement during suturing. A range between 9% and 36% of patients with scleral-sutured lenses and penetrating keratoplasty experience this complication. The two important factors affecting the likelihood of iris chafe are suture location and tightness of the suture. The central iris is most mobile, therefore, central suture placement will result in excessive inflammation, but the fixing of central iris at sites of suture fixation will result in an irregular pupil with peaking at those sites. Excessively tight sutures or excessively large bites of Glaucoma Glaucoma is another common complication of scleral-sutured posterior chamber lens implants. Glaucoma after an implantation occurs even more frequently when the operation is performed at the same time as penetrating keratoplasty. Holland and colleagues suspected that scleral-sutured lenses were associated with glaucoma. Lens Decentration Lens tilt or decentration is found in 510% of patients after scleral-sutured posterior chamber lens implantation. The patients must be carefully informed about the possible risk of decreased vision and of complications during the procedure. The variety of methods of intraocular implantation allows the surgeon to individualize the approach to best fit each case. Choroidal Detachment Transscleral sutures are thought to increase the risk of choroidal detachment. Bellucci R, Pucci V, Morselli S, Bonomi L: Secondary implantation of angle-supported anterior chamber and scleral-fixated posterior chamber intraocular lenses. Hayashi K, Hayashi H, Nakao F, Hayashi F: Corneal endothelial cell loss in phacoemulsification surgery with silicone intraocular lens implantation. Hannush S: Sutured posterior chamber intraocular lenses: indications and procedures. Miyake K, Asakura M, Kobayashi H: Effect of intraocular lens fixation on the blood-aqueous barrier.
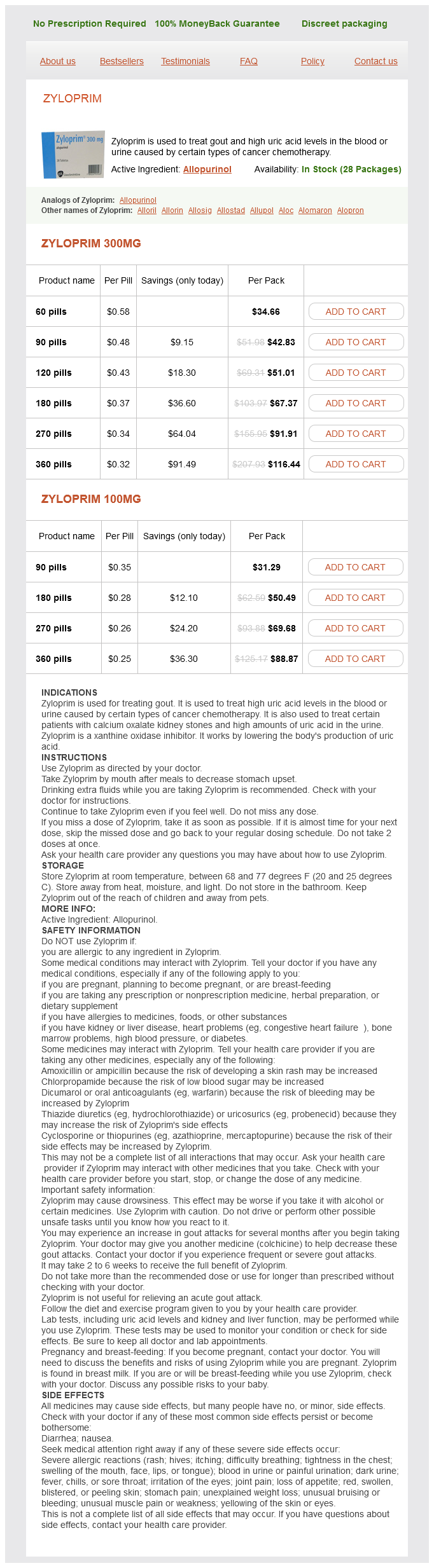
Zyloprim Dosage and Price
Zyloprim 300mg
- 60 pills - $34.66
- 90 pills - $42.83
- 120 pills - $51.01
- 180 pills - $67.37
- 270 pills - $91.91
- 360 pills - $116.44
Zyloprim 100mg
- 90 pills - $31.29
- 180 pills - $50.49
- 270 pills - $69.68
- 360 pills - $88.87
Zhang Y medications used for migraines purchase generic zyloprim on line, Stone J: Role of astrocytes in the control of developing retinal vessels. Junctional complexes of the retinal vessels and their role in the permeability of the blood-retinal barrier. Carella E, Carella G: Microangioarchitecture of the choroidal circulation using latex casts. Spitznas M, Reale E: Fracture faces of fenestrations and junctions of endothelial cells in human choroidal vessels. Sugita A, Hamasaki M, Higashi R: Regional difference in fenestration of choroidal capillaries in Japanese monkey eye. Ehinger B: Adrenergic nerves to the eye and to related structures in man and cynomolgus monkey. Nilsson: Nitric oxide as a mediator of parasympathetic vasodilation in ocular and extraocular tissues in the rabbit. Büngard M: the three-dimensional organisation of tight jonctions in a capillary endothelium revealed by serial-section microscopy. Neuhaus J, Risau W, Wolburg H: Induction of blood-brain barrier characteristics in bovine brain endothelial cells by rat astroglial cells in transfilter coculture. Tornquist P, Alm A, Bill A: Studies on ocular blood flow and retinal capillary permeability to sodium in pigs. Alm A, Tornquist P: the uptake index method applied to studies on the bloodretinal barrier. Tornquist P, Alm A: Carrier-mediated transport of amino acids through the blood-retinal and the blood-brain barriers. Bill A: Calorimetric procedures for the study of the blood flow through the ciliary region and the choroid in rabbits. Effects of high intraocular pressure and of increased arterial carbon dioxide tension on uveal and retinal blood flow in cats. A study with radioactively labelled microspheres including flow determinations in brain and some other tissues. Alm A, Bill A: Ocular and optic nerve blood flow at normal and increased intraocular pressures in monkeys (Macaca irus): a study with radioactively labelled microspheres including flow determinations in brain and some other tissues. Alm A, Bill A: Blood flow and oxygen extraction in the cat uvea at normal and high intraocular pressures. Tornquist P, Alm A: Retinal and choroidal contribution to retinal metabolism in vivo. Tsacopoulos M, Poitry S, Borsellino A: Diffusion and consumption of oxygen in the superfused retina of the drone (Apis mellifera) in darkness. Pournaras C, Tsacopoulos M, Chapuis P: Studies on the role of prostaglandins in the regulation of retinal blood flow. Tsacopoulos M, Levy S: Intraretinal acidbase studies using pH glass microelectrodes: effect of respiratory and metabolic acidosis and alkalosis on innerretinal pH. Alm A: Effects of norepinephrine, angiotensin, dihydroergotamine, papaverine, isoproterenol, histamine, nicotinic acid, and xanthinol nicotinate on retinal oxygen tension in cats. Granstam E, Wang, Bill A: Ocular effects of endothelin-1 in the cat 1992; 11:325332. Eddahibi S, Monirul M, et al: Dilator effect of endothelins in pulmonary circulation: damages associated with chronic hypoxia. Garhofer G, Resch H, et al: Effect of intravenous administration of sodiumlactate on retinal blood flow in healthy subjects. Jeppesen P, Aalkjoer C, Bek T: Bradykinin relaxation in small porcine retinal arterioles. Delaey C, Van de Voorde J: Pressureinduced myogenic responses in isolated bovine retinal arteries. Bill A, Aspects of oxygen and glucose consumption in the retina: effects of high intraocular pressure and light. Iadecola C: Regulation of the cerebral microcirculation during neural activity: is nitric oxide the missing link Kondo M, Wang L, Bill A: the role of nitric oxide in hyperaemic response to flicker in the retina and optic nerve in cats. Deussen A, Sonntag M, Vogel R: L-arginine-derived nitric oxide: a major determinant of uveal blood flow. Moncada S: Pharmacology and endogenous roles of prostaglandins endoperoxides, thromboxane A2 and Prostacyclin 1979; 30:293331. Nagaoka T, Mori F, et al: the effect of nitric oxide on retinal blood flow during hypoxia in cats. Alm A: the effect of sympathetic stimulation on blood flow through the uvea, retina and optic nerve in monkeys (Macaca irus). Alm A, Bill A: the effect of stimulation of the cervical sympathetic chain on retinal oxygen tension and on uveal, retinal and cerebral blood flow in cats. Bill A, Linder M, Linder J: the protective role of ocular sympathetic vasomotor nerves in acute arterial hypertension. Nilsson Bill A: Characteristicss of uvea vasodilation produced by facial nerve stimulation in monkeys, cats, and rabbits. Schmetterer L, et al: the effect of systemic nitric oxide-synthase inhibition on ocular fundus pulsations in man. Tsacopoulos M: Role of metabolic factors in the regulation of retinal blood minute volume. Bietti G: Effects of experimentally decreased or increased oxygen supply in some ophthalmic diseases; practical value for diagnosis, prognosis, and treatment.