General Information about Udenafil
Apart from its primary use in treating erectile dysfunction, udenafil is also being studied for its potential in different conditions such as pulmonary arterial hypertension (PAH) and premature ejaculation (PE). PAH is a rare but severe condition that causes high blood pressure within the lungs, resulting in difficulty in respiration. Udenafil has been discovered to enhance exercise capability and hemodynamic parameters in sufferers with PAH. In terms of PE, udenafil has been proven to improve intravaginal ejaculatory latency time and enhance ejaculatory management in men with primary PE.
In conclusion, udenafil is a promising treatment for the therapy of erectile dysfunction. It offers a safe and efficient possibility for men fighting this condition, with a quick onset of motion and longer duration of impact. It also has potential benefits in different circumstances, such as PAH and PE, making it a well-studied and versatile treatment within the subject of urology. However, it is essential to seek the advice of with a health care provider before starting treatment to make sure its suitability and security for particular person use.
Udenafil, additionally known by its brand name Zudena, is a medication primarily used to deal with erectile dysfunction (ED) in males. It is a potent and selective phosphodiesterase sort 5 (PDE5) inhibitor and has been proven to be efficient in improving sexual operate and enhancing sexual satisfaction.
Zudena is out there in pill type, with a really helpful starting dose of 100mg, to be taken approximately 30 minutes earlier than sexual activity. Dosage adjustments could additionally be needed primarily based on a person's response and tolerance to the drug. It is crucial to notice that udenafil doesn't trigger spontaneous erections; sexual stimulation continues to be needed for the medicine to be effective.
Udenafil works by inhibiting the PDE5 enzyme, which is responsible for breaking down cGMP, a chemical that helps relax the graceful muscular tissues within the penis. By blocking PDE5, udenafil allows increased blood flow into the penis, resulting in a firm and long-lasting erection. The drug has a sooner onset of motion and an extended duration of motion compared to other PDE5 inhibitors, making it a preferred alternative amongst males with ED.
Erectile dysfunction, also recognized as impotence, is a very common condition that affects tens of millions of males worldwide. It is characterised by the shortcoming to achieve or maintain an erection adequate for sexual activity. ED can have a significant impression on a person's vanity, mental well being, and relationships. It can be a warning signal of underlying well being conditions like diabetes, heart illness, or hypertension.
Like any treatment, udenafil may work together with sure drugs, together with nitrates and alpha-blockers, which are sometimes prescribed for heart conditions. It is essential to tell a healthcare professional of all medicines being taken earlier than starting udenafil. It just isn't really helpful to take the drug with alcohol as it may enhance the likelihood of unwanted effects.
One of the main advantages of udenafil is its security and tolerability profile. In numerous scientific trials, it has been proven to have a low incidence of opposed results corresponding to headache, flushing, and nasal congestion, that are widespread with different PDE5 inhibitors. Udenafil has also been found to be well-tolerated in patients with underlying medical circumstances, similar to diabetes and hypertension. However, caution must be exercised in sufferers with extreme liver or kidney impairment.
Rifampicin is now not recommended in combination with nevirapine (Panel on Antiretroviral Guidelines erectile dysfunction ka desi ilaj buy generic udenafil 100 mg on-line, 2016), etravirine, or rilpivirine. Rifampicin causes dramatic reductions in protease inhibitor levels, and the coadministration of rifampicin and protease inhibitors (with or without ritonavir boosting) is not recommended. Additional ritonovir does not overcome this interaction and increases hepatotoxicity (Panel on Antiretroviral Guidelines, 2016). Dolutegravir at 50 mg twice daily given together with standard-dose rifampicin was well tolerated and resulted in dolutegravir concentrations similar to those of 50 mg of dolutegravir given once daily alone (Dooley et al. Severe reactions thought to be immune mediated are rare, each occurring in less than 0. Although the classification is not absolute, it can be useful in understanding the pathophysiology underlying particular reactions. The adverse events associated with intermittent administration are often because of the development of rifampicin-dependent antibodies that result in complementmediated cell damage. Cutaneous reactions A "cutaneous syndrome" may occur in patients receiving daily or intermittent rifampicin therapy and usually becomes apparent early in the course of treatment. It consists of flushing and/or itching of the skin with or without a rash, involving particularly the face and scalp; redness and watering of the eyes may also occur. Symptoms usually appear 23 hours after a rifampicin dose, are generally self-limiting, and only require symptomatic treatment (Girling and Fox, 1971; Aquinas et al. Pruritis with or without rash may occur in as many as 6% of patients, but is generally self-limited (Villarino et al. This reaction may not represent true hypersensitivity, and continued treatment with the drug may be possible. Skin rash is rarely a valid reason to permanently discontinue rifampicin; use of antihistamines, and if necessary, desensitization, can enable virtually all such patients to remain on rifampicin (Matz et al. Rifampicin has also been reported to exacerbate pre-existing pemphigus vulgaris (Miyagawa et al. Some adverse reactions can occur with either daily or intermittent therapy, while some occur only when the drug is given intermittently. Serious reactions are uncommon if the recommended dosage schedules for daily and intermittent therapy are followed. Adverse reactions associated with rifampicin have been separated into two groups: reactions that can arise during 6b. Hypersensitivity reactions More severe, true hypersensitivity reactions are uncommon, occurring in 0. On rare occasions, an acute shock-like state, probably due to anaphylaxis, has followed rifampicin administration (Nessi et al. Immediate-type hypersensitivity reactions have been documented by the presence of anti-rifampicin IgE antibodies and/or a urticarial response to skin testing (Martinez et al. Oral desensitization therapy has allowed some individuals with hypersensitivity 2388 Rifampicin (Rifampin) Table 126. Marked decrease in etravirine predicted based on data on the interaction with rifabutin. Increasing the dose to 300 mg twice daily or 400 mg twice daily still resulted in subtherapeutic atazanavir concentrations. Doubling the dose to 300/100 twice daily resulted in hepatotoxicity in healthy volunteers. The combination of darunavir/ritonavir and rifampicin has not been evaluated, but concentrations are expected to be decreased. The combination of saquinavir (1000 mg twice daily), ritonavir (100 mg twice daily), and rifampicin caused unacceptable rates of hepatotoxicity among healthy volunteers. In tuberculosis patients, 400/400 twice daily caused similar rates of hepatotoxicity. Marked decrease in elvitegravir and cobicistat concentrations predicted based on metabolic pathways of these drugs. Gastrointestinal adverse effects Gastrointestinal symptoms, including nausea, anorexia, and abdominal pain, have been reported. The incidence is variable, but symptoms are rarely severe enough to necessitate discontinuation of the drug (Aquinas et al. This elevation is thought to be the result of inhibition of bilirubin excretion rather than true hepatic toxicity, and to be of no clinical significance (Cohn, 1969). Many patients receiving rifampicin alone or in combination with other drugs develop elevations of serum transaminase levels, particularly during the first few weeks of therapy, but most of these are asymptomatic, and the transaminase levels return to normal whether rifampicin is stopped or not (Newman et al. Baron and Bell (1974) also demonstrated that transient biochemical liver disturbances were common during the early weeks of antituberculosis treatment, irrespective of whether rifampicin was in the regimen, and they did not imply serious toxicity. Spontaneous resolution of these abnormalities despite ongoing administration of the drug is common (Weidmer et al. The incidence of rifampicin-induced hepatitis is relatively low (Girling and Hitze, 1979) but has varied among different patient populations, with the highest rates reported among individuals with chronic liver disease or predisposing conditions, such as alcohol abuse or coadministration of other potentially hepatotoxic medications. A meta-analysis reported that the incidence of hepatitis among adults receiving rifampicin is more common when given in combination with isonaizid (2. More severe clinical hepatitis requiring discontinuation of rifamycin therapy that typically has a cholestatic pattern may also occur (Sanders, 1976; Steele et al. Occasional acute liver failure, necessitating liver transplantation, occurred in patients receiving combined rifampicin, isoniazid, and pyrazinamide therapy (Mitchell et al. No underlying liver 2390 Rifampicin (Rifampin) disease has been present in most subjects in whom hepatotoxicity has developed. The incidence of this complication is not known with certainty, but reported rates of hepatotoxicity range from 1. As a result of the unexpectedly high rate of hepatotoxicity, this combination is no longer recommended for the treatment of latent tuberculosis infection (Getahun et al.
Antibiotic susceptibility and phage typing of methicillin-resistant and -sensitive Staphylococcus aureus clinical isolates at three periods during 19911997 erectile dysfunction treatment with injection udenafil 100 mg purchase. Clinical efficacy of combination of rifampin and streptomycin for treatment of Mycobacterium ulcerans disease. Epidemiological survey of rifampicin resistance in clinic isolates of Brucella melitensis obtained from all regions of Turkey. Depression of colony formation by human thymus-derived lymphocytes with rifampin and other antimicrobial agents. Evaluation of rifampin and other antibiotics against Listeria monocytogenes in vitro and in vivo. Rifampicin-resistant and rifabutin-susceptible Mycobacterium tuberculosis strains: a breakpoint artefact Phagocytosis of Mycobacterium ulcerans in the course of rifampicin and streptomycin chemotherapy in Buruli ulcer lesions. Stability of isoniazid, rifampin and pyrazinamide in suspensions used for the treatment of tuberculosis in children. Emergence of rifampicin resistance in methicillin-resistant Staphylococcus aureus in tuberculosis wards. Antimicrobial susceptibility patterns and characterization of clinical isolates of Staphylococcus aureus in KwaZulu-Natal province, South Africa. Haemophilus influenzae type b resistant to ampicillin and chloramphenicol in an orphanage in Thailand. Equivalence of ceftriaxone and rifampicin in eliminating nasopharyngeal carriage of serogroup B Neisseria meningitidis. Colistin against colistin-onlysusceptible Acinetobacter baumannii-related infections: Monotherapy or combination therapy Controlled trial of intermittent regimens plus isoniazid for pulmonary tuberculosis in Singapore. Rifampin concentrations in cerebrospinal fluid of patients with tuberculous meningitis. Mutations outside the rifampicin resistance-determining region associated with rifampicin resistance in Mycobacterium tuberculosis. Treatment of human brucellosis: systematic review and meta-analysis of randomised controlled trials. Antimicrobial susceptibility of viridans group streptococcal blood isolates to eight antimicrobial agents. Mycobacterium terrae: case reports, literature review, and in vitro antibiotic susceptibility testing. In vitro susceptibilities of four Bartonella bacilliformis strains to 30 antibiotic compounds. Trimethoprimsulfamethoxazole prophylaxis and antibiotic nonsusceptibility in invasive pneumococcal disease. Doxycycline-rifampin versus doxycycline-streptomycin in treatment of human brucellosis due to Brucella melitensis. The molecular basis of resistance to isoniazid, rifampin, and pyrazinamide in Mycobacterium tuberculosis. Colistin and rifampicin combination in the treatment of ventilator-associated pneumonia caused by carbapenemresistant Acinetobacter baumannii. Prompt diagnosis and extraordinary survival from Naegleria fowleri meningitis: a rare case report. Phenotypic and genotypic characteristics of Neisseria meningitidis disease-causing strains in Argentina, 2010. Nationwide surveillance of resistance rates of Staphylococcus aureus clinical isolates from Greek hospitals, 20122013. In vitro interactions between amphotericin B and other antifungal agents and rifampin against Fusarium spp. Efficacy of 2- and 4-week rifampicin treatment on the Wolbachia of Onchocerca volvulus. Resistance to methicillin and other antibiotics in isolates of Staphylococcus aureus from blood and cerebrospinal fluid, England and Wales, 198995. Reduced release of pneumolysin by Streptococcus pneumoniae in vitro and in vivo after treatment with nonbacteriolytic antibiotics in comparison to ceftriaxone. Rifampicin-resistant meningococci causing invasive disease: detection of point mutations in the rpoB gene and molecular characterization of the strains. Detection of resistance to rifampicin and decreased susceptibility to penicillin in Neisseria meningitidis by real-time multiplex polymerase chain reaction assay. Combination and sequential antifungal therapy for invasive aspergillosis: review of published in vitro and in vivo interactions and 6281 clinical cases from 1966 to 2001. Primary amoebic meningoencephalitis: a report of two cases and antibiotic and immunologic studies. Prevention of infection in peripheral arterial reconstruction: A systematic review and meta-analysis. Safety of 2 months of rifampin and pyrazinamide for treatment of latent tuberculosis. Rapid spread of penicillin-resistant Streptococcus pneumoniae among high-risk hospital inpatients and the role of molecular typing in outbreak confirmation. Rifampicin+ceftriaxone versus vancomycin+ceftriaxone in the treatment of penicillin- and cephalosporin-resistant pneumococcal meningitis in an experimental rabbit model. Controlled clinical trial of a regimen of two durations for the treatment of isoniazid-resistant pulmonary tuberculosis. Staphylococcus aureus peritonitis complicates peritoneal dialysis: review of 245 consecutive cases. Multicenter study for defining the breakpoint for rifampin resistance in Neisseria meningitidis by rpoB sequencing.
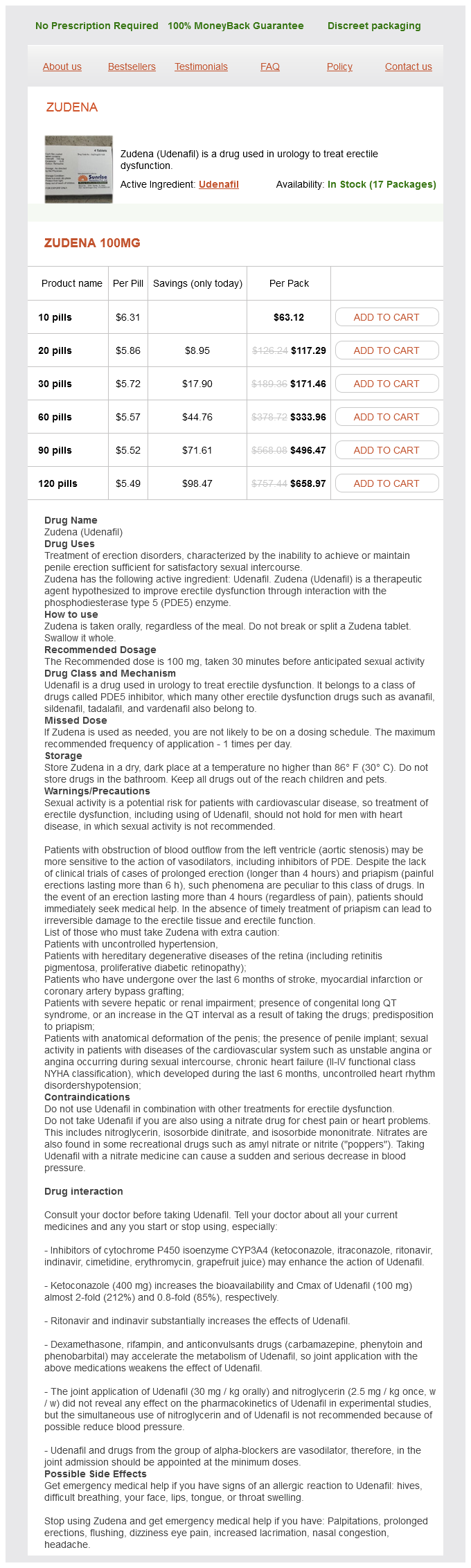
Udenafil Dosage and Price
Zudena 100mg
- 10 pills - $63.12
- 20 pills - $117.29
- 30 pills - $171.46
- 60 pills - $333.96
- 90 pills - $496.47
- 120 pills - $658.97
Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america erectile dysfunction at age 19 buy udenafil american express. Comparison of amphotericin B and N-D-ornithyl amphotericin B methyl ester in experimental cryptococcal meningitis and Candida albicans endocarditis with pyelonephritis. Treatment of experimental cryptococcal meningitis with amphotericin B, 5-fluorocytosine, and ketoconazole. Prophylactic intravenous amphotericin B in neutropenic autologous bone marrow transplant recipients. Treatment outcomes of surgery, antifungal therapy and immunotherapy in ocular and vascular human pythiosis: a retrospective study of 18 patients. Multicenter randomized trial of fluconazole versus amphotericin B for treatment of candidemia in non-neutropenic patients. Evaluation of Etest performed in Mueller-Hinton agar supplemented with glucose for antifungal susceptibility testing of clinical isolates of filamentous fungi. Combination therapy of experimental candidiasis, cryptococcosis, aspergillosis and wangiellosis in mice. Amphotericin B with and without itraconazole for invasive aspergillosis: a three-year retrospective study. A controlled trial of fluconazole or amphotericin B to prevent relapse of cryptococcal meningitis in patients with the acquired immunodeficiency syndrome. A randomized comparison of liposomal versus conventional amphotericin B for the treatment of pyrexia of unknown origin in neutropenic patients. Effects of immunomodulatory and organism-associated molecules on the permeability of an in vitro bloodbrain barrier model to amphotericin B and fluconazole. Chromoblastomycosis: an overview of clinical manifestations, diagnosis and treatment. Amphotericin B lipid complex or amphotericin B multiple-dose administration to rabbits with elevated plasma cholesterol levels: pharmacokinetics in plasma and blood, plasma lipoprotein levels, distribution in tissues, and renal toxicities. In vitro studies of Exserohilum rostratum with antifungal drugs and methylprednisolone. A randomized trial comparing fluconazole with amphotericin B for the treatment of candidemia in patients without neutropenia. Antifungal susceptibility testing of isolates from a randomized, multicenter trial of fluconazole versus amphotericin B as treatment of nonneutropenic patients with candidemia. Combination amphotericin B-rifampin therapy for pulmonary aspergillosis in a leukemic patient. Corneal and intra-ocular infection by Candida albicans treated with 5-fluorocytosine. The prophylactic use of low-dose amphotericin B in bone marrow transplant patients. Invasive pulmonary aspergillosis in a non-immunosuppressed patient: successful management with systemic amphotericin and flucytosine and inhaled amphotericin. Transient fungemia caused by an amphotericin B-resistant isolate of Candida haemulonii. Amphotericin B-induced severe hypertension in a young patient: case report and review of the literature. Epidemiology and outcome of Scedosporium prolificans infection, a review of 162 cases. Effects of double and triple combinations of antifungal drugs in a murine model of disseminated infection by Scedosporium prolificans. Posaconazole combined with amphotericin B, an effective therapy for a murine disseminated infection caused by Rhizopus oryzae. Amphotericin B formulations exert additive antifungal activity in combination with pulmonary alveolar macrophages and polymorphonuclear leukocytes against Aspergillus fumigatus. Combination therapy of disseminated Fusarium oxysporum infection with terbinafine and amphotericin B. Low-dose amphotericin B prophylaxis against invasive Aspergillus infections in allogeneic marrow transplantation. Aerosol delivery of amphotericin B desoxycholate (Fungizone) and liposomal amphotericin B (AmBisome): aerosol characteristics and in-vivo amphotericin B deposition in rats. Treatment of pulmonary aspergilloma in cystic fibrosis by percutaneous instillation of amphotericin B via indwelling catheter. Mechanisms of amphotericin B-induced decrease in glomerular filtration rate in rats. The enigma of candiduria: evolution of bladder irrigation with amphotericin B for management-from anecdote to dogma and a lesson from Machiavelli. Amphotericin B mediates killing in Cryptococcus neoformans through the induction of a strong oxidative burst. Direct vasoconstriction as a possible cause for amphotericin B-induced nephrotoxicity in rats. Aerosol amphotericin B is effective for prophylaxis and therapy in a rat model of pulmonary aspergillosis. Aerosolized amphotericin B inhalations as prophylaxis of invasive aspergillus infections during prolonged neutropenia: results of a prospective randomized multicenter trial. Amphotericin B tolerance: a characteristic of Candida parapsilosis not shared by other Candida species. In vitro susceptibility of mycelial and yeast forms of Penicillium marneffei to amphotericin B, fluconazole, 5-fluorocytosine and itraconazole.