General Information about Trimox
In abstract, Trimox is a commonly prescribed antibiotic that is used to deal with a variety of bacterial infections. It is very efficient in relieving symptoms and preventing additional complications. If you might be prescribed Trimox, it is essential to follow your healthcare supplier's instructions and full the total course of therapy to make sure a profitable restoration.
In addition to the above talked about makes use of, Trimox can also be typically prescribed in combination with another antibiotic known as clarithromycin to deal with abdomen ulcers caused by the bacteria Helicobacter pylori. These ulcers could be painful and might result in serious problems, so you will want to treat them promptly. The combination of Trimox and clarithromycin helps to get rid of the bacteria and promote healing of the ulcer.
The medicine works by interfering with the expansion of bacterial cell walls, thus preventing the micro organism from multiplying and inflicting additional infection. This makes it a highly effective treatment for bacterial infections.
It is important to notice that whereas Trimox is efficient against bacterial infections, it isn't effective in opposition to viral infections such as the widespread chilly or flu. It can be important to complete the full course of the treatment, even if symptoms improve, to make certain that the infection is totally eradicated and stop the event of antibiotic-resistant micro organism.
Another common use of Trimox is for the treatment of gonorrhea, a sexually transmitted infection (STI) brought on by the bacteria Neisseria gonorrhoeae. Gonorrhea can cause severe symptoms together with painful urination, discharge, and in some cases, infertility. Trimox is a generally used antibiotic for treating this an infection, and is often very efficient in clearing up the symptoms.
One of the commonest makes use of of Trimox is for treating ear infections. These are sometimes caused by micro organism in the center ear, which might lead to pain, inflammation, and even short-term listening to loss. Trimox helps to clear up the an infection, relieving signs and stopping additional issues.
Trimox can additionally be used to deal with pneumonia, a severe an infection of the lungs and respiratory system. Pneumonia may be attributable to a big selection of bacteria, and might result in symptoms such as fever, coughing, and issue breathing. Trimox is commonly used at the facet of other antibiotics to effectively deal with pneumonia and prevent it from worsening.
In addition to ear infections, Trimox can be prescribed for urinary tract infections (UTIs) corresponding to bladder an infection. UTIs are mostly attributable to micro organism entering the urinary tract, which can trigger painful urination, frequent urination, and a powerful urge to urinate. Trimox is an effective treatment for most of these infections, usually providing relief within a couple of days.
Trimox, also identified by its generic name amoxicillin, is a extensively used antibiotic that belongs to the penicillin household. It is used to treat quite a lot of infections caused by bacteria, together with ear infections, bladder infections, pneumonia, gonorrhea, and certain types of stomach ulcers.
Trimox is generally well-tolerated by sufferers, although some might expertise mild side effects such as nausea, diarrhea, and stomach upset. These unwanted aspect effects are normally momentary and subside because the body adjusts to the medicine.
For example infection vs intoxication purchase 250 mg trimox visa, a patient who complains about the sound of the voice may in fact have a normal voice but actually have severe dysarthria and hypernasality secondary to amyotrophic lateral sclerosis. The site of the lesion associated with the neurologic disorder will result in characteristic physical findings and facilitate establishment of a correct diagnosis (Table 401-3). In dystonia (Chapter 382), spasmodic dysphonia fluctuates moment to moment and day to day. Adductor spasms of the vocal folds produce strained, strangled vocal quality with pitch breaks. Successful management depends on early detection by a careful examination of the entire upper aerodigestive tract, biopsy with histopathologic examination, and aggressive treatment based on the clinical stage and site of the lesion. Laryngeal paralysis most often is manifested as a unilateral paralysis as a result of a mediastinal tumor; surgical trauma during thyroid, carotid, or anterior cervical spine surgery; blunt or penetrating trauma; aortic aneurysm; progressive neurologic disease; or viral or idiopathic causes. Unilateral vocal fold paralysis with a favorable prognosis occurs after blunt trauma, endotracheal intubation, idiopathic vocal fold paralysis, and paralysis associated with viral pathogens (Ramsay Hunt syndrome). In this setting, the severity of aspiration, dysphonia, and electromyographic findings can be used to determine the choice of procedure and timing of intervention. Temporary medialization with collagen injection is warranted in patients with unilateral paralysis and a good prognosis. Patients who have poor prognosis for recovery include those with injury after complete section of the nerve during a surgical resection of tumor, invasion of cranial nerves by a tumor, paralysis associated with thoracic aneurysm, or paralysis due to progressive neurologic disorders. In patients with a low likelihood of recovery, permanent medialization of the paralyzed vocal fold is warranted. Bilateral vocal fold motion impairment, which is less common, has the same causes. Its management is most often directed toward improving the airway because the predominant symptom is airway obstruction. Tonsillectomy versus watchful waiting for recurrent throat infection: a systematic review. Metronidazole in conjunction with penicillin neither prevents recurrence nor enhances recovery from peritonsillar abscess when compared with penicillin alone: a prospective, double-blind, randomized, placebo-controlled trial. Effect of oral dexamethasone without immediate antibiotics vs placebo on acute sore throat in adults: a randomized clinical trial. Tonsillectomy or adenotonsillectomy versus non-surgical treatment for chronic/recurrent acute tonsillitis. Appropriate antibiotic use for acute respiratory tract infection in adults: advice for high-value care from the American College of Physicians and the Centers for Disease Control and Prevention. Rapid antigen detection test for group A streptococcus in children with pharyngitis. Comparison of medical therapy alone to medical therapy with surgical treatment of peritonsillar abscess. Presentation and outcomes of localized immunoglobulin light chain amyloidosis: the Mayo Clinic experience. A study of clinicopathological profile of patients of hoarseness of voice presenting to tertiary care hospital. The consultant can help avoid unnecessary and repetitive preoperative testing that is costly in the aggregate with essentially no benefit. Surgeons typically request a postoperative medical consultation when a complication has developed that is beyond their area of expertise (Chapter 405). These problems are commonly urgent, so the goal is expeditious consultation and prompt intervention. Management of these problems does not usually differ from management in nonoperative settings. Another reason for a postoperative consultation is to obtain assistance in post-hospitalization care or to facilitate seamless discharge planning. Consultants should aid in the transition to the outpatient or long-term care setting by taking primary or consultative roles as appropriate. Cross-consultations between medical subspecialists or between a subspecialist and a generalist, in either direction, are quintessential examples of collaboration. Shared care, which is defined as truly joint participation of primary care physicians and specialist physicians in the delivery of care for patients with chronic conditions, can improve outcomes for hypertension, depression, and other medical conditions. A1 For example, a randomized trial of shared care for patients with hypertension and chronic kidney disease demonstrated lower blood pressures and better use of lipid-lowering drugs in the shared care group. Infectious disease consultation also is associated with better adherence to quality measures, reduced in-hospital mortality,4 with bacteremia and other infectious diseases. This transfer of responsibility is not dissimilar to that occurring when a patient is submitted to the care of a subspecialist for a procedure such as cardiac catheterization or gastrointestinal endoscopy. Similar issues also arise when a critically ill patient with a condition such as a complicated myocardial infarction (Chapter 64) or shock (Chapters 98, 99, and 100) is managed principally by a critical care medical specialist and is then expected to return to the care of the primary physician after hospital discharge. However, a key difference is that the inpatient hospitalist physician, unlike the consulting subspecialist, will not typically have an ongoing comanagement role. Because of the higher risk for discontinuity, effective communication at the time of hospitalization, whenever key issues arise during hospitalization, and at the time of discharge is even more important in the inpatient hospitalist model than in the other settings in which subspecialists may take on more of a comanagement role. Effective and comprehensive hand-offs at the time of hospital discharge improve continuity and reduce the potential for errors and medicolegal liability. A recent quality improvement initiative has been the development of rapid response teams.
The flashes antibiotics for uti list order trimox paypal, which may be more pronounced in the dark and with rapid eye movement, may be associated with the sudden onset of floaters, which can indicate debris or blood in the vitreous cavity. Because a tear in the retina can lead to a retinal detachment, urgent consultation with an ophthalmologist is required. Flashing light with a migraine (Chapter 370) is described as scintillations or zigzagging lights that march across the visual field for a few minutes or as long as 30 minutes, sometimes associated with transient visual field loss. Floaters, which are caused by small aggregates or opacities in the vitreous cavity, result from the normal aging of the vitreous. The acute onset of vitreous floaters may be associated with uveitis or with the sudden onset of bleeding in the vitreous cavity owing to diabetes or sickle cell anemia. Acute floaters, however, particularly if associated with flashing lights, may indicate a posterior vitreous detachment and/or a retinal tear with an impending retinal detachment. Photophobia, particularly if associated with eye pain, redness, and decreased vision, is a symptom of intraocular inflammation (uveitis) from trauma or other causes. Patients with cataracts commonly see halos around lights, particularly when driving at night. Episodic decreased vision, redness, and halos around lights may be symptoms of impending angle-closure glaucoma owing to increased intraocular pressure with resulting corneal edema and loss of corneal clarity. A foreign body sensation is commonly caused by ocular surface diseases such as dry eye syndrome (see later). Most corneal abrasions cause severe pain, but minor corneal abrasions may be associated with a foreign body sensation rather than the severe pain. An arc welder burn causes a punctate corneal keratopathy, and foreign body sensation may be a prominent symptom. Tearing can occur because of the overproduction of tears or impairment of tear drainage. Any abnormalities in upper or lower lid laxity, position, or closure can impair the lacrimal pump system. All orbital processes can affect orbital cranial nerves, with associated diplopia or optic neuropathy. Idiopathic orbital inflammation can cause acute, usually unilateral proptosis, with severe pain, particularly with eye movement, and often with decreased vision. An optic nerve tumor causes chronic, unilateral proptosis associated with a slow onset of visual field loss. Acute cellulitis can be associated with unilateral proptosis, severe redness, and moderate to severe pain, commonly with sinusitis and an elevated white blood cell count. Causes include Horner syndrome, associated with ptosis on the same side; the bilaterally small, poorly reacting pupils of tertiary syphilis (Argyll Robertson pupils), which accommodate with normal constriction to a near object; miotic drops. Any -adrenergic or anticholinergic agent placed into the eye can cause a large pupil. With eye trauma, the iris sphincter muscle can be damaged, and an abnormally large pupil can result. Tears in the iris sphincter can sometimes be appreciated on slit lamp examination. Third nerve palsy may cause a dilated pupil associated with ptosis and decreased elevation, depression, and medial eye movement. Recent eye surgery, uveitis, an acute angle-closure glaucoma attack, and traumatic iritis can cause a large pupil. Leukocoria (white pupil) in a young child is a critically important because it may be a sign of retinoblastoma. Some of the more common nonretinoblastoma conditions presenting with leukocoria (Table 395-5) include cataracts, retinal detachment, persistent fetal vasculature (a developmental anomaly of drainage system owing to age, inflammation, infection, or neoplasm can prevent appropriate tear drainage. Finally, ocular surface irritants such as trichiatic eyelashes touching the cornea can stimulate excessive tear production. Occasional twitching of the lids usually is associated with stress or adrenergic stimulation. Benign essential blepharospasm is severe spasm of the lids leading to functional impairment. Any ocular inflammation, including corneal ulcers, angle-closure glaucoma, endophthalmitis, and uveitis, can be associated with secondary conjunctival hyperemia. Conjunctivitis usually involves the entire conjunctiva, is associated with a discharge, and usually is not associated with pain (see Table 395-4). However, it also can be caused by a third nerve palsy, Horner syndrome, myasthenia gravis (Chapter 394), or other neurologic conditions. With myasthenia gravis (Chapter 394), other typical features of muscle weakness and fatigability are usually present or can be elicited. Non-neurologic causes of ptosis include age-related dehiscence of the levator muscle. Proptosis, or a prominent globe, can be a manifestation of thyroid eye disease, which in turn is associated with thyroid abnormalities, especially Graves disease (Chapter 213). Diseases of the Visual system 2523 that respond to warm compresses and topical antibiotics. An ophthalmologist may perform incision and drainage if symptoms do not improve within 48 hours. Rosacea (Chapter 410) is the most common associated cutaneous condition, and Staphylococcus aureus is the most common infectious agent. If untreated, blepharitis becomes chronic and may lead to corneal and conjunctival inflammation (blepharoconjunctivitis). Effective supportive care for blepharitis includes warm compresses and maintenance of good lid hygiene. In seborrheic blepharitis, exfoliated keratinous debris accumulates along the eyelid margin, particularly at the follicles of the eyelashes, and irritates the conjunctiva.
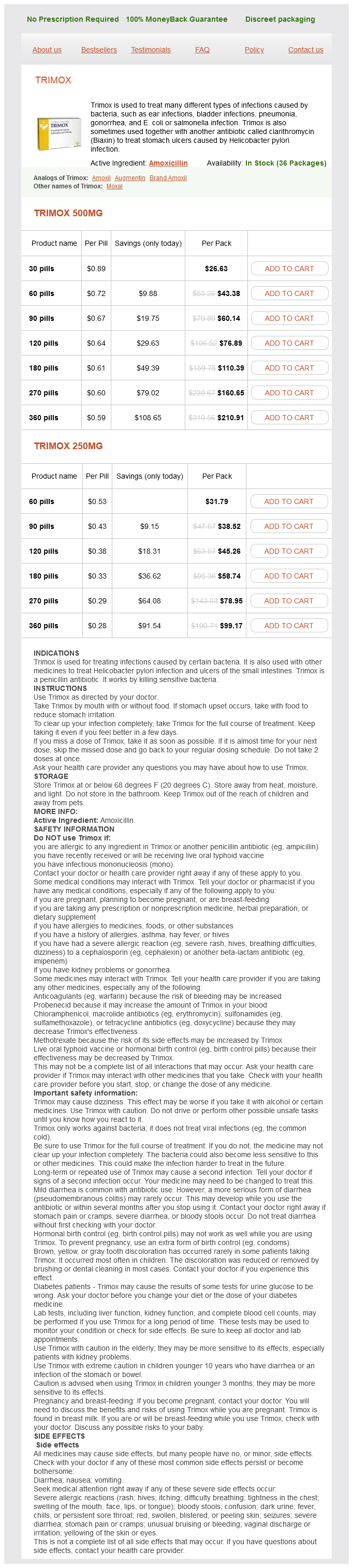
Trimox Dosage and Price
Trimox 500mg
- 30 pills - $26.63
- 60 pills - $43.38
- 90 pills - $60.14
- 120 pills - $76.89
- 180 pills - $110.39
- 270 pills - $160.65
- 360 pills - $210.91
Trimox 250mg
- 60 pills - $31.79
- 90 pills - $38.52
- 120 pills - $45.26
- 180 pills - $58.74
- 270 pills - $78.95
- 360 pills - $99.17
Modifiable risk factors include cigarette smoking infection pictures purchase trimox 250 mg with mastercard, heavy alcohol use, arterial hypertension, and use of sympathomimetic agents such as cocaine and phenylpropanolamine. In 80% of cases, the cause of subarachnoid hemorrhage is rupture of an intracranial saccular or berry aneurysm. Justin Zivin) Data are from 580 patients treated at Columbia University Medical Center. The most common cause of intracerebral hemorrhage is rupture of the small penetrated arteries within the brain parenchyma, whereas subarachnoid hemorrhage is caused by ruptured vessels on the surface of the brain, especially a congenital berry aneurysm. Subarachnoid hemorrhage classically presents with an extremely severe headache followed by a stiff neck, nausea, vomiting, and often loss of consciousness. Treatment for ruptured berry aneurysm is either surgical clipping or endovascular coiling. Treatment focuses on control of blood pressure and cerebral edema, compulsive intensive management to prevent complications, and rapid reversal of any underlying anti-coagulation. Brain vascular malformations can cause space-occupying symptoms or bleed into the intracerebral, intraventricular, or subarachnoid spaces. For patients who survive the acute episode, options include embolization, surgical resection, or radiationinduced thrombosis. Thick subarachnoid hemorrhage is defined as completely filling at least one cistern or fissure. Effect of cisternal and ventricular blood on risk of delayed cerebral ischemia after subarachnoid hemorrhage: the Fisher scale revisited. The cumulative risk of rebleeding in untreated patients is 20% at 2 weeks and 30% at 1 month. Poor clinical grade and larger size aneurysms are the strongest risk factors for in-hospital rebleeding. Delayed cerebral ischemia from vasospasm accounts for a large proportion of morbidity and mortality after subarachnoid hemorrhage. Progressive arterial narrowing develops in approximately 70% of patients, but delayed ischemic deficits develop in only 20 to 30%. The most important risk factor for symptomatic vasospasm is thick cisternal or intraventricular clot, which can be graded using the Modified Fisher scale (Table 380-2). Initial misdiagnosis of subarachnoid hemorrhage occurs in approximately 15% of patients, especially patients with the mildest symptoms. Approximately 40% of misdiagnosed patients experience subsequent neurologic deterioration, which is associated with increased morbidity and mortality, owing to rebleeding, hydrocephalus, or vasospasm before reaching medical attention. Ottawa Subarachnoid Hemorrhage Rule* Patients who are 15 years old and have a new severe atraumatic headache with maximum intensity within 1 hour. Subarachnoid hemorrhage can be differentiated from a traumatic tap by a xanthochromic (yellow-tinged) appearance of the supernatant fluid after centrifugation. The combined finding of less than 2000 red blood cells/µL and the absence of xanthochromia excludes the diagnosis of aneurysmal subarachnoid hemorrhage with a sensitivity of close to 100% and a specificity of 91%. Red blood cells and xanthochromia disappear in about 2 weeks, unless hemorrhage recurs. In approximately 20% of cases of subarachnoid hemorrhage, the initial angiogram is negative. In half of subarachnoid hemorrhages in which an aneurysm is not identified, the blood has a focal "perimesencephalic" distribution around the midbrain or anterior to the pons. Patients are neurologically intact, there is no risk of rebleeding or symptomatic vasospasm, and full recovery is the rule. In the remainder of cases of nonaneurysmal subarachnoid hemorrhage (Table 380-3), the bleeding source is usually a thin-walled arterial "blister" that is not amenable to surgical clipping or endovascular coiling. The daily percentage probability for the development of symptomatic vasospasm (blue line) or rebleeding (orange line) after subarachnoid hemorrhage. A, Diffuse thick subarachnoid hemorrhage is seen in the anterior interhemispheric and bilateral sylvian fissures and the quadrageminal cistern. B, Perimesencephalic subarachnoid hemorrhage; only a small focus of blood in the interpeduncular cistern is identified. Vasospasm Symptomatic vasospasm usually involves a decrease in level of consciousness, hemiparesis, or both. Vasospasm, local thrombosis, or poor technique can lead to a false-negative angiogram. For this reason, patients with a high clinical suspicion but an initially negative angiogram should have a follow-up study 1 to 2 weeks later; an aneurysm will be demonstrated in about 5% of these cases. Susceptibility-weighted imaging may be useful for documenting a completely thrombosed aneurysm in selected patients who have subarachnoid hemorrhage but a negative angiogram. Laboratory Testing In the emergency department, the immediate concern in high-risk patients is reducing intracranial pressure and preventing secondary cerebral hypoxicischemic injury. Patients with impaired ability to protect the airway should be intubated, given supplemental oxygen as needed, and treated aggressively with fluids and vasopressors to maintain a mean arterial pressure of 90 mm Hg (Table 380-3). Stuporous or comatose patients with extensive subarachnoid blood, intraventricular hemorrhage, acute obstructive hydrocephalus, or global cerebral edema should be empirically treated for intracranial hypertension with 1. Further doses of bolus osmotherapy should be directed at reducing intracranial pressure to less than 20 mm Hg. After subarachnoid hemorrhage, brain edema may be focal (usually related to a space-occupying hematoma) or global (an ominous pattern that implies severe primary brain injury and a poor prognosis). Cerebral Edema Definitive Surgery Complete obliteration of a ruptured berry aneurysm by either surgical clipping or endovascular coiling is the definitive treatment for prevention of rebleeding and should be performed as an emergency procedure. The only exception to this rule is in patients who are Hunt and Hess grade 5 and who have an extremely poor neurologic prognosis.