General Information about Vasodilan
Raynaud disease is one other medical situation that affects blood move, causing episodes of decreased blood supply to the fingers and toes, resulting in numbness, tingling, and pain. Vasodilan can be used to help loosen up and widen the blood vessels in these areas, reducing the frequency and severity of those episodes.
Buerger illness, also referred to as thromboangiitis obliterans, is a uncommon situation that impacts the small and medium-sized blood vessels in the legs and arms. This may find yourself in decreased blood flow to these areas, resulting in ulcers and gangrene. Vasodilan can be used as part of the treatment plan for Buerger illness, as it helps to enhance blood circulate and stop further injury to the affected areas.
While Vasodilan is efficient in bettering blood move within the circumstances talked about above, it might even have some side effects corresponding to nausea, dizziness, and headaches. It is essential to speak to your doctor about another medications you might be taking or any medical conditions you may have before starting Vasodilan.
One of the principle uses of Vasodilan is in treating cerebral vascular insufficiency. This condition occurs when there's not sufficient blood circulate to the mind, which might result in symptoms similar to dizziness, reminiscence loss, and issue concentrating. By dilating the blood vessels, Vasodilan helps to extend the availability of oxygen to the mind, enhancing its function and lowering these symptoms.
It can be important to note that Vasodilan should not be utilized in pregnant girls or those that have a historical past of coronary heart disease, low blood strain, or kidney disease. It must also be used with warning in sufferers with an overactive thyroid or diabetes.
Vasodilan, also known by its generic name isoxsuprine, is a drugs used to enhance blood circulate in certain medical conditions. It belongs to a category of drugs called vasodilators, which work by stress-free the muscular tissues in blood vessel walls, thereby increasing the diameter of the vessels and improving blood circulate.
In conclusion, Vasodilan is a medication that's beneficial in enhancing blood move in sure medical situations, similar to cerebral vascular insufficiency, arteriosclerosis obliterans, Buerger disease, and Raynaud illness. By helping to chill out and widen blood vessels, it might possibly alleviate symptoms and improve overall functioning. However, it ought to all the time be used under the steerage of a well being care provider and any potential unwanted effects must be mentioned.
Vasodilan works by directly affecting the muscle tissue within the partitions of blood vessels, inflicting them to relax and widen. This permits more blood to flow through and reach areas which will have been experiencing lowered blood supply.
Another condition that Vasodilan is usually used for is arteriosclerosis obliterans, a medical situation that impacts the arteries within the legs and arms. This situation causes narrowing and hardening of the arteries, which might result in ache, numbness, and cramping in the affected limbs. By bettering blood circulate to these areas, Vasodilan helps to alleviate these signs and improve general functioning.
The functional diversification of the immune response into different anatomical compartments requires a finely coordinated system to connect and unify the defense reaction hypertension xerostomia cheap vasodilan 20 mg on line. A process of lymphocyte recirculation has evolved to allow naïve lymphocytes to Mucosal Immunology. A naïve lymphocyte re-circulates continuously between the blood and secondary lymphatic organs (von Andrian and Mackay, 2000). The recirculation process encompasses distinct phases during which the blood-borne lymphocyte transiently interacts with vascular endothelium, during which firm adhesion is activated before transmigration across endothelium into the tissue. The cell is then guided through the stroma before exiting tissue via efferent lymphatics that drain back to the central veins. This recirculation continues until the cell either dies or finds its antigen, which has been carried from the external surfaces via the afferent lymphatics into the secondary lymphatic organ. However, the activated immunoblast shows a strong preference to migrate back to the initial area that supplied antigen to the secondary lymphatic organ in which the cell first became activated. For instance, a lymphocyte that meets its antigen in the Peyer patch of the gut proliferates and differentiates locally before being carried via efferent lymphatics into mesenteric lymph nodes and then via the main lymphatic trunks to the circulation. This activated cell no longer extravasates at a random anatomical location but instead migrates preferentially into the lamina propria of the gut (or related mucosa-associated lymphatic organs) to exert its effector functions. This tissue-tropism ensures that the immune response is targeted to the sites that are most likely to be exposed to the same invading stimulus in the future. The unique morphology of these endothelial cells, their expression of adhesion receptors, and hemodynamic factors render them especially attractive for blood-borne lymphocytes. In contrast, few lymphocytes adhere to non-inflamed flat endothelial cells lining normal venules, whereas memory/ effector lymphocytes bind avidly to these vessels during acute inflammation. Inflamed skin, brain, lung, synovial tissue in joints, and liver all have lymphocyte homing specificities with distinct characteristics. Lymphocyte homing to the inflamed skin involves homing receptors imprinted on immunoblasts during activation in peripheral lymph nodes but the site of activation of synovia-, pancreas- and liver-seeking cells is less well understood. At the molecular level, each step is governed by distinct adhesion receptors belonging to different structural families (Agace, 2006). Selectins and their carbohydrate ligands mediate initial capture under shear stress (Zarbock et al. This capture process must be able to arrest cells that travel 500 times their own diameter in 1 s. Whereas selectin binding occurs without the need for activation, optimal integrin binding requires conformational changes and rapid increases in affinity and/or avidity in response to activating stimuli. In most cases, activation is achieved by binding of chemoattractant cytokines (typically chemokines) to seven transmembrane spanning G-protein linked receptors (Sallusto and Baggiolini, 2008), which promotes the binding of lymphocyte integrins to their immunoglobulin superfamily ligands on vascular endothelium. These interactions promote stable adhesion, intravascular crawling, and transmigration (Ley et al. Although the expression of many adhesion receptors is induced or increased at sites of inflammation, in many situations the activation state of an adhesion molecule is more important functionally than the absolute level of expression. Although the expression and function of adhesion molecules differ between leukocyte subsets, the basic principles of leukocyteendothelial interactions apply to lymphocytes, monocytes/macrophages, and granulocytes. Thereafter, these cells use other non-tissue selective adhesion mechanisms to secure stable adhesion and subsequent transmigration. A consequence of activation in mucosal lymphatic tissues is a relative loss of L-selectin on the progeny of activated lymphocytes and increased synthesis of 47 integrin, which is also modulated into a more functionally active state. The adhesion cascade is described in Lymphocyte Trafficking by Agace and Luster (Chapter 41). The initial interactions take place within milliseconds of contact between the lymphocyte and the endothelium, whereas activation and stable adhesion occur over minutes and transmigration is estimated to be complete within 1015 min. Systemic Manifestations of Mucosal Diseases Chapter 90 1751 effector cells to invade mucosal tissue. The same chemokines may also dictate tissue-specificity of lymphocyte homing at the endothelial cell level (Campbell and Butcher, 2002). Although these molecules are not restricted to synovial tissue, functional evidence strongly supports the existence of a joint-specific multidigit extravasation code. Evidence supports the existence of lymphocyte traffic to and from the pancreas, although under normal conditions few lymphocytes are detected within either compartment. Lymphocyte Homing to Liver Has Several Unique Characteristics the liver has a unique vasculature receiving 75% of its blood from the intestine via the portal vein and the remaining 25% from the hepatic artery. The sinusoids are lined by a unique fenestrated endothelium that possesses potent scavenging properties, and resident macrophages (Kupffer cells) that rapidly phagocytose potentially harmful pathogens or antigens from sinusoidal blood. Thus, the liver acts as a second firewall to prevent the spread of infection that evades immune surveillance in the gut (Adams and Eksteen, 2006). Lymphocytes can enter the liver through portal tract vessels and, more important, via the sinusoids (Lalor and Adams, 1999; Xu et al. Several Homing-Associated Molecules Are Up-Regulated on Inflamed Synovial Endothelium Vessels in inflamed synovia also display characteristics of a unique binding specificity, although joint-restricted adhesion molecules have yet to be discovered. Evidence that such molecules exist stems from finding peptides that specifically bind to synovial vasculature in vivo (Lee et al. Likewise, when patients with spondylarthropathies are carefully investigated, many are found to have either macroscopic or microscopic inflammatory lesions in the bowel (Cua and Sherlock, 2011). Moreover, in a subpopulation of rheumatoid arthritis patients, the severity of arthritic disease is regulated by dietary factors and more than a quarter of individuals who undergo jejunocolic bypass operations develop arthritic symptoms. Interestingly, surgical reversal of the bypass is followed by immediate and permanent remission of the arthritis (Kevans et al. Intestinal infections caused by bacteria such as Salmonella, Shigella, and Yersinia are also commonly followed by a reactive arthritis accompanied by detectable levels of bacterial antigens in the affected joints. There is mounting evidence that an enteric dysbiosis results in microbiota in the gastrointestinal tract initiating and sustaining inflammatory arthropathies such as rheumatoid arthritis and spondylarthritis (Yeoh et al.
Display of heterologous proteins on the surface of Lactococcus lactis using the H and W domain of PrtB from Lactobacillus delburueckii subsp hypertension patient teaching discount vasodilan express. The shdA gene is restricted to serotypes of Salmonella enterica subspecies I and contributes to efficient and prolonged fecal shedding. Regulated delayed expression of rfc enhances the immunogenicity and protective efficacy of a heterologous antigen delivered by live attenuated Salmonella enterica vaccines. Regulated delayed expression of rfaH in an attenuated Salmonella enterica serovar Typhimurium vaccine enhances immunogenicity of outer membrane proteins and a heterologous antigen. Palmitoylation state impacts induction of innate and acquired immunity by the Salmonella enterica serovar Typhimurium msbB mutant. Phosphate groups of lipid A are essential for Salmonella enterica serovar Typhimurium virulence and affect innate and adaptive immunity. Salmonella synthesizing 1-dephosphorylated [corrected] lipopolysaccharide exhibits low endotoxic activity while retaining its immunogenicity. Effect of deletion of genes involved in lipopolysaccharide core and O-antigen synthesis on virulence and immunogenicity of Salmonella enterica serovar Typhimurium. Utilizing Salmonella for antigen delivery: the aims and benefits of bacterial delivered vaccination. Regulated programmed lysis of recombinant Salmonella in host tissues to release protective antigens and confer biological containment. Safety and immunogenicity of Vi conjugate vaccines for typhoid fever in adults, teenagers, and 2- to 4-year-old children in Vietnam. Histomorphometric evaluation of intestinal cellular immune responses in pigs immunized with live oral F4ac+ non-enterotoxigenic E. Autodisplay: development of an efficacious system for surface display of antigenic determinants in Salmonella vaccine strains. A live oral recombinant Salmonella enterica serovar Typhimurium vaccine expressing Clostridium perfringens antigens confers protection against necrotic enteritis in broiler chickens. Oral immunization of broiler chickens against necrotic enteritis with an attenuated Salmonella vaccine vector expressing Clostridium perfringens antigens. Mucosal immunization with surfacedisplayed severe acute respiratory syndrome coronavirus spike protein on Lactobacillus casei induces neutralizing antibodies in mice. Evaluation of new generation Salmonella enterica serovar Typhimurium vaccines with regulated delayed attenuation to induce immune responses against PspA. A sopB deletion mutation enhances the immunogenicity and protective efficacy of a heterologous antigen delivered by live attenuated Salmonella enterica vaccines. Mucosal vaccination with a codon-optimized hemagglutinin gene expressed by attenuated Salmonella elicits a protective immune response in chickens against highly pathogenic avian influenza. Construction and characterization of recombinant attenuated Salmonella typhimurium expressing the babA2/ureI fusion gene of Helicobacter pylori. Induction of immune responses in mice after oral immunization with recombinant Lactobacillus casei strains expressing enterotoxigenic Escherichia coli F41 fimbrial protein. Therapeutic efficacy of oral immunization with attenuated Salmonella typhimurium expressing Helicobacter pylori CagA, VacA and UreB fusion proteins in mice model. A comparison of immunogenicity and protective immunity against experimental plague by intranasal and/or combined with oral immunization of mice with attenuated Salmonella serovar Typhimurium expressing secreted Yersinia pestis F1 and V antigen. Systemic immune responses to oral administration of recombinant attenuated Salmonella typhimurium expressing Helicobacter pylori urease in mice. Attenuated Salmonella enterica serovar Typhi expressing urease effectively immunizes mice against Helicobacter pylori challenge as part of a heterologous mucosal priming-parenteral boosting vaccination regimen. Morphological and immunocytochemical analysis of Escherichia coli-specific surface antigens in wildtype strains and in recombinant Vibrio cholerae. Development of nonantibiotic-resistant, chromosomally based, constitutive and inducible expression systems for aroA-attenuated Salmonella enterica serovar Typhimurium. Nasal immunization with Lactococcus lactis expressing the pneumococcal protective protein A induces protective immunity in mice. Impact of vector-priming on the immunogenicity of a live recombinant Salmonella enterica serovar Typhi Ty21a vaccine expressing urease A and B from Helicobacter pylori in human volunteers. Lactobacillus acidophilus as a live vehicle for oral immunization against chicken anemia virus. Induction of protective immunity against microbial challenge by targeting antigens expressed by probiotic bacteria to mucosal dendritic cells. Dendritic cell targeting of Bacillus anthracis protective antigen expressed by Lactobacillus acidophilus protects mice from lethal challenge. A Salmonella enterica serovar Typhi vaccine expressing Yersinia pestis F1 antigen on its surface provides protection against plague in mice. A novel in vivo inducible expression system in Edwardsiella tarda for potential application in bacterial polyvalence vaccine. Oral immunization with attenuated Salmonella vaccine expressing Escherichia coli O157:H7 intimin gamma triggers both systemic and mucosal humoral immunity in mice. Induction of systemic and mucosal immune response and decrease in Streptococcus pneumoniae colonization by nasal inoculation of mice with recombinant lactic acid bacteria expressing pneumococcal surface antigen A. Expression of Streptococcus pneumoniae antigens, PsaA (pneumococcal surface antigen A) and PspA (pneumococcal surface protein A) by Lactobacillus casei. MyD88 signaling is not essential for induction of antigen-specific B cell responses but is indispensable for protection against Streptococcus pneumoniae infection following oral vaccination with attenuated Salmonella expressing PspA antigen. Effect of expression level on immune responses to recombinant oral Salmonella enterica serovar Typhimurium vaccines.
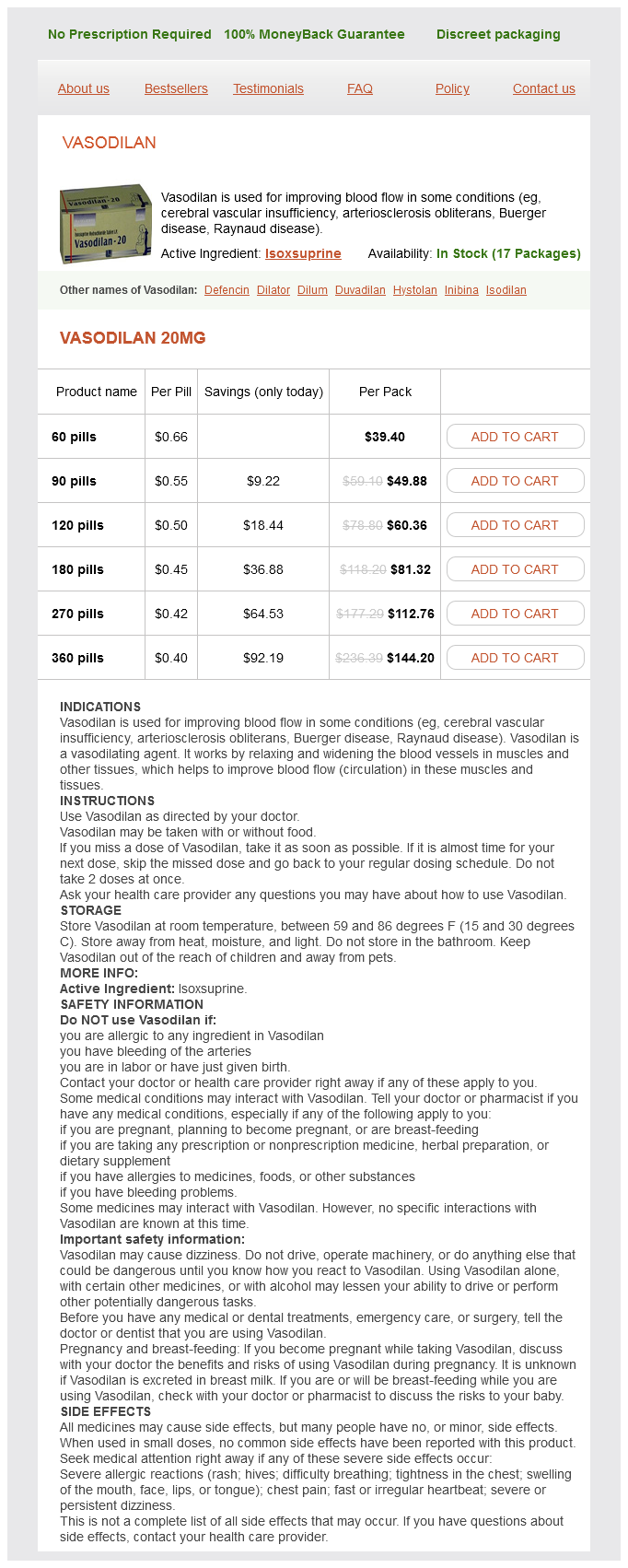
Vasodilan Dosage and Price
Vasodilan 20mg
- 60 pills - $39.40
- 90 pills - $49.88
- 120 pills - $60.36
- 180 pills - $81.32
- 270 pills - $112.76
- 360 pills - $144.20
The electrophoretic alpha-globulin pattern of serum in alpha-antitrypsin deficiency pulse pressure meaning cheap 20 mg vasodilan fast delivery. P2X7 receptor signaling in the pathogenesis of smoke-induced lung inflammation and emphysema. Origin, homeostasis and function of Langerhans cells and other langerin-expressing dendritic cells. Anti-tissue antibodies are related to lung function in chronic obstructive pulmonary disease. A novel insight into adaptive immunity in chronic obstructive pulmonary disease: B cell activating factor belonging to the tumor necrosis factor family. Antielastin B-cell and T-cell immunity in patients with chronic obstructive pulmonary disease. Evidence that Langerhans cells in adult pulmonary Langerhans cell histiocytosis are mature dendritic cells: importance of the cytokine microenvironment. Chapter 98 Mucosal Immunity in the Oral Cavity, Upper Respiratory Tract, and Adjacent Areas: An Overview Michael W. The reasons are quite simple: the mouth and its secretion, the saliva, are the most accessible components of the mucosal immune system and can be readily sampled without need for invasive procedures in persons of any age. Indeed, the first experimental demonstration that the common mucosal immune system existed in humans was accomplished by oral immunization with a suspension of Streptococcus mutans, revealing immunoglobulin (Ig) A antibody responses in saliva and tears but no serum antibodies (Czerkinsky et al. Immunity to oral infections, which include another highly prevalent condition, periodontal disease, continue to afford opportunities for investigating the mucosal immune system and its interface with systemic immunity (Chapter 102). Thus, comprehension of the immune regulatory mechanisms involved and how they are disrupted by periodontal pathogens will likely reveal parallels with other mucosal inflammatory conditions, such as inflammatory bowel disease. Although the precise contribution of the tonsils to the generation of mucosal immune responses and their dissemination to remote effector sites has been controversial, it is clear that these tissues are an active site of induction as well as expression of immune responses, with connections to the systemic and mucosal compartments of immunity. The cellular and molecular mechanisms operating in these tissues are extensively reviewed in Chapter 103. From the pharynx, it is but a short step to the nasal passages in one direction and to the middle ears via the Eustachian tubes in another, and both are sites of significant infectious pathology and immunopathology. For many years, the nose has been regarded by many immunologists as "the part of the lung that you can touch with your fingers. However, as explained in Chapter 100, we now realize that the nose is a distinct mucosal immune site from the lungs, in which there is a much greater effect of vasomotor tone and reflexes. Primary entry of antigens via the nose often leads to tolerance induction, characterized by the induction of regulatory T cells and production of IgA responses to antigens. Because the nose was considered a nonimmunogenic site, this led to the idea that drugs such as insulin could be administered via the nose, avoiding the generation of antibodies. However, it has become clear that the nose is a very active site of immune induction, even to harmless antigens such as insulin, and this route of administration of protein drugs has been virtually abandoned. We now realize in greater detail that immune defense of the nose consists of more than the sneezing reflex and the mucociliary blanket. Subsequently, effector T and B cells return to the nasal mucosa and control innate and adaptive immune responses. The seasonal and perennial forms of this disease are common causes of absenteeism from school and work and have great impact on the quality of life of those affected, even more than asthma. Allergic rhinitis is also a common comorbidity of asthma (80% of cases occur together), affecting the severity of asthma (von Mutius et al. Mouse models of asthma and rhinitis have clearly shown that allergic rhinitis influences the generation of asthma (Hellings et al. Chronic rhinosinusitis with or without polyps is well described in Chapter 100 and represents a highly interesting model of a mucosal disease. In nasal polyps, sometimes a predominance of eosinophils is seen, whereas sometimes neutrophilia is noticed. These distinct forms of the same polyp are influenced by genetics, colonization by Staphylococci, and by prior therapy. Chronic rhinosinusitis is also very often a comorbidity of severe corticosteroid-dependent asthma, particularly in female patients. In these patients, there might be a predominant role of type 2 innate lymphocytes, identifying this disease as one of the first in which such cells seem to play a predominant role. Relatively little is known or reported on the detailed immunology of the ear and Eustachian tube (Chapter 101). Part of the problem is that this organ is very inaccessible in humans and there are only sparse studies reported in animal models of disease. One of the most common diseases is serous otitis media, possibly a dysbiosis of the middle ear. Much is yet to be learned about the lymphoid drainage and precise immune cell types in the middle ear. Animal models for the precise study of the immune response in the ear are also greatly needed. We know a lot about the organogenesis of the ear, as well as the transcription factors involved, but we have no idea when and where the immune drainage of the ear develops. The eyes have been considered as a site of "immune privilege," implying that a different set of underlying principles operate at least within the interior of the eyeball. However, current understanding of immune regulation has put a different interpretation on the observations that led to this concept. Moreover, as discussed in Chapter 99, corneal antigen-presenting cells function in a similar manner as elsewhere, but a regulatory cytokine environment maintains tissue homeostasis. The lacrimal glands clearly represent another effector site of mucosal immunity where S-IgA production is abundant, along with high concentrations of potent innate defense factors.