General Information about Viagra Jelly
One potential downside of Viagra Jelly is that it can be more expensive than the capsule form. However, this price could also be price it for these who prefer the comfort and faster-acting results of Viagra Jelly. It can be necessary to note that this medication is not a treatment for Impotence but rather a temporary treatment. It is crucial to deal with any underlying causes of Impotence with a health care provider and make essential life-style modifications to take care of long-term sexual health.
So, what exactly is Viagra Jelly and how does it differ from the standard capsule form? Viagra Jelly is a gel-like substance that contains the active ingredient Sildenafil Citrate, the same ingredient found within the tablet form of Viagra. The main difference is that while the pill must be swallowed and may take up to an hour to begin working, Viagra Jelly may be taken sublingually (under the tongue) and is absorbed much quicker, usually inside 15 minutes. This makes it a well-liked selection for many who need a faster-acting and extra discreet possibility.
In conclusion, Viagra Jelly is a handy and efficient choice for those trying to treat male Impotence. Its faster absorption, discreet packaging, and variety of flavors make it a preferred choice for a lot of males. However, it is essential to seek the assistance of with a doctor before beginning any new treatment and to address any underlying causes of Impotence. With proper use and steerage, Viagra Jelly may help enhance the sexual experience and high quality of life for so much of males.
Like any medication, it is important to be aware of attainable unwanted effects. Common side effects of Viagra Jelly might embody headache, flushing, dizziness, upset abdomen, and nasal congestion. However, these side effects are sometimes mild and short-term. It is crucial to seek the assistance of with a physician before beginning any new medication, especially when you have a history of heart illness, hypertension, or are presently taking any other drugs.
Viagra Jelly is a extensively known and in style treatment used to deal with male Impotence, also called erectile dysfunction. It has been available on the market for over 20 years and has helped countless men regain their confidence and enhance their sexual performance. However, what many could not know is that there's now a model new and improved type of this medicine known as Viagra Jelly.
One of the main advantages of using Viagra Jelly is its convenience. The sachet packaging is compact and straightforward to carry, making it discreet and handy for spontaneous use. It also comes in a wide selection of flavors, corresponding to strawberry, pineapple, and banana, making it a more palatable option for individuals who have hassle swallowing pills. This could be a game-changer for many who might have prevented taking the standard capsule kind as a result of its taste.
Another benefit of Viagra Jelly is its efficacy. As talked about before, the lively ingredient Sildenafil Citrate is the same in both forms of the medicine. This means that it works in the identical way, helping to relax the blood vessels within the penis and growing blood move, resulting in a firmer and longer-lasting erection. Many males have reported seeing outcomes inside 10-15 minutes of taking Viagra Jelly, and the results can last for about 4-6 hours, similar to the capsule kind.
Open tension-free mesh repairs can be carried out under local anaesthesia as day cases and this reduces the costs considerably impotence viriesiem 100 mg viagra jelly buy with mastercard. The laparoscopic approach has a number of advantages that include less postoperative pain, earlier return to full activity and work, and reduced incidence of persistent groin pain at 1 year. The initial higher morbidity (including major vascular, bowel, bladder and nerve injuries) and high recurrence rates reflected inexperience with the technique as surgeons were not familiar with the anatomy of the posterior abdominal wall as visualized from the peritoneal side. The morbidity and recurrence rates of the laparoscopic versus open tension-free repairs are now equivalent. The residual disadvantages are increased hospital (but not total) costs and the need for general or epidural anaesthesia. Uniformly excellent results have been reported consistently with the open Lichtenstein repair using polypropylene (Marlex) mesh under local anaesthesia. Most of the recurrences occur at the pubic tubercle, usually because the mesh used was too small. A preformed mesh plug is used to fill and expand extraperitoneally occluding the defect. The technique is simple and entails minimal dissection, especially in direct hernias. However, patients undergoing the laparoscopic repair required less narcotic analgesic medication and returned Hernias 501 to full activity 1 week sooner than the open surgery group. The complications of inguinal hernia repair are: retention, especially in males ·urinary infection and haematomas wound ·scrotal swelling ·orchitis and testicular atrophy ·recurrence ·iatrogenic bladder, bowel, nerve and vascular injuries ·chronic groin pain. A Swedish study on a large cohort (n = 1232) of patients aged 1580 years operated upon for inguinal or femoral hernia involving several surgeons/ hospitals demonstrated the positive effect of audit (closing the loop) over a 10 year period. During this interval, there was a corresponding decline in the reoperation rate for recurrence at 3 years from 10. The surgical treatment of recurrent inguinal hernias is less effective and the risk of further recurrence is higher than after first time repair. It is now generally agreed that all recurrent inguinal hernias require some form of tension-free prosthetic mesh repair (open or laparoscopic). It is essential that the size of the mesh used is large enough to overlap the defect by a significant margin. The risk of further recurrence depends on the technique and the number of previous repairs. Thus, in a large reported series, patients with a first-time recurrence had recurrence rates of 2% as opposed to 9% in patients who had undergone two or more prior repairs. The morbidity of recurrent hernia repair is higher and includes wound haematoma, scrotal oedema, temporary pain at the wound site, paraesthesiae, injury of the ilioinguinal nerve and femoral hernia, although the overall morbidity can be low with good surgical technique. The hernia may, however, remain quite small and be invisible or scarcely palpable in obese patients. Of the emergency group up to 40% will have strangulation of the hernial sac contents (omentum, small bowel, vermiform appendix) requiring excision. Femoral hernias can occur at any age with peak incidence in the fifth and sixth decades and are significantly commoner in females especially if multiparous (female to male ratio 4:1). The higher incidence on the right side is inexplicable unless the right leg being in use more often than the left in severe exercise is the reason. On other occasions, the nodule, typically below and lateral to the pubic tubercle, may be difficult to differentiate from a lymph node. Treatment of femoral hernias All require surgical repair because of risk of obstruction/ strangulation. In the elective situation, the surgical approach may be from below the inguinal ligament or through the inguinal canal. Infrainguinal operations In the classic low approach, the hernial sac is isolated through an incision below the inguinal ligament. The sac is opened and emptied, with care taken to avoid injury to the bladder wall, which may be close to the medial side of the sac. The peritoneum is closed above the neck of the sac and the stump returned to the abdomen. The repair with this cylindrical mesh prosthesis inserted into the femoral canal gives better results than the classic low fascial repair and is favoured nowadays. Alternatively a mesh repair can be effected laparoscopically using the total extraperitoneal approach. Transinguinal approach the inguinal canal is opened anteriorly and then the neck of the femoral hernia exposed by incising the posterior inguinal canal wall. The sac is open and the contents are reduced, after which the peritoneum is closed and a tension-free mesh repair is effected of the posterior wall of the inguinal canal, ensuring this is of adequate size and thus overlaps the pubic tubercle. Obstructed/strangulated femoral hernia Although both the above can be used in patients with obstructed femoral hernias, the preperitoneal approach of McEvedy is recommended, especially in the presence of strangulation of the contents of the hernial sac because this gives immediate access to the peritoneal cavity. The skin incision may be longitudinal Femoral hernias the pathogenesis of femoral hernias is now thought to be related to the mode of insertion of the fibres of the transversus abdominis and its investing sheath into the superior pubic ramus and develops in two stages. If the insertion of the transversus abdominis fibres on the superior pubic ramus is through a narrow band, a cone-shaped defect overlying the femoral ring (the femoral cone) results. Initially, preperitoneal fat with or without a sac enters this femoral cone as a result of increased abdominal pressure. This is the asymptomatic stage I (internal) femoral hernia that can only be detected if the preperitoneal space is explored during inguinal herniorrhaphy. The musculoaponeurotic layer is divided lateral to the rectus abdominis, and the extraperitoneal space of the lower abdomen is entered. In this case the incision is enlarged and the peritoneal cavity entered above the sac.
Infantile umbilical hernia the worst defect is exomphalos erectile dysfunction stress viagra jelly 100 mg purchase on line, which fortunately is a rare condition, occurring in about one in 5000 births and is nowadays diagnosed prenatally. It is frequently associated with Non-incisional abdominal wall hernias these hernias occupy a good deal of surgical time and account for 1015% of all surgical operations. The majority of operations (80%) are performed for inguinal hernias, although this figure is even higher in the male population. The remainder are in the region of the umbilicus (8%), incisional (7%) and femoral hernias (5%). Rarer forms of hernias, although very interesting, form only a tiny proportion of the surgical problem. Diagnosis of abdominal wall hernias In the vast majority of patients, the diagnosis is made on history and physical examination (location of the bulge and cough impulse) and no other confirmatory tests are needed. However, diagnostic problems may be encountered especially in obese patients and those presenting with acute intestinal obstruction. Water-soluble contrast herniography is an accurate means of identifying inguinal and femoral hernias in cases presenting diagnostic problems. Simple umbilical hernia is common in infants and young children with the highest reported incidence in African Caribbean babies. In the vast majority of infantile umbilical hernias spontaneous closure occurs (reduction in size by approximately 18% each month) before the age of 4 years and thus management is conservative, especially as complications during this age period are rare. However, large infantile umbilical hernias (neck of the sac >2 cm) are unlikely to close spontaneously and surgical repair is therefore advisable. Irrespective of size, an umbilical hernia that persists beyond 4 years requires surgical repair, as closure then becomes unlikely. It is generally considered important to preserve the umbilical cicatrix after excising the sac and repairing the defect so that the child will not appear different from its fellows. The most common complication in these children is incarceration with the development of small bowel obstruction. The reported risk of this complication is approximately one in 1500 umbilical hernias. Another very rare complication reported in Nigerian children is spontaneous rupture. This usually occurs in the first year of life and is probably precipitated by raised intra-abdominal pressure from excessive crying. Adult umbilical hernia the umbilical hernia that develops in patients with refractory ascites due to chronic liver disease is often overlooked but can assume clinical significance. In the first instance incarceration is well documented as a complication of effective relief of the ascites following diuresis, paracentesis, peritoneovenous shunting and transjugular intrahepatic portosystemic shunt. Second, these patients have marked atrophy of the abdominal muscles and some have, in addition, large high-pressure veins following recanalization of the umbilical vein (caput medusae). Thus repair can be difficult and should always be conducted using prosthetic mesh, preferably of the double-stranded, closely knitted variety. In addition, subcutaneous suction drains should be avoided because of the increased risk of infection of the ascitic fluid. The majority of patients who are admitted as emergencies with complicated groin hernias have not previously sought medical attention or been diagnosed with the condition in the outpatient department. This observation implies that most hernias that develop complications do so within a relatively short time in the natural history of the disease. Mortality of obstructed hernias is high in patients with coexisting cardiorespiratory disease, whereas the morbidity rate is influenced by the viability of contents of the hernial sac. In turn, this is directly related to the duration of irreducibility/incarceration or delay in presentation. The risk factors for complications of groin hernias are: ·Adults:age old · duration of hernia: short duration <1 year type of hernia: femoral more than inguinal coexisting medical illness: especially chronic obstructive airways disease. Children: very young (infants) gender (male) short duration of hernia side (right). Inguinal hernia By far and away, inguinal hernia is the most common external abdominal hernia, accounting for over 90%. With increased intra-abdominal pressure, contraction of the internal oblique and transversus muscles acts upon the section of the transversus aponeurosis that arches convexly upwards over the medial half of the canal. The arch is pulled down and flattened and thus reinforces the posterior inguinal wall. The second mechanism, which may in fact be more important, depends upon the attachment of the strong fascial layer forming the deep inguinal ring. This fascial ring is normally firmly adherent to the posterior surface of the transversus muscle so that contraction of this muscle pulls the ring upwards and laterally. In essence, an inguinal hernia is the consequence of weakness of the posterior abdominal wall. In the past, stretching of the transversalis fascia was considered to be the most important factor and some fascial repair procedures (Shouldice operation) were based on suture plication of this layer. Some, however, consider the transversalis (endoabdominal) fascia to be the thinnest and least important layer in the prevention of inguinal hernia formation and consider that the strength of the posterior wall of the inguinal canal is due to the muscle fibres and aponeuroses of the internal oblique and transversus abdominis. There is evidence for an increased risk of right inguinal hernia after appendicectomy. This is related to the denervation of the right transversus abdominis muscle fibres.
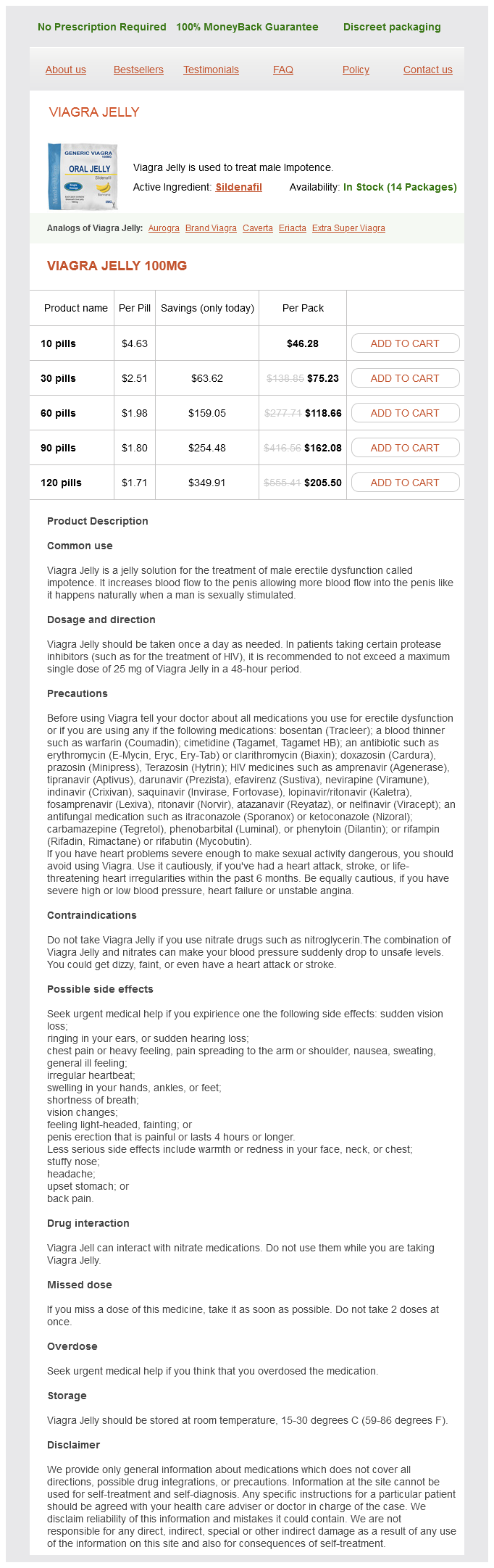
Viagra Jelly Dosage and Price
Viagra Jelly 100mg
- 10 pills - $46.28
- 30 pills - $75.23
- 60 pills - $118.66
- 90 pills - $162.08
- 120 pills - $205.50
In practice radiotherapy is reserved for tumours which are inoperable by virtue of involvement of vital structures and for postoperative treatment of tumours that have been inadequately excised because of anatomical considerations erectile dysfunction remedies purchase discount viagra jelly. This tends to occur particularly in lesions of the ear and requires a wide excision or radiotherapy. When wide excision is performed, intraoperative frozen section will help to define the extent of excision. Treatment of metastatic disease When metastatic deposits in the regional lymph nodes are detected, en bloc resection of the lymph node group is indicated and postoperative radiotherapy should be considered for poorly differentiated tumours. Currently there is no evidence for the use of prophylactic block dissection of regional lymph nodes in high-risk large tumours. Some recommend sentinel node biopsy in these cases but again the benefit of this approach remains uncertain. Metastatic lesions of the bone and brain may be treated by radiotherapy to reduce local symptoms but widespread disease will require chemotherapy. Randomized studies have established the combination of cisplatin and infusional 5-fluorouracil and paclitaxel is effective in palliation (pain relief and improved quality of life) but does not materially improve survival. A number of non-platinum agents are also active including gefitinib and the newer antifolates which target or restore deficient p53. Overall, the 5-year survival in patients with metastatic disease at presentation is 25%. Other treatment modalities these include Mohs micrographic surgery, cryotherapy, photodynamic therapy, curettage and cautery and topical therapy. Mohs micrographic surgery consists of microscopically controlled precise excision of the tumour in increasingly deeper layers until the microscopy shows no tumour cells. The lesion is first curetted (for debulking) and then cautery (electrodessication) applied to the wound. The problem with this treatment is that curettage provides poorly orientated material for histological examination and assessment of the completeness of removal is not possible. There is no level 1 evidence that other treatments such as photodynamic therapy and topical treatment with imiquimod, 5-fluorouracil paste and interferon- are effective in the long term. Increasing age, male sex, skin type I (skin that always burns and never tans), blond hair with blue/green eyes, freckles and sunburn in childhood and adolescence (as opposed to adults), immune suppression, ionizing radiation, burns and arsenic exposure are other recognized risk factors. A second procedure with wider and deeper excision should therefore be undertaken immediately unless this is contraindicated by involvement of vital structures. This risk, variously reported at 3377%, depends on the number of lesions present and location of tumour in the trunk. Clinically, it presents as a slowly growing nodule with waxy or pearly appearance associated with telangiectasia. The central scar area contains sweat glands but the hair follicles are destroyed producing characteristic alopecia. The tumour is frequently multifocal and is commonly advanced at presentation owing to the insidious nature of its development. Morphoeic basal cell carcinoma this presents as a dense greyish yellow plaque that increases in size gradually. Fibroepithelioma of Pinkus this presents as a papilloma without scaling or ulceration. Factors indicating higher risk include histological type (morphoeic), size at presentation (>2. Histologically, the tumour consists of clumps of basophilic cells surrounded by a connective tissue stroma. At the periphery of the tumour, columnar cells form a palisade which is the hallmark of the tumour. Noduloulcerative basal cell carcinoma (cystic basal cell carcinoma, rodent ulcer) this forms a well-circumscribed tumour with islands of basal cells embedded in a fibroblastic stroma. Centrally the cells are arranged randomly, but peripherally the cells form palisades. The basal cells may show differentiation towards the adnexal structures of the skin or may demonstrate squamous metaplasia. Superficial spreading basal cell carcinoma In this variant, there are nests of basiloid cells with peripheral palisading at the level of the basal layer of the epidermis with atrophy of the epidermis above this. Morphoeic basal cell carcinoma this type, which accounts for 5% of cases, is the most aggressive. Histologically, it is characterized by the presence of a dense fibrous dermal stroma with scanty strands and groups of cells embedded within it. The tumour cell strands may stream from the under surface of the tumour into the deeper tissues without definite margins. Proliferation of the stroma may also occur in the horizontal plane beneath apparently normal epidermis. Some of these tumours may be very large at presentation and cause significant disfigurement requiring lengthy plastic surgical reconstruction. Pigmented basal cell carcinoma this is similar in histological appearance to the noduloulcerative type but contains melanocytes. Fibroepithelioma of Pinkus In this variant, strands of basiloid cells extend into the deeper fibrous stroma but there is no palisading. It uses a photosensitizer drug, -aminolaevulinic acid, in a 20% emulsion applied to the tumour, which then takes it up and thereby becomes photosensitized. As a result, it is ablated when exposed to light in the wavelength range of 620670 nm. It does, however the choice of treatment in the individual case depends on the size and site of the tumour, its histological nature, the condition of the patient and, in recurrent tumours, the methods previously used.