General Information about Voltaren
In abstract, Voltaren is a highly efficient NSAID that may present reduction from ache and inflammation related to arthritis and acute accidents. Its various types and decrease threat of gastrointestinal unwanted facet effects make it a preferred choice for a lot of sufferers. However, it could be very important use Voltaren as directed and to seek the guidance of with a physician earlier than beginning treatment. With applicable use and monitoring, Voltaren might help many patients to better handle their situations and improve their quality of life.
One of the main advantages of Voltaren over other NSAIDs is that it has a comparatively low risk of inflicting gastrointestinal unwanted effects, similar to stomach ulcers and bleeding, which are common with different medicines in this class. However, like all medications, Voltaren should still cause some mild side effects in some sufferers, corresponding to nausea, dizziness, and headache. It is essential to discuss potential side effects with a doctor earlier than beginning Voltaren and to report any antagonistic reactions to the medication.
Voltaren is on the market by prescription solely, which implies that patients might need to consult with a health care provider before beginning therapy. This is to ensure that the medication is used safely and effectively, and to monitor for any potential drug interactions or other well being considerations. Patients also needs to inform their physician of any current medical circumstances or medications they're taking, as this will have an effect on the appropriateness of Voltaren for their particular person scenario.
One of the first makes use of of Voltaren is within the remedy of arthritis. Arthritis is a chronic condition characterised by inflammation of the joints, which may cause important ache and discomfort for individuals who suffer from it. Voltaren is ready to scale back inflammation by blocking the production of sure enzymes which are responsible for inflicting irritation. By doing so, it helps to alleviate ache and swelling in the joints, making it easier for patients to hold out their every day activities.
In addition to arthritis, Voltaren can be commonly used to treat acute injuries, such as sprains, strains, and bruises. These kinds of injuries can be attributable to sports activities, accidents, or different physical actions and can lead to significant ache and discomfort. Voltaren works by blocking the manufacturing of prostaglandins, that are hormones that promote inflammation. By reducing irritation at the web site of the injury, it could help to ease ache and improve mobility, allowing patients to recover more shortly.
Voltaren, also known by its generic name diclofenac, is a nonsteroidal anti-inflammatory drug (NSAID) that is generally used to relieve irritation and pain in patients with conditions such as arthritis or acute injuries. It was first launched by the Swiss pharmaceutical firm Novartis in 1973 and has since turn out to be a widely prescribed treatment because of its effectiveness in decreasing ache and irritation.
Voltaren is out there in a variety of varieties, including tablets, capsules, and topical gels or creams. The tablets and capsules are usually taken by mouth, whereas the topical gels or lotions are applied on to the affected space. This permits for flexibility in treatment choices, so patients can choose probably the most suitable form of Voltaren based mostly on their individual needs and preferences.
For example rheumatoid arthritis kill you order voltaren 50 mg overnight delivery, more than 50% of lymphocytes in the small bowel mucosa of mice and chickens, called intraepithelial lymphocytes, are T cells. A working hypothesis for the specificity of T cells is that they may recognize antigens that are frequently encountered at epithelial boundaries between the host and the external environment. A number of biologic activities have been ascribed to T cells, including secretion of cytokines and killing of infected cells, but the function of these cells and their contribution to normal immune responses remain poorly understood. It has been postulated that this subset of T cells may initiate immune responses to microbes at epithelia, before the recruitment and activation of antigenspecific T cells. It is not known if this is the case in other inflammatory disorders or what the cells are recognizing or how much they are contributing to the development of the disease. However, the roles of these cells in protective immunity or disease in humans are unclear. Given their abundance in the liver, it is possible that they represent a second important barrier to gut flora that have breached the intestinal epithelial barrier and entered the blood, since blood draining the gut first enters the liver through the portal circulation. Each subset produces cytokines that increase its own development and inhibit the development of the other subsets, thus leading to increasing polarization of the response. Activated macrophages kill phagocytosed microbes ingested into phagolysosomes by the actions of reactive oxygen and nitrogen species and enzymes (called classical macrophage activation). Th17 cells may also be important in mediating tissue damage in autoimmune diseases. These cells produce cytokines and may contribute to host defense and inflammatory diseases. It is mediated by T lymphocytes and can be transferred from immunized to naive individuals by T cells and not by antibodies. Mechanisms underlying helper T-cell plasticity: implications for immune-mediated disease. Th17 cell pathway in human immunity: lessons from genetics and therapeutic interventions. A brief history of T(H)17, the first major revision in the T(H)1/T(H)2 hypothesis of T cell-mediated tissue damage. Interleukin-4- and interleukin13-mediated alternatively activated macrophages: roles in homeostasis and disease. The viruses cannot be destroyed if the infected cells are not phagocytes with intrinsic lysosomal microbicidal mechanisms. Even in phagocytes, if the viruses are in the cytosol, they are inaccessible to these killing mechanisms. In these situations, the only way to eradicate the established infection is to kill the infected cell, crippling the ability of the virus to survive and replicate. The same mechanism is used to eliminate phagocytes containing ingested bacteria that escape from phagosomes into the cytosol and are no longer susceptible to the killing activity of the phagocytes. Two transcription factors that are required for this program of new gene expression are T-bet (which we discussed in relationship to Th1 differentiation in Chapter 10) and eomesodermin, which is structurally related to T-bet. As we discussed in Chapter 6, the immune system deals with this problem by the process of cross-presentation. The requirement for helper cells varies according to the type of antigen exposure. These cytokines may be produced by different dendritic cell populations during the innate immune response to viral and some bacterial infections. The term exhaustion has been used to imply that the effector response starts but is shut down (unlike in tolerance, when lymphocytes fail to develop into effector cells). This phenomenon of exhaustion was first described in a chronic viral infection in mice and was implicated in the prolonged persistence of the virus. The cells also express transcription factors associated with effector and memory cells, including T-bet and eomesodermin, but they remain functionally inactive. The phenomenon of T cell exhaustion may have evolved to attenuate the tissue-damaging consequences of chronic infection. The granules also contain a sulfated proteoglycan, serglycin, which serves to hold granzymes and perforin in the granules in an inactive state. The main function of perforin is to facilitate delivery of the granzymes into the cytosol of the target cell. Perforin can polymerize and form aqueous pores in the target cell membrane, but these pores may not be of sufficient size to allow granzymes to enter. Perforin may then act on the endosomal membrane to facilitate the release of the granzymes into the target cell cytosol. Once in the cytosol, the granzymes cleave various substrates, including caspases, and initiate apoptotic death of the cell. For example, granzyme B cleaves and activates caspase-3 as well as the Bcl-2 family member Bid, which triggers the mitochondrial pathway of apoptosis. The granzymes are delivered into the cytoplasm of the target cells by a perforin-dependent mechanism, and they induce apoptosis. This interaction also results in activation of caspases and apoptosis of Fas-expressing targets. This is particularly important in two types of situations when cells cannot destroy microbes that infect them. First, most viruses live and replicate in cells that lack the phagosome/lysosome machinery for destroying microbes (such as hepatitis viruses in liver cells). Second, even in phagocytes, some microbes escape from vesicles and live in the cytosol, where microbicidal mechanisms are ineffective because these mechanisms are largely restricted to vesicles (to protect the host cells from damage). Bacteria such as Mycobacterium tuberculosis and Listeria monocytogenes are examples of microbes that escape from vesicles and enter the cytosol of infected cells. These viruses are not highly cytopathic, but the host senses and reacts against the infectious microbe and is not able to distinguish microbes that are intrinsically harmful or relatively harmless (see Chapter 19).
The lateral aortic or lumbar lymph nodes (para-aortic nodes) receive lymphatics from the body wall arthritis reversed buy voltaren online, the kidneys, the suprarenal glands, and the testes or ovaries. The pre-aortic nodes are organized around the three anterior branches of the abdominal aorta that supply the abdominal part of the gastrointestinal tract, as well as the spleen, pancreas, gallbladder, and liver. They are divided into celiac, superior mesenteric, and inferior mesenteric nodes, and receive lymph from the organs supplied by the similarly named arteries. Finally, the lateral aortic or lumbar nodes form the right and left lumbar trunks, whereas the pre-aortic nodes form the intestinal trunk. These trunks come together and form a con uence that, at times, appears as a saccular dilation (the cisterna chyli). Lymphatic vessel Right jugular trunk Left jugular trunk Right subclavian trunk Left subclavian trunk Right bronchomediastinal trunk Left bronchomediastinal trunk Area drained Right side of head and neck Left side of head and neck Right upper limb, super cial regions of thoracic and upper abdominal wall Left upper limb, super cial regions of thoracic and upper abdominal wall Right lung and bronchi, mediastinal structures, thoracic wall Left lung and bronchi, mediastinal structures, thoracic wall Lower limbs, abdominal walls and viscera, pelvic walls and viscera, thoracic wall 200 Thoracic duct Regional anatomy · Posterior abdominal region 4 Clinical app Retroperitoneal lymph node surgery From a clinical perspective, retroperitoneal lymph nodes are arranged in two groups. The pre-aortic lymph node group drains lymph from the embryological midline structures, such as the liver, bowel, and pancreas. The para-aortic lymph node group (the lateral aortic or lumbar nodes), on either side of the aorta, drain lymph from bilateral structures, such as the kidneys and adrenal glands. Organs embryologically derived from the posterior abdominal wall also drain lymph to these nodes. These organs include the ovaries and the testes (importantly, the testes do not drain lymph to the inguinal regions). Massively enlarged lymph nodes are a feature of lymphoma, and smaller lymph node enlargement is observed in the presence of infection and metastatic malignant spread of disease. The surgical approach to retroperitoneal lymph node resection involves a lateral paramedian incision in the midclavicular line. The three layers of the anterolateral abdominal wall (external oblique, internal oblique, and transversus abdominis) are opened and the transversalis fascia is divided. Instead of entering the parietal peritoneum, which is standard procedure for most intra-abdominal surgical operations, the surgeon gently pushes the parietal peritoneum toward the midline, which moves the intra-abdominal contents and allows a clear view of the retroperitoneal structures. On the left, the para-aortic lymph node group (lateral aortic or lumbar nodes) are easily demonstrated with a clear view of the abdominal aorta and kidney. On the right the inferior vena cava is demonstrated, which has to be retracted to access to the right para-aortic lymph node chain (lateral aortic or lumbar nodes). The procedure of the retroperitoneal lymph node dissection is extremely well tolerated and lacks the problems of entering the peritoneal cavity. Unfortunately, the complication of a vertical incision in the midclavicular line is to divide the segmental nerve supply to the rectus abdominis muscle. This produces muscle atrophy and asymmetrical proportions to the anterior abdominal wall. Sympathetic trunks and splanchnic nerves the sympathetic trunks pass through the posterior abdominal region anterolateral to the lumbar vertebral bodies, before continuing across the sacral promontory and into the pelvic cavity. These represent collections of neuronal cell bodies-primarily postganglionic neuronal cell bodies-which are located outside the central nervous system. There are usually four ganglia along the sympathetic trunks in the posterior abdominal (lumbar) region. Also associated with the sympathetic trunks in the posterior abdominal region are the lumbar splanchnic nerves. These components of the nervous system pass from the sympathetic trunks to the plexus of nerves and ganglia associated with the abdominal aorta. Usually two to four lumbar splanchnic nerves carry preganglionic sympathetic bers and visceral afferent bers. Abdominal prevertebral plexus and ganglia the abdominal prevertebral plexus is a network of nerve bers surrounding the abdominal aorta. It extends from the aortic hiatus of the diaphragm to the bifurcation of the aorta into the right and left common iliac arteries. Continuing inferiorly, the plexus of nerve bers extending from just below the superior mesenteric artery to the aortic bifurcation is the abdominal aortic plexus. At the bifurcation of the abdominal aorta, the abdominal prevertebral plexus continues inferiorly as the superior hypogastric plexus. Throughout its length, the abdominal prevertebral plexus is a conduit for: preganglionic sympathetic and visceral afferent bers from the thoracic and lumbar splanchnic nerves. Associated with the abdominal prevertebral plexus are clumps of nervous tissue (the prevertebral ganglia), which are collections of postganglionic sympathetic neuronal cell bodies in recognizable aggregations along the abdominal prevertebral plexus; they are usually named after the nearest branch of the abdominal aorta. They are therefore referred to as celiac, superior mesenteric, aorticorenal, and inferior mesenteric ganglia. These structures, along with the abdominal prevertebral plexus, play a critical role in the innervation of the abdominal viscera. Nervous system in the posterior abdominal region Several important components of the nervous system are in the posterior abdominal region. These include the sympathetic trunks and associated splanchnic nerves, the plexus of nerves and ganglia associated with the abdominal aorta, and the lumbar plexus of nerves. Pos terior root Anterior root Es ophagus Vagus nerve Aorta Celiac ganglion Preganglionic paras ympathetic Enteric neuron Gray ramus communicans Pos terior and anterior rami White ramus communicans Sympathetic ganglion and trunk Greater s planchnic nerve Vis ceral afferent Vis ceral afferent Preganglionic s ympathetic Pos tganglionic s ympathetic 202. Lumbar plexus the lumbar plexus is formed by the anterior rami of nerves L1 to L3, and most of the anterior ramus of L4 (Table 4. Branches of the lumbar plexus include the iliohypogastric, ilio-inguinal, genitofemoral, lateral cutaneous nerve of thigh (lateral femoral cutaneous), femoral, and obturator nerves. The lumbar plexus forms in the substance of the psoas major muscle anterior to its attachment to the transverse processes of the lumbar vertebrae. Therefore, relative to the psoas major muscle, the various branches emerge either: anterior-genitofemoral nerve, medial-obturator nerve, or lateral-iliohypogastric, ilio-inguinal, and femoral nerves, and the lateral cutaneous nerve of the thigh. T12 L1 Iliohypogas tric nerve Ilio-inguinal nerve Genitofemoral nerve L3 Lateral cutaneous nerve of thigh L4 To iliacus mus cle Femoral nerve Obturator nerve To lumbos acral trunk L2 Iliohypogastric and ilio-inguinal nerves (L1) the iliohypogastric and ilio-inguinal nerves arise as a single trunk from the anterior ramus of nerve L1. Either before or soon after emerging from the lateral border of the psoas major muscle, this single trunk divides into the iliohypogastric and the ilio-inguinal nerves.
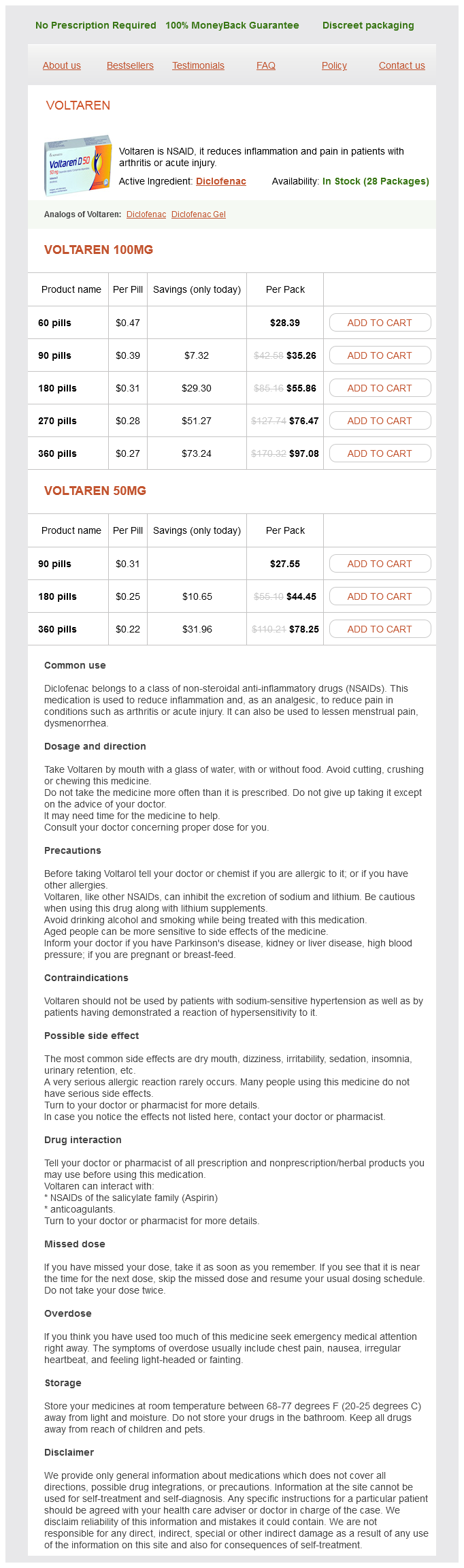
Voltaren Dosage and Price
Voltaren 100mg
- 60 pills - $28.39
- 90 pills - $35.26
- 180 pills - $55.86
- 270 pills - $76.47
- 360 pills - $97.08
Voltaren 50mg
- 90 pills - $27.55
- 180 pills - $44.45
- 360 pills - $78.25
The lateral femoral cutaneous nerve is most often affected and presents with numbness over the lateral thigh arthritis in knee from running 50 mg voltaren order with amex. Making a Local Anesthetic Toxicity Kit and posting instructions for its use are encouraged. Know the expected response, onset, duration, and limitations of "test dose" in identifying intravascular injection. Therefore it is recommended to avoid high doses of epinephrine and use smaller doses. Propofol is a cardiovascular depressant with lipid content too low to provide benefit. Its use is discouraged when there is a risk of progression to cardiovascular collapse. Nulliparity, fetal macrosomia, prolonged second stage of labor, and prolonged duration of hip hyperflexion are associated with increased rates of injury. Regional labor analgesia was not associated with nerve injury in a large prospective study (22). Occasionally, root injuries or radiculopathy may present postpartum due to exacerbation of underlying pathologies such as disk herniation. During neuraxial block, a needle or catheter may directly traumatize nerves, resulting in injury. Persistence of paresthesias or severe pain during a neuraxial technique should prompt withdrawal of the needle or catheter. Documentation of neurologic examination and pre-existing deficits prior to neuraxial procedures is important, and intrinsic nerve injuries due to labor and delivery must be distinguished from those resulting from neuraxial anesthesia. Electromyogram may be helpful in determining the amount of time a deficit has been present. Neuraxial Hematoma or Abscess Epidural bleeding or abscess can be catastrophic because of pressure exerted on the spinal cord or cauda equina. Neuraxial hematoma is a rare event, but traumatic or difficult placement and coagulopathy or anticoagulant use increase the likelihood of occurrence. The American Society of Regional Anesthesia recommendations for use of anticoagulants and placement of neuraxial anesthesia can be viewed at their website. Motor weakness that persists or worsens despite discontinuation of local anesthetic is the most common presentation for a neuraxial hematoma. Time is important in cases of neuraxial hematoma because neurologic outcomes are worse the longer treatment is delayed. Neuraxial hematoma necessitates immediate neurosurgical consultation for possible emergent decompression of the clot. Neuraxial infection may manifest as either meningitis or abscess; both are very uncommon events. Contaminants causing meningitis tend to arise from the nasopharynx of the provider who placed the block. Sterile preparation, draping, and use of a surgical mask are standard during placement of neuraxial blocks to prevent iatrogenic infection. Anesthesia for Nonobstetric Surgery during Pregnancy Nonobstetric elective surgery during a desired pregnancy is not recommended. Occasionally emergency conditions warrant surgery during pregnancy, the most common of which are appendicitis or trauma. The safest time to perform surgery during pregnancy is the second trimester because surgery during the first trimester is associated with spontaneous abortion and during the third trimester with preterm labor. Organogenesis occurs early in the first trimester, and it is still unclear what effects anesthetic agents may have on the developing fetus. In certain cases, continuous fetal monitoring may be indicated, specifically if the fetus is viable and if staff qualified to perform emergency cesarean delivery are available. Observation postoperatively is generally recommended due to the increased risk of preterm labor. Normotension, maintenance of eucarbia, and adequate oxygenation will provide the fetus and mother with adequate perfusion and oxygenation. Most anesthetic agents, other than the neuromuscular blocking agents, cross the placenta with unknown fetal effects. Neuromuscular blockade reversal agents do cross the placenta, but glycopyrrolate does not. Therefore, the anesthesiologist should reverse blockade with atropine to avoid fetal effects of reversal, including bradycardia. In summary, providing optimal anesthetic care to pregnant patients requires consideration of the many maternal physiologic changes pregnancy induces, as well as recognition of the effects of anesthesia on both the mother and the fetus. The anesthesiologist is responsible for providing analgesia for labor, but also for guiding the response to complex medical and emergency clinical situations. A thorough knowledge of the medical histories of patients who are admitted to labor and delivery, as well as coordinated multidisciplinary care, is of the utmost importance to ensure optimal outcomes for both mothers and babies. Cesarean delivery: A randomized trial of epidural analgesia versus intravenous meperidine analgesia during labor in nulliparous women. Randomized controlled comparison of epidural analgesia and combined spinal-epidural analgesia in a private practice setting: Pain scores during first and second stages of labor and at delivery. Incidence and characteristics of failures in obstetric neuraxial analgesia and anesthesia: A retrospective analysis of 19,259 deliveries. Practice guidelines for the prevention, detection, and management of respiratory depression associated with neuraxial opioid administration: An updated report by the American Society of Anesthesiologists Task Force on Neuraxial Opioids. The most common reason for difficult mask ventilation and laryngoscopy in the pregnant patient is because: A. Pregnant women have less neck mobility, making the head-tilt required difficult B.