General Information about Vermox
Vermox is usually well-tolerated, with few side effects reported. However, some individuals could experience delicate unwanted effects similar to nausea, vomiting, and belly pain. These unwanted effects are often temporary and will subside as quickly as the treatment is stopped.
It is important to note that Vermox just isn't efficient against all forms of worm infections. It just isn't effective against tapeworms or flukes, and it should not be used to deal with pregnant or breastfeeding women. It can additionally be necessary to comply with correct hygiene practices, similar to washing arms often, to forestall re-infection after remedy with Vermox.
In conclusion, Vermox is a secure and efficient medication for treating worm infections brought on by parasites corresponding to whipworm, pinworm, roundworm, and hookworm. With its capability to kill and cease the worms from reproducing, Vermox offers reduction from signs and helps forestall critical health issues. If you believe you studied that you just or your youngster may have a worm an infection, it is important to consult a healthcare professional for correct prognosis and therapy with Vermox.
Hookworm infection is brought on by a small, blood-feeding worm that may enter the body through the skin. This infection is common in areas with poor sanitation and can result in anemia and malnutrition if not treated. Vermox is a protected and efficient treatment for hookworm, with multiple doses typically beneficial for full eradication.
One of the commonest infections handled with Vermox is pinworm, also referred to as threadworm. This infection is brought on by a small, white worm that lives within the large intestine and exits the physique by way of the anus, causing intense itching within the anal area. Pinworm an infection is especially common in kids, as it is simply transmitted via contact with contaminated surfaces or objects. Vermox is an efficient remedy for pinworm, with one dose typically adequate to eradicate the an infection.
Helminths, or parasitic worms, are organisms that can reside and thrive inside the human physique. These worms can enter the body through contaminated meals, water, or soil, or via contact with infected people. Once inside the physique, these worms can cause quite a lot of symptoms including stomach pain, diarrhea, weight loss, anemia, and nutritional deficiencies. In some cases, critical complications such as liver or lung injury can occur.
Roundworm, also referred to as ascariasis, is one other widespread infection treated with Vermox. This type of worm is usually found in tropical and subtropical areas and could be transmitted by way of contaminated soil or food. If left untreated, roundworm an infection can result in malnutrition, intestinal obstruction, and impaired growth in children. Vermox is extremely effective in treating roundworm, with two doses given two weeks apart typically recommended for complete eradication.
Vermox, also called mebendazole, is an anthelmintic treatment generally used to deal with infections brought on by parasitic worms in the physique. These worms, known as helminths, may cause a selection of sicknesses and health issues if left untreated. Vermox is a secure and efficient therapy possibility for a range of worm infections, including whipworm, pinworm, roundworm, and hookworm.
Vermox works by killing the worms and stopping them from reproducing, thereby treating the an infection and relieving signs. The lively ingredient in Vermox, mebendazole, works by disrupting the worms' capacity to absorb glucose, which is important for his or her survival. Without glucose, the worms ultimately die off and are passed out of the physique by way of bowel actions.
Whipworm, or trichuriasis, is a much less common worm infection treated with Vermox. These small worms reside within the giant gut and can trigger diarrhea, belly ache, and rectal prolapse if left untreated. Vermox is an effective treatment for whipworm, with a single dose recommended for adults and two doses given two weeks aside for kids.
Their relative contributions vary between species antiviral principle order 100 mg vermox fast delivery, and it is these differences that complicate elucidation of the exact factors that regulate human parturition. When parturition is abnormal, then preterm labor, dystocia, or postterm pregnancy may result. Of these, preterm labor remains the major contributor to neonatal mortality and morbidity. In contrast to skeletal or cardiac muscle, the smooth muscle cell is not terminally differentiated and therefore is readily adaptable to environmental changes. Varied stimuli such as mechanical stretch, inflammation, and endocrine and paracrine signals can modulate the transition of the smooth muscle cell among phenotypes that provide cell growth, proliferation, secretion, and contractility. In addition to this phenotypic plasticity, several smooth muscle qualities confer advantages for uterine contraction efficiency and fetal delivery. First, the degree of smooth muscle cell shortening with contractions may be one order of magnitude greater than that attained in striated muscle cells. This differs from the contraction force generated by skeletal muscle, which is always aligned with the axis of the muscle fibers. In myometrium, the thick and thin filaments are found in long, random bundles throughout the cells. Last, greater multidirectional force generation in the uterine fundus compared with that of the lower uterine segment permits versatility in expulsive force directionality. Lining the thick muscular uterine walls, the endometrium is transformed by pregnancy hormones and is then termed decidua. Composed of stromal cells and maternal immune cells, the decidua serves to maintain the pregnancy via unique immunoregulatory functions that suppress inflammatory signals during gestation. With this, the decidua transitions to induce inflammatory signals and withdraw active immunosuppression, which contribute to parturition initiation. During pregnancy, the cervix has multiple functions that include: (1) maintenance of barrier function to protect the reproductive tract from infection, (2) maintenance of cervical competence despite greater gravitational forces as the fetus grows, and (3) orchestration of extracellular matrix changes that allow progressively greater tissue compliance. In nonpregnant women, the cervix is closed and firm, and its consistency is similar to nasal cartilage. By the end of pregnancy, the cervix is easily distensible, and its consistency is similar to the lips of the oral cavity. Observations in threedimensional sonography and magnetic resonance imaging show increases in the cross-sectional area of the cervical canal and in the cervical stroma from early to late pregnancy (House, 2009; Lang, 2010). Concurrent with expansion of the stroma, the cervical epithelia proliferate and exert a pregnancy-specific immunoprotection. Placenta In addition to providing the exchange of nutrients and waste between mother and fetus, the placenta is a key source of steroid hormones, growth factors, and other mediators that maintain pregnancy and potentially aid the transition to parturition. The fetal membranes-amnion and chorion and adjacent decidua-make up an important tissue shell around the fetus that serves as a physiological, immunological, and metabolic shield to protect against untimely parturition initiation. This avascular tissue is highly resistant to penetration by leukocytes, microorganisms, and neoplastic cells. It also constitutes a selective filter to prevent fetal particulate-bound lung and skin secretions from reaching the maternal compartment. In this manner, maternal tissues are protected from amnionic fluid constituents that could prematurely accelerate decidual or myometrial activation or could promote adverse events such as amnionic fluid embolism. The role of decidual activation in parturition is unclear but may involve local progesterone metabolism and higher prostaglandin receptor concentrations, thus enhancing uterine prostaglandin actions and cytokine production. It is also enriched with enzymes that inactivate uterotonins, which are agents that stimulate contractions. Inactivating enzymes include prostaglandin dehydrogenase, oxytocinase, and enkephalinase (Cheung, 1990; Germain, 1994). And, the removal of progesterone, that is, progesterone withdrawal, directly precedes progression of parturition. In addition, providing progesterone to some species will delay parturition via a decline in myometrial activity and continued cervical competency (Challis, 1994). In humans, however, it seems most likely that both estrogen and progesterone are components of a broader molecular system that maintains uterine quiescence. Plasma levels of estrogen and progesterone in normal pregnancy are enormous and in great excess of the affinity constants for their receptors. For this reason, it is difficult to comprehend how relatively subtle changes in the ratio of their concentrations could modulate physiological processes during pregnancy. The teleological evidence, however, for an increased progesterone-to-estrogen ratio in the maintenance of pregnancy and a decline in this ratio for parturition is overwhelming. These include cervical ripening, greater cervical distensibility, and augmented uterine sensitivity to uterotonins (Bygdeman, 1994; Chwalisz, 1994b; Wolf, 1993). The exact role of estrogen in regulation of human uterine quiescence and cervical competency is less well understood. That said, estrogen can advance progesterone responsiveness and, in doing so, promote uterine quiescence. At the end of pregnancy, estrogen aids processes that mediate uterine activation and cervical ripening. Both progesterone and estrogen bind to nuclear receptors that regulate gene transcription in a cell- and context-specific pattern. In parturition, they play a prominent role in myometrial contractility, relaxation, and inflammation. Prostaglandins interact with a family of eight different G-protein coupled receptors (p. Prostaglandins are produced using plasma membrane-derived arachidonic acid, which usually is released by the action of phospholipase A2 or C. Through prostaglandin isomerases, prostaglandin H2 is converted to active prostaglandins. Isomerase expression is tissue-specific and thereby controls the relative production of various prostaglandins.
Nursing Human milk is ideal food for newborns in that it provides age-specific nutrients hiv infection rate vietnam order vermox now, immunological factors, and antibacterial substances. Milk also contains factors that act as biological signals for promoting cellular growth and differentiation. For example, women who breastfeed have a lower risk of breast and reproductive cancer, and their children have increased adult intelligence independent of a wide range of possible confounding factors (Jong, 2012; Kramer, 2008). Breastfeeding is associated with decreased postpartum weight retention (Baker, 2008). In addition, rates of suddeninfant-death syndrome are significantly lower among breastfed infants. Bartek and colleagues (2013) estimate that a 90-percent breastfeeding rate for 12 months would save more than $3 billion annually in excess infant and maternal morbidity costs. For all these reasons, the American Academy of Pediatrics (2017) and American College of Obstetricians and Gynecologists (2016a, 2017b) supports the World Health Organization (2011) recommendations of exclusive breastfeeding for up to 6 months. Department of Health and Human Services (2011) lists some barriers to breastfeeding and suggests practical means of overcoming them. Educational initiatives that include father and peer counseling may improve these rates (Pisacane, 2005; Wolfberg, 2004). The Baby Friendly Hospital Initiative is an international program to increase rates of exclusive breastfeeding and to extend its duration. It is based on the World Health Organization (1989)Ten Steps to Successful Breastfeeding (Table 36-4). Worldwide, almost 20,000 hospitals are designated as "baby-friendly," however, only 10 to 15 percent of hospitals in the United States are so designated (Centers for Disease Control and Prevention, 2014; Perrine, 2015). Forrester-Knauss and coworkers (2013) described successful trends toward exclusive breastfeeding in Switzerland during 9 years in which a Baby-Friendly Hospital Initiative was implemented. In a large population-based study done in the United States, fewer than two thirds of term neonates were exclusively breastfed at the time of discharge (McDonald, 2012). Have a written breastfeeding policy that is regularly communicated to all health-care staff 2. Show mothers how to breastfeed and how to sustain lactation, even if they should be separated from their infants 6. Feed newborns nothing but breast milk, unless medically indicated, and under no circumstances provide breast milk substitutes, feeding bottles, or pacifiers free of charge or at low cost 7. Practice rooming-in, which allows mothers and newborns to remain together 24 hours a day 8. Help start breastfeeding support groups and refer mothers to them Adapted with permission from World Health Organization: Protecting, promoting and supporting breast-feeding: the special role of maternity services. Various individual resources available are available for breastfeeding mothers that include online information from the American Academy of Pediatrics. Care of Breasts the nipples require little attention other than cleanliness and attention to skin fissures. Fissured nipples render nursing painful, and they may have a deleterious influence on milk production. Because dried milk is likely to accumulate and irritate the nipples, washing the areola with water and mild soap is helpful before and after nursing. When the nipples are irritated or fissured, some recommend topical lanolin and a nipple shield for 24 hours or longer. Although specific evidence supporting this practice is lacking, nipple pain usually subsides by 10 days (Dennis, 2014). If fissuring is severe, the newborn should not be permitted to nurse on the affected side. Instead, the breast is emptied regularly with a pump until the lesions are healed. For example, the newborn may take into its mouth only the nipple, which is then is forced against the hard palate during suckling. Ideally, the nipple and areola are both taken in to evenly distribute suckling forces. Moreover, the force of the hard palate against the lactiferous sinuses aids their efficient emptying, while the nipple is thereby positioned closer to the soft palate. For example, with maternal cytomegalovirus infection, both virus and antibodies are present in breast milk. And, although hepatitis B virus is excreted in milk, breastfeeding is not contraindicated if hepatitis B immune globulin is given to the newborns of affected mothers. Maternal hepatitis C infection is not a contraindication because breastfeeding has not been shown to transmit infection (Society for Maternal-Fetal Medicine, 2017). Women with active herpes simplex virus may suckle their infants if there are no breast lesions and if particular care is directed to hand washing before nursing. Drugs Secreted in Milk Most drugs given to the mother are secreted in breast milk, although the amount ingested by the infant typically is small. Many factors influence drug excretion and include plasma concentration, degree of protein binding, plasma and milk pH, degree of ionization, lipid solubility, and molecular weight (Rowe, 2013). The ratio of drug concentration in breast milk to that in maternal plasma is the milk-toplasma drug-concentration ratio. Ideally, to minimize infant exposure, medication selection should favor drugs with a shorter half-life, poorer oral absorption, and lower lipid solubility. If multiple daily drug doses are required, then each is taken by the mother after the closest feed. Single daily-dosed drugs may be taken just before the longest infant sleep interval-usually at bedtime (Spencer, 2002). Only a few drugs are absolutely contraindicated while breastfeeding (Berlin, 2013; Bertino, 2012).
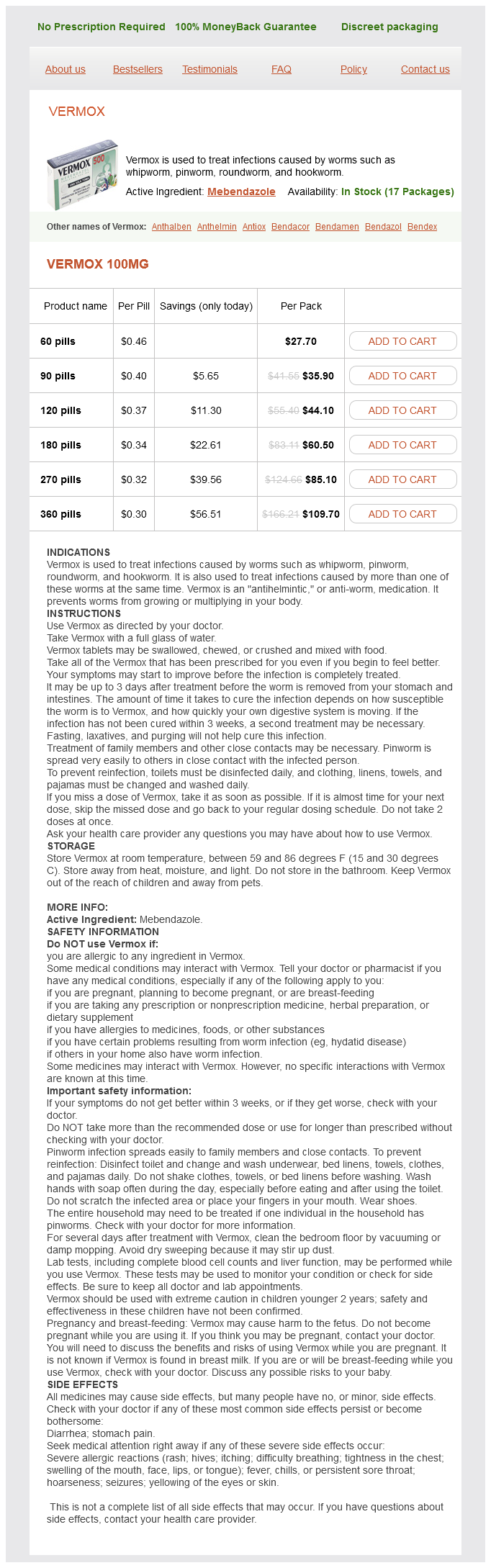
Vermox Dosage and Price
Vermox 100mg
- 60 pills - $27.70
- 90 pills - $35.90
- 120 pills - $44.10
- 180 pills - $60.50
- 270 pills - $85.10
- 360 pills - $109.70
This can require up to 8 hours or more before cesarean delivery is performed for dystocia anti viral hand wash 100 mg vermox purchase. The cumulative time required to effect this stepwise management approach permits many women to establish effective labor. This management protocol has been evaluated in more than 20,000 women with uncomplicated pregnancies. Importantly, these labor interventions and the relatively infrequent use of cesarean delivery did not jeopardize the fetusnewborn. Obstet Gynecol 100:46, 2002 Althabe F, Buekens P, Bergel E, et al: A behavioral intervention to improve obstetrical care. N Engl J Med 358:1929, 2008 American Academy of Pediatrics and the American College of Obstetricians and Gynecologists: Guidelines for Perinatal Care, 8th ed. Committee Opinion 71, August 1989 American College of Obstetricians and Gynecologists: Hospital-based triage of obstetric patients. Am J Obstet Gynecol 187:430, 2002 Carlhäll S, Källén K, Blomberg M: Maternal body mass index and duration of labor. Clin Biochem 46(18):1816, 2013 Dujardin B, De Schampheleire I, Sene H, et al: Value of the alert and action lines on the partogram. Lancet 339:1336, 1992 Dupuis O, Silveira R, Zentner A, et al: Birth simulator: Reliability of transvaginal assessment of fetal head station as defined by the American College of Obstetricians and Gynecologists classification. Am J Obstet Gynecol 192:868, 2005 Eason E, Labrecque M, Wells G, et al: Preventing perineal trauma during childbirth: a systematic review. N Engl J Med 333:745, 1995 Gardberg M, Tuppurainen M: Anterior placental location predisposes for occiput posterior presentation near term. Acta Obstet Gynecol Scand 73:151, 1994a Gardberg M, Tuppurainen M: Persistent occiput posterior presentation-a clinical problem. Am J Obstet Gynecol 108:751, 1970 Herbst A, Källén K: Time between membrane rupture and delivery and septicemia in term neonates. Obstet Gynecol 67:727, 1986 Lydon-Rochelle M, Albers L, Gorwoda J, et al: Accuracy of Leopold maneuvers in screening for malpresentation: a prospective study. Obstet Gynecol 130(1):139, 2017 Noumi G, Collado-Khoury F, Bombard A, et al: Clinical and sonographic estimation of fetal weight performed in labor by residents. Am J Obstet Gynecol 192:1407, 2005 Nygaard I: Pelvic floor recovery after childbirth. J Obstet Gynaecol Br Commonw 76:817, 1969 Saccone G, Berghella V: Antibiotic prophylaxis for term or near-term premature rupture of membranes: metaanalysis of randomized trials. Am J Obstet Gynecol 161(3):562, 1989 Staer-Jensen J, Siafarikas F, Hilde G, et al: Postpartum recovery of levator hiatus and bladder neck mobility in relation to pregnancy. At the same time, the cervix, which was becoming obliterated and dilated in a satisfactory manner, ceases to make further progress and labour apparently comes to a standstill. Whitridge Williams (1903) the term dystocia as described by Williams in the first edition of this text still applies today. It literally means difficult labor and is characterized by abnormally slow labor progress. Similar to the factors described by Williams, dystocia arises from three distinct abnormality categories. First, uterine contractions may be insufficiently strong or inappropriately coordinated to efface and dilate the cervix -uterine dysfunction. Also, voluntary maternal muscle effort during second-stage labor may be inadequate. Second, fetal abnormalities of presentation, position, or anatomy may slow progress. Or, soft tissue abnormalities of the reproductive tract may form an obstacle to fetal descent. More simply, these alterations can be mechanistically simplified into three categories that include abnormalities of the powers-uterine contractility and maternal expulsive effort; of the passenger-the fetus; and of the passage-the pelvis and lower reproductive tract. Commonly used expressions today such as cephalopelvic disproportion and failure to progress are used to describe ineffective labors. Of these, cephalopelvic disproportion is a term that came into use before the 20th century to describe obstructed labor resulting from disparity between the fetal head size and maternal pelvis. But, the term originated at a time when the main indication for cesarean delivery was overt pelvic contracture due to rickets (Olah, 1994). Such absolute disproportion is now rare, and most cases result from malposition of the fetal head within the pelvis (asynclitism) or from ineffective uterine contractions. True disproportion is a tenuous diagnosis because many women who undergo cesarean delivery for this reason subsequently deliver even larger newborns vaginally in subsequent pregnancies. A second phrase, failure to progress in either spontaneous or stimulated labor, has become an increasingly popular description of ineffectual labor. This term reflects lack of progressive cervical dilation or lack of fetal descent. Common Clinical Findings in Women with Ineffective Labor Inadequate cervical dilation or fetal descent: Protracted labor-slow progress Arrested labor-no progress Inadequate expulsive effort-ineffective pushing Fetopelvic disproportion: Excessive fetal size Inadequate pelvic capacity Malpresentation or position of the fetus Abnormal fetal anatomy Ruptured membranes without labor Mechanisms of Dystocia At the end of pregnancy, the fetal head encounters a relatively thick lower uterine segment and undilated cervix. With the onset of labor, the factors influencing progress are uterine contractions, cervical resistance, and the forward pressure exerted by the leading fetal part. After complete cervical dilation, the mechanical relationship between the fetal head size and position and the pelvic capacity, namely fetopelvic proportion, becomes clearer as the fetus attempts to descend. Because of this, abnormalities in fetopelvic proportions become more apparent once the second stage is reached.