General Information about Verapamil
When taken as directed, Verapamil can successfully control the signs of SVT, including heart palpitations, chest ache, and shortness of breath. It can also reduce the frequency and severity of SVT episodes and enhance the general high quality of life for those dwelling with this condition.
In conclusion, Verapamil is a commonly used medication for the treatment of supraventricular tachycardia. By blocking calcium channels in the coronary heart, it helps to control the guts price and enhance symptoms of SVT. While it is generally well-tolerated, precautions ought to be taken, and patients ought to closely monitor for any potential unwanted effects. With proper medical steering, Verapamil can present significant aid for those residing with SVT, allowing them to lead a more normal and comfortable life.
Verapamil is a widely prescribed and generally secure medicine that has been used for many years in the remedy of SVT. However, it is necessary to note that it is in all probability not suitable for everyone. Patients with certain coronary heart circumstances, liver or kidney illness, or a historical past of coronary heart failure should consult with their doctor earlier than taking this medication. Additionally, pregnant or breastfeeding girls ought to search medical recommendation before beginning Verapamil treatment.
Verapamil is on the market in different types, together with immediate-release tablets, sustained-release tablets, and extended-release capsules. The dose and frequency of administration rely upon the individual’s medical condition and response to the medication. Often, the doctor will start with a decrease dose and progressively enhance it to realize the specified effect.
As with any treatment, there are some potential unwanted aspect effects related to Verapamil. These can embrace dizziness, headache, flushing, low blood stress, constipation, and nausea. In uncommon cases, more critical unwanted aspect effects may occur, such as irregular heartbeat, coronary heart failure, or allergic reactions.
It is necessary to comply with the dosage instructions rigorously and to monitor for any opposed effects. Patients must also inform their doctor of another medicines they're taking, as Verapamil might work together with sure antibiotics, blood thinners, and different medicines.
Verapamil, also recognized by its model name Calan, is a widely used medicine for treating supraventricular tachycardia (SVT). SVT is a type of heart rhythm dysfunction the place the center beats sooner than normal, usually above one hundred beats per minute. It is brought on by abnormal electrical impulses in the higher chambers of the center, often recognized as the atria.
Verapamil belongs to a category of medicines called calcium channel blockers. It works by blocking the entry of calcium ions into the muscle tissue of the center, which relaxes and widens the blood vessels, permitting for improved blood flow and a slower coronary heart price. This helps to decrease the workload and oxygen demand of the center, making it particularly useful in treating SVT.
Screen and treat for retinopathy and coronary artery disease prior to conception 230 Diabetic Nephropathy Answers 1 blood pressure medication helps acne buy verapamil with a visa. Strict arterial blood pressure control has proven to be one of the most important factors in preventing or delaying progression of diabetic nephropathy, and other cardiovascular complications. Studies support the recommendation that all patients with diabetes should be treated for hypertension with a target blood pressure of less than 140/90 mmHg. In patients with coexisting microalbuminuria, a more intensive blood pressure target of 130/80 is supported by some additional studies. It is likely that the specific benefits of these drugs relate to their ability to alter intraglomerular pressure, owing to the role of angiotensin in causing efferent arteriolar vasoconstriction. If a patient with diabetes experiences a sudden deterioration in renal function, it is unlikely to be due to diabetic nephropathy alone. All patients with diabetes should be screened on a regular basis for evidence of early diabetic nephropathy so that interventions may be undertaken to prevent or delay its progression. Sulphonylureas can be used but run a higher risk of causing hypoglycaemia given the reduced renal clearance. Blood glucose control is a strong predictor of the risk of diabetic nephropathy, though there is significant intraindividual variation. Smoking habits, and the amount and origin of dietary protein also seem to play a role as risk factors. It is vital to strictly control blood glucose levels and blood pressure during pregnancy to reduce maternal and foetal complications. Choice of antihypertensive medication use in pregnancy is limited due to potential for teratogenicity. Phanish and Vinay Sakhuja Summary · Plasma cell dyscrasias are a heterogenous group of disorders characterized by the proliferation of monoclonal bone marrow plasma cells. Clinical manifestations can range from relatively benign presentation with an incidental discovery of paraprotein to an aggressive malignant disease. These diseases are often associated with kidney disease, and advanced kidney disease can limit treatment options, making early diagnosis and treatment an essential aspect of care given to these patients. Light chains, by virtue of their smaller size, are freely filtered across the glomeruli and hence cause nephrotoxicity, as discussed later. The plasma cells proliferate in the bone marrow and can cause extensive skeletal damage. Up to 10% of patients present in severe renal failure needing dialysis and only 1530% of these patients can discontinue dialysis. Myeloma accounts for around 13% of all haematological cancers and is characterized by dysregulated overproduction of immunoglobulins by a single clone of malignant plasma cells. Paraproteins produced are immunoglobulin (Ig) G in 52%, IgA in 21%, kappa or lambda light chain only (BenceJones protein) in 16%, IgD in 2%, biclonal in 2%, IgM in 0. Evidence of endorgan damage that can be attributed to the underlying plasma cell proliferative disorder, specifically: · Hypercalcaemia: serum calcium >0. These tubular casts occlude the tubular lumen, leading to cast nephropathy (myeloma kidney) and the resultant renal failure. The greater the urinary excretion of free light chains, the greater is the risk for renal failure. The obstructing casts elicit a surrounding interstitial inflammatory reaction with or without multinucleated giant cells and at times lead to tubular rupture, allowing escape of the light chains into the interstitium and leading to an interstitial inflammatory process. The amount of filtered free light chains (light chain load) is a critical factor for the development of cast nephropathy. Excessive monoclonal light chains freely filtered by the glomerulus lead to intratubular cast formation and elicit an inflammatory reaction. The risk of renal failure is twice as high in patients with pure light chain myeloma. More than 70% of patients who secrete >10 g/day of light chains develop renal failure [5]. Whilst both kappa and lambda light chains can cause renal injury, some Volume depletion, by slowing down the flow within the tubules, which can promote cast formation. Metabolic acidosis, which by lowering the urinary pH promotes the binding of free light chains to TammHorsfall protein. Radiocontrast agents, which may interact with light chains and promote intratubular obstruction. It is important to note that light chains in urine are not detected by urinary dipsticks. Interestingly, when light chains from patients with myeloma cast nephropathy are injected into mice, they precipitate in tubules, causing cast nephropathy more frequently when compared to light chains from myeloma patients with normal renal function. This suggests that these light chains causing cast nephropathy are inherently abnormal [6]. Glomeruli are typically spared unless there is associated amyloidosis or light chain deposition disease. Treatment of Myeloma Cast Nephropathy Correction of Reversible Factors these patients often present with significant dehydration and require aggressive hydration with intravenous normal saline. The use of frusemide to promote diuresis should be avoided, as increased distal delivery of sodium (Na+) and acidic urinary pH can increase binding of free light chains to TammHorsfall protein and thus promote tubular cast formation. Alkalinization of urine with intravenous sodium bicarbonate inhibits cast formation by inhibiting the 236 Kidney Disease in Myeloma interaction between the free light chains and Tamm Horsfall protein [7]. Reducing the Production of Light Chains Chemotherapy aimed at rapid reduction in the levels of free light chains has resulted in significant improvements in both renal recovery and overall survival [8]. The immediate commencement of highdose dexamethasone is advised, as the plasma cells are highly responsive to corticosteroids. The firstline agent in the current era is bortezomib, which is a potent proteasome inhibitor.
Whilst histological examination of renal allograft tissue may show deposition of Gb3 in tubular epithelial and endothelial cells blood pressure medication to treat acne purchase verapamil 120 mg visa, these deposits appear to be insufficient to compromise allograft function [33]. Overall, kidney transplantation has an excellent longterm outcome in these patients [34]. The cystic fibrosis transmembrane conductance regulator mediates transepithelial fluid secretion by human autosomal dominant polycystic kidney disease epithelium in vitro. Cystic fibrosis and the phenotypic expression of autosomal dominant polycystic kidney disease. Tissue Doppler imaging in the evaluation of left ventricular function in young adults with autosomal dominant polycystic kidney disease. Magnetic resonance imaging evaluation of hepatic cysts in early autosomaldominant polycystic kidney disease: the consortium for radiologic imaging studies of polycystic kidney disease cohort. An ultrasound renal cyst prevalence survey: specificity data for inherited renal cystic diseases. Xlinked Alport syndrome: natural history in 195 families and genotypephenotype correlations in males. Persistent familial hematuria in children and the locus for thin basement membrane nephropathy. The tuberous sclerosis 2000 study: presentation, initial assessments and implications for diagnosis and management. Enzyme replacement therapy for Anderson Fabry disease: a complementary overview of a Cochrane publication through a linear regression and a pooled analysis of proportions from cohort studies. The commonest diagnosis seen on renal biopsy of patients with asymptomatic haematuria is: a. Benign tumours starting in the epithelial tissue of a gland or glandlike structure c. Focal but disorganized collection of normal tissue that grow at the same rate as normal tissue 194 Hereditary and Familial Renal Diseases Answers 1. Trimethoprimsulfamethoxazole and fluoroquinolones by virtue of their lipophilic nature are able to cross the lipidrich cyst wall and achieve good intracystic concentration. It is estimated that 2025% of patients who have renal biopsy for asymptomatic haematuria have thin basement membrane nephropathy. IgA nephropathy is the commonest cause of glomerulonephritis worldwide but the question was for patients with asymptomatic haematuria and not glomerulonephritis. Patients with postinfectious glomerulonephritis and lupus nephritis are unlikely to present with just asymptomatic haematuria. Hamartomas are focal but disorganized collection of normal tissue that grows at the same rate as normal tissue; they often cause problems by virtue of their location. It is essentially the outcome of a sequence of reductions in renal perfusion induced by increasingly severe hepatic injury. However, with ongoing or worsening hepatic injury, the kidneys are unable to sustain the generation of enough local vasodilators. The urea cycle occurs in the liver and therefore patients with advanced liver disease have a low urea generation. These patients are also likely to have reduced meat intake and decreased muscle mass, often leading to a lower than expected serum creatinine level. Prerenal disease is also usually reversible when diuretics or nephrotoxins are withheld, or when the acute precipitating event is addressed. These patients often have multiorgan failure with low blood pressure and hyponatraemia. Whilst patients may not be oliguric at presentation, the urine output tends to drop with disease progression. Usually no precipitating cause is identified and the condition reflects the natural course of the disease. Vasoconstriction increases the effective arterial blood volume and leads to better renal perfusion and some reversal of the condition [2]. Midodrine, by its alpha1 adrenergic agonist activity, is a systemic vasoconstrictor, whilst octreotide is an inhibitor of endogenous vasodilators [11, 12]. Terlipressin with Albumin Terlipressin is a vasopressin analogue which reverses splanchnic vasodilatation. Although the optimum duration of therapy is not clear, it is usually continued for 15 days or until serum creatinine decreases to less than 133 mol/l (1. Terlipressin therapy with and without albumin for patients with hepatorenal syndrome: results of a prospective, nonrandomized study. Terlipressin plus albumin infusion: an effective and safe therapy of hepatorenal syndrome. Renal failure in cirrhotic patients: role of terlipressin in clinical approach to hepatorenal syndrome type 2. Beneficial effects of terlipressin in hepatorenal syndrome: a prospective, randomized placebo controlled clinical trial. Terlipressin in patients with cirrhosis and type 1 hepatorenal syndrome: a retrospective multicenter study. The effects of chronic treatment with octreotide versus octreotide plus midodrine on systemic hemodynamics and renal hemodynamics and function in nonazotemic cirrhotic patients with ascites. Effects of noradrenalin and albumin in patients with type I hepatorenal syndrome: a pilot study. Caused by imbalance between renal vasodilatation and splanchnic vasoconstriction d.
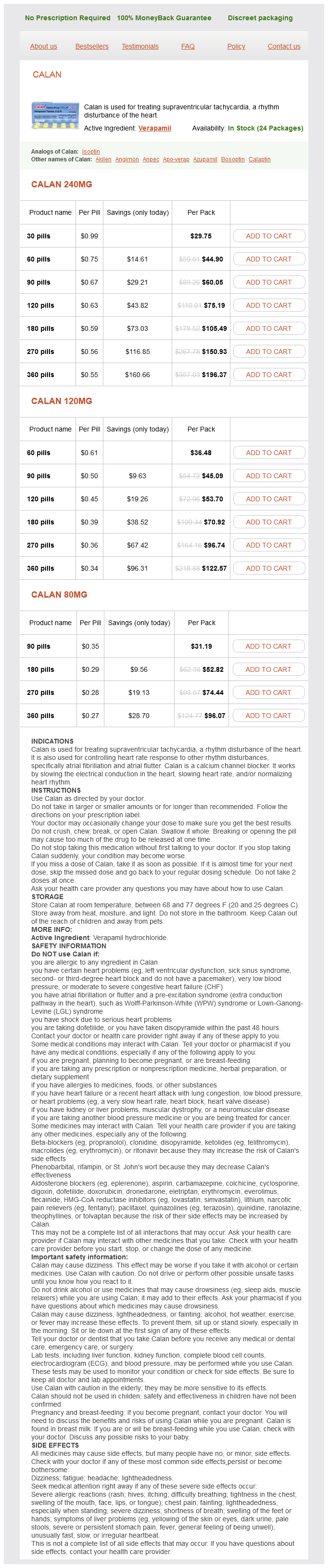
Verapamil Dosage and Price
Calan 240mg
- 30 pills - $29.75
- 60 pills - $44.90
- 90 pills - $60.05
- 120 pills - $75.19
- 180 pills - $105.49
- 270 pills - $150.93
- 360 pills - $196.37
Calan 120mg
- 60 pills - $36.48
- 90 pills - $45.09
- 120 pills - $53.70
- 180 pills - $70.92
- 270 pills - $96.74
- 360 pills - $122.57
Calan 80mg
- 90 pills - $31.19
- 180 pills - $52.82
- 270 pills - $74.44
- 360 pills - $96.07
Repeat doses can be given but it is recommended to keep serum osmolality less than 320 mOsm/L blood pressure chart malaysia 120 mg verapamil purchase visa. There is no evidence to recommend tight glucose control in head injured patients, nor is there evidence suggesting the use of immune modulating diets at this time. Elevating the head of the bed 30 degrees while keeping it in the midline position enhances cerebral venous outflow. Therefore, we believe current standard of care is normothermia for traumatic brain injury in children. Common causes of hydrocephalus include obstructed ventricular shunts, aqueductal stenosis/compression as a result of congenital malformations, infection, posterior fossa tumors, or intracranial bleeding. Following a posterior fossa craniectomy, hemorrhage into the posterior fossa can compromise respiration, and if there is an externalized ventricular drain present, output should be carefully inspected. Status Epilepticus in Children Status epilepticus is a continuous motor seizure that lasts for more than 20 minutes or a series of seizures without intercurrent awakening. Although it is common for physicians to never find a cause of the seizures, the most commonly diagnosed causes are infections (meningitis or encephalitis) and metabolic abnormalities (toxins, head trauma, and hypoxic and ischemic injury). Because seizure activity increases with status epilepticus, brain and skeletal muscle metabolism and oxygen consumption increase and place the child at risk for cellular hypoxia. During a seizure, airway obstruction and ineffective chest wall and diaphragmatic excursion can limit ventilation and worsen arterial hypoxemia and hypercapnia. Treatment of a seizure begins with establishing a patent airway, administering oxygen, and ensuring adequate ventilation. Commonly used anticonvulsants include lorazepam, phenobarbital, paraldehyde, and phenytoin. Phenobarbital, 5- to 10- mg/kg boluses (maximal dose of 20 mg/kg), also stops seizures. The main complication of lorazepam is respiratory depression when administered in high doses. Giving both phenobarbital and lorazepam together exaggerates the respiratory depression. Fosphenytoin is also given intravenously in doses of up to 20 mg/kg and should be administered slowly to avoid cardiovascular depression. Once the seizures are under control, the cause of the seizures must be determined. Embryologic development of the renal system begins in the middle of the third week of gestation with development of the pronephric tubules. Because the placenta is the major excretory organ of the fetus, renal growth is not governed by functional requirements. Renal growth increases linearly with body weight and body surface area during the third trimester of pregnancy. The renal tubular glucose threshold of term infants is similar to that of adults, but it is only 125 to 150 mg/dL in premature infants. A full-term infant has 1% or less fractional excretion of sodium by the third day of life. Renin, angiotensin, and aldosterone concentrations are high in newborns and decrease over the first few weeks of life. Creatinine is an end product of skeletal muscle catabolism and is excreted solely by the kidneys and blood urea nitrogen is a byproduct of protein metabolism. An important aspect of critical care is the maintenance of appropriate fluid balance in the critically ill child. The ascending loop diuretic furosemide is likely one of the most widely used drugs in pediatric intensive care. Electrolyte and renal function need to be monitored frequently, as diuretic therapy frequently causes significant hypokalemia and hypochloremia, as well as other electrolyte wasting. Furosemide is albumin-bound and, in low albumin states, often found in critical illness, the delivery of furosemide to renal secretory sites is decreased. Improved delivery and diuresis is often improved with the administration of 25% albumin just before or with the diuretic. Additional diuretics acting at other locations such as hydrochlorothiazide (distal tubule) can are often used as adjuvant medications to improve diuresis. The drug spironolactone, which blocks the hormone aldosterone, is a weak diuretic but may prevent spare potassium loss. Failure of increasing amounts of diuretics to be effective likely represents worsening renal perfusion and or renal failure. Acute renal failure is defined as an abrupt, often temporary loss of renal function (see Chapters 17 and 42), where there is insufficient removal of nitrogenous wastes and problems with fluid and electrolyte balance. Acute renal failure is described by (1) the area of obstruction (prerenal, postrenal [obstructive], or intrinsic renal disorders); and (2) the urine volume (oliguria, polyuria, and anuria). Urine composition is often altered, and fluid, electrolyte, and acid-base disorders are common in acute renal failure. Common causes include hypoperfusion, obstruction, toxins, drugs, inflammation, and autoimmune disorders. Prerenal causes are common in the critically ill child due to systemic hypoperfusion and reduced renal blood flow, resulting in reduced urine output and results in azotemia and ischemic renal damage. Azotemia is the term for the accumulation of nitrogenous byproducts of protein metabolism. Intravascular fluids in the case of dehydration or fluids and inotropic support may be needed to reverse prerenal renal failure. Intrinsic renal failure is caused by disorders of the renal glomeruli, tubules, or blood vessels.