General Information about Valtrex
Valtrex can additionally be generally prescribed for the remedy of genital herpes, which is a sexually transmitted infection caused by the herpes simplex virus (HSV). When taken throughout a herpes outbreak, it can help scale back the severity of symptoms and speed up the therapeutic course of. It may also be used as a suppressive therapy to prevent recurrent outbreaks and cut back the danger of transmission to sexual companions.
Valtrex is usually well-tolerated, with frequent side effects together with nausea, headache, and dizziness. In uncommon circumstances, it could cause more critical side effects such as confusion, decreased urine production, and allergic reactions. It is necessary to inform a physician if any of these unwanted effects are experienced.
Valtrex, also recognized by its generic name valacyclovir, is an antiviral drug that's used to deal with herpes zoster (shingles), genital herpes, and herpes cold sores on the face and lips. It belongs to a bunch of medication called nucleoside analogues, which work by interfering with the growth and spread of the herpes virus.
Herpes is a typical virus that impacts hundreds of thousands of people worldwide. It is a contagious an infection that can trigger painful blisters and sores in numerous elements of the body. While there isn't any remedy for herpes, there are medications that may help manage the symptoms and forestall outbreaks. One of those medicines is Valtrex.
Valtrex is available within the form of an oral pill, and it's typically taken twice a day for one to 10 days, relying on the condition being handled. The dosage may vary based on factors such because the severity of the an infection, age, and other medical circumstances.
In conclusion, Valtrex is a widely used antiviral drug that's efficient in treating shingles, genital herpes, and cold sores. It helps to reduce signs and velocity up the therapeutic process, providing relief to those affected by these conditions. If you may have been identified with any of these infections, consult your physician to see if Valtrex is a suitable remedy possibility for you.
It is price noting that Valtrex just isn't a treatment for herpes, and it doesn't forestall the transmission of the virus to others. Therefore, it is essential to apply protected intercourse and keep away from intimate contact during outbreaks to prevent passing the infection to a companion.
In treating shingles, Valtrex helps to reduce the severity and duration of the rash, in addition to alleviate the pain and itching associated with it. It is normally really helpful for people over 50 years old, as they're at a better risk of growing shingles as a end result of weakened immune methods. Despite being vaccinated towards chickenpox in childhood, the virus can reactivate within the body later in life, causing shingles.
In addition to shingles and genital herpes, Valtrex can additionally be efficient in treating recurrent herpes labialis (cold sores) on the face and lips. Cold sores are caused by the herpes simplex virus type 1 (HSV-1), they usually usually appear as small, fluid-filled blisters on or around the lips. Valtrex can help to scale back the pain and discomfort associated with cold sores and pace up the healing process.
Syphilis testing: similar to sarcoidosis hiv infection prevalence worldwide generic valtrex 500 mg amex, syphilis can cause any type of uveitis in the absence of characteristic systemic manifestations. Therefore, serologic testing should be performed on all patients with uveitis of unknown etiology. Medication history: certain medications such as bisphosphonates, moxifloxacin, and sulfonamides can cause uveitis. Mydriatic and cycloplegic agents are used to alleviate pain and prevent synechiae. Topical corticosteroids are the hallmark of therapy, but have limited efficacy in posterior disease. Periocular or intravitreal corticosteroids may be useful for more severe cases, or when posterior disease is prominent. When the above measures fail, or when disease onset is severe, systemic corticosteroids are indicated (usually started at a dose of 1 mg/kg/day). When systemic steroids are inadequate, not tolerated, or cannot be tapered, steroid-sparing immunosuppressive agents are required. In most cases, management strategies for uveitis parallel those of the systemic disease. Affects women in two thirds of cases, is bilateral at some point over the course of disease in 50% of cases, and is associated with a systemic autoimmune disorder in 30% of cases. Tends to have a good prognosis, typically resolving in 2 to 3 weeks without complications, but may recur at 1-month to 3-month intervals for several years in up to 60% of cases. Patients typically have severe, boring, and persistent pain (except with scleromalacia perforans), with associated erythema, photophobia, and tearing. Bilateral disease develops in 30% to 70% of cases, with recurrence rates of up to 70%. Associated with a systemic disease in 50% of cases, with frequency depending on the subtype (see below). Complications include keratitis, uveitis, glaucoma, cystoid macular edema, and exudative retinal detachment. Diffuse scleritis is the most benign form, with ocular complications occurring in 50% of cases, but only 18% experiencing a decrease in visual acuity. Approximately 60% of patients have an associated systemic disease, with rheumatoid arthritis being the most common. Nodular scleritis is characterized by local inflammation with a tender immobile nodule. Ocular complications occur in 50% of cases, with <10% experiencing decreased visual acuity. Approximately 45% of patients have an associated systemic disorder such as rheumatoid arthritis. Necrotizing scleritis is the most destructive form and can progress rapidly to scleral necrosis. Up to 95% of patients have an associated systemic disorder and ocular complications are common. Its presence may indicate increased activity of systemic vasculitis, and 45% of untreated patients will die from vasculitis complications within 5 years. Can be insidious when not associated with visible inflammation (scleromalacia perforans), and pain and globe perforation are rare in this setting. Posterior scleritis may be difficult to diagnose because redness may be absent (unless anterior involvement is also present), and pain and visual disturbance may be minimal. Associated with systemic disease in less than one third of patients when posterior involvement is isolated. The superficial inflammation of the loose vascular connective tissue overlying the sclera that characterizes episcleritis explains the historical and examination features that may distinguish it from scleritis. The significant pain associated with scleritis is the primary distinguishing feature. A blue/purple hue, rather than bright red discoloration, may be seen with scleritis; and the presence of avascular areas within the regions of vascular engorgement is highly suggestive of scleromalacia perforans. In episcleritis, application of phenylephrine results in rapid resolution of erythema. Episcleritis and scleritis can coexist, which must be remembered when interpreting these results. What systemic autoimmune/autoinflammatory diseases are associated with episcleritis? Joint inflammation may be "burnt out," and patients often have other extraarticular manifestations. What nonrheumatologic diseases should be considered in a patient with episcleritis or scleritis? A high index of suspicion must be maintained for infectious causes in the setting of the chronic immunosuppression typical of rheumatology patients. Oral and intravenous bisphosphonates, trauma, and malignancies (penetration by ocular adnexal lymphoproliferative lesions and intraocular tumors) are rare causes. If frequent or prolonged use of topical lubricants is required, preservative-free formulations should be used to prevent irritation. Topical corticosteroids are extremely effective and should be considered the next line of therapy. Systemic therapy is required for scleritis whether it is isolated or in the setting of systemic disease, and pain is often the best indicator of inflammation control. The selection of therapy is based on the subtype of the disease and any associated systemic features.
A randomized antiviral restriction factor transgenesis in the domestic cat cheap valtrex 1000 mg buy on-line, controlled, multicenter dose-response study, J Bone Joint Surg Am 89:1424, 2007. The most common benign joint neoplasms are tenosynovial giant cell tumors and synovial chondromatosis. A benign or malignant neoplasm of the joint should be considered in any patient with a nontraumatic hemarthrosis. Why should practicing physicians be concerned with tumors that affect the joints and synovium? Benign and malignant neoplasms affecting articular and periarticular structures may mimic inflammatory arthritis. Awareness of these conditions is crucial to prevent diagnostic delay and to avoid the initiation of ineffective and/or inappropriate therapy. A young adult presents with a solitary, painless mass adjacent to a finger joint that has been slowly enlarging. This benign condition, which occurs with a slightly increased predilection for females, is second only to the ganglion as a source of localized swelling in the hand and wrist. These nodular lesions usually occur in association with a tendon sheath (formerly called giant cell tumor of tendon sheath). Grossly, the synovium is red-brown to mottled orange-yellow and prolific with coarse villi, finer fronds, and diffuse nodularity resembling an Angora rug. Swelling and effusion accompanied by moderate discomfort, decreased range of motion, and increased warmth to palpation are typical. It tends not to be as darkly pigmented and has less villous proliferation than is seen in the diffuse form. Plain radiographs are usually nonspecific except for mild increased density of the soft tissue of the joint resulting from blood and hemosiderin deposits. The tumor may invade into bone causing cysts or scalloped erosive changes with sclerotic borders mimicking gout or tuberculosis. Nodules with sufficient hemosiderin appear dark on both T1-weighted and T2-weighted images. It is characterized by a dense cellular infiltrate composed of synovial cell hyperplasia with surface and subsynovial invasion of mitotically active cells with eosinophilic cytoplasm. Other invading cells are fibroblasts, lipidladen macrophages (xanthoma cells), hemosiderin-containing macrophages, and scattered, frequent, multinucleated giant cells. Surgical treatment with complete synovectomy is standard, either via open or arthroscopic approaches. Intraarticular installation of radioisotopes or low-dose external beam radiation are used in refractory cases. Synovial chondromatosis is characterized by the development of multiple foci of cartilaginous metaplasia (? These foci form nodules that may be invaded by blood vessels leading to endochondral ossification (termed osteochondromatosis). The chondral nodules are frequently released as free bodies (joint mice) into the joint space. It is almost always monoarticular affecting the knee (50%) more than hip, shoulder, ankle, elbow, or other joints. Clinically, there is an increasingly compromised range of motion with crepitus and often with unexpected locking. Synovial chondromatosis of the knee demonstrating multiple, calcified chondroid bodies. Although considered benign, this condition can result in extensive local joint destruction if left untreated. Synovial chondromatosis never metastasizes but may undergo malignant transformation into a chondrosarcoma (5% of cases). It is a highly malignant neoplasm and generally occurs in the lower extremities (70%) of young people. A slowly growing, often minimally symptomatic mass adjacent to the joint is the typical presentation. The histology of this tumor may be biphasic, in which epithelial cells arranged in clusters, tubules, and acini are interspersed in a spindle cell stroma; or monophasic, in which either the epithelial or spindle cells predominate. Other morphologic types are recognized, however, including mixed and hemangiopericytic. Behavioral features include calcifying, ossifying, and poorly differentiated types. Although this tumor is called synovial sarcoma, ultrastructural and immunohistochemical studies have implicated an epithelial origin. Treatment is an aggressive combination of radical surgery, radiation therapy, and chemotherapy. Prognosis depends, in large part, on tumor size at the time of discovery, age of patient (<age 25 years do better), and whether or not the tumor is poorly differentiated. The cause of death in progressive disease is usually as a result of extensive pulmonary metastasis. Other common sites of metastasis include regional lymph nodes, bones, skin, and brain. Five-Year Survival in Synovial Sarcoma All tumors Tumor < 5 cm Tumor > 10 cm 50% 86% 22% 16. Clear cell sarcoma is a rare highly malignant tumor of tendons, ligaments, and fascial aponeuroses. What is its association with a malignancy more commonly thought of as a skin cancer? There are multiple lines of evidence suggesting, rather convincingly, that clear cell sarcoma is a representation of malignant melanoma. Which primary malignant tumor of joints may be difficult to differentiate from the benign cartilaginous metaplasia of synovial chondromatosis?
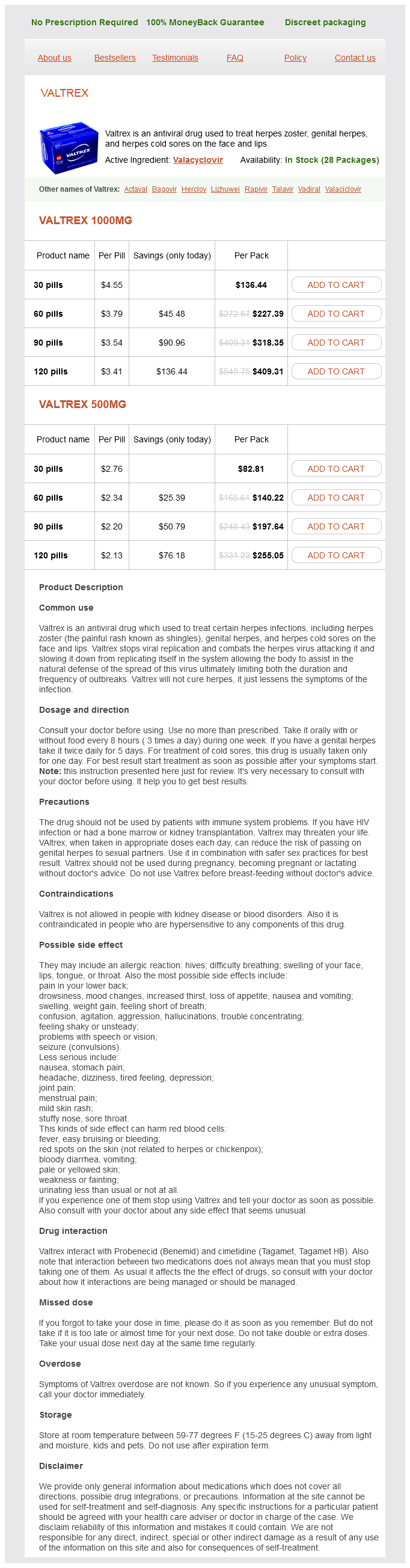
Valtrex Dosage and Price
Valtrex 1000mg
- 30 pills - $136.44
- 60 pills - $227.39
- 90 pills - $318.35
- 120 pills - $409.31
Valtrex 500mg
- 30 pills - $82.81
- 60 pills - $140.22
- 90 pills - $197.64
- 120 pills - $255.05
Most importantly hiv infection potential long term effects purchase 500 mg valtrex fast delivery, it can be used to exclude other forms of glomerular damage such as antiphospholipid antibody syndrome in a patient with hematuria or the presence of scar (nonactive disease) in a patient with persistent proteinuria. However, it has been emphasized that knowledge of the histological type of renal disease may add little clinically useful information over and above what is already known from clinical laboratory studies (urinalysis, protein excretion, and especially renal function studies). When interpreting histological findings in lupus nephritis, keep in mind that the renal biopsy is only a reflection of what is currently going on in the kidney and that change from one pathological class to another over time is well documented in patients with lupus nephritis and can occur in up to 40% of patients on therapy. Describe the key histological findings of the various pathological forms of lupus nephritis and their clinical implications. Minimal mesangial nephritis (class I) is characterized by immune deposits in the mesangium that are best seen by immunofluorescence and electron microscopy. Any sign of scar, crescents, or subendothelial deposits should suggest a higher class. Patients with mesangial nephritis usually demonstrate little clinical evidence of renal involvement, with normal or near-normal urinalysis and renal function, and rarely require any treatment for their renal disease. Immune complex deposits are often also present in the subendothelium and mesangial space. Patients with this pattern usually demonstrate proteinuria and hematuria, but severe (nephrotic range) proteinuria or progressive loss of renal function is less common than with diffuse disease. Focal proliferative nephritis should be viewed on a continuum with diffuse disease because the lesions are qualitatively similar but less extensive. Diffuse lupus nephritis is characterized by involvement of >50% of the glomeruli, with generalized hypercellularity of mesangial and endothelial cells. These changes may ultimately lead to obliteration of the capillary loops and sclerosis. Immunofluorescence microscopy demonstrates extensive deposition with IgG, IgM, IgA, C3, and C1q (full house pattern) in the deposits. Electron microscopy shows immune complex deposits in both subendothelial and subepithelial distributions, although subepithelial lesions should involve less than 50% of glomeruli. The pathology report should also describe the activity and chronicity of the lesion. Clinically, patients almost always have proteinuria (frequently nephrotic), cellular casts, and hematuria and, not infrequently, decreased renal function. Membranous lupus nephritis (class V) is characterized by the presence of granular global or segmental subepithelial immune deposits seen by immunofluorescence or electron microscopy. Clinically, patients who have pure membranous disease frequently have extensive proteinuria but only minimal hematuria or renal functional abnormalities. Membranous disease can also be observed as a transition stage after treatment for proliferative glomerulonephritis. What is the importance of evaluating biopsies for the extent of activity or chronicity? Historically on a renal biopsy report, pathologists would provide a calculated score to represent disease activity and disease chronicity. However, more recent literature shows mixed predictive value of using such a score and these calculations are no longer universally used. However, the identification of histological changes that represent chronicity and activity are thought to be helpful in contributing to the overall description of the renal biopsy. Evidence of fibrosis indicates chronic scarring disease, which may be less likely to respond to therapy Table 16-5). Which serological tests are most useful when following a patient with lupus nephritis? In addition, patients with active lupus nephritis have decreased levels of complement components. Thus, two alternative theories have been proposed to explain the pathogenic mechanisms of these antibodies. The activation of complement components through the classical pathway, with amplification by the alternative pathway, appears to be involved in the pathogenesis of glomerular damage. Complement activation may cause direct damage as well as recruit inflammatory cells to the sites of immune complexes. Which patients with severe lupus nephritis are more likely to progress to end-stage renal disease? Other features, which have been suggested, include lower socioeconomic status, poor compliance with medications, and comorbidities such as hypertension and diabetes. Failure to normalize the serum creatinine and decrease proteinuria to <1 g/day within 6 months of starting therapy is associated with a poorer long-term renal prognosis. Patients who fail to respond to both are candidates for rituximab or calcineurin inhibitors (cyclosporin, tacrolimus). Previously, cyclophosphamide was given as a daily oral dose or a prolonged (18 to 24 months) course of intravenous dosing. There is also accumulating data that low-dose cyclophosphamide followed by maintenance therapy is equivalent in efficacy to higher-dose regimens. Low-dose therapy ("Euro-Lupus" protocol) is associated with fewer serious infections and less infertility but has mostly been studied in white Europeans. Note that the risk of premature ovarian failure correlates with the cumulative dose of cyclophosphamide and the age of the patient. If creatinine clearance is less than 35 to 40 mL/min, then start the initial dose at 0. Which cytotoxic agents are most frequently used for maintenance therapy in treatment of lupus nephritis? Each of these drugs are given in association with a dose of prednisone required to control extrarenal manifestations, and prednisone is tapered over time. Calcineurin inhibitors (cyclosporin, tacrolimus) have also been used for maintenance therapy and in patients with refractory disease. A 30-year-old woman with severe nephritis and end-stage renal failure is referred for further evaluation and treatment.