General Information about Terbinafine
Tinea versicolor, also referred to as pityriasis versicolor, is a skin infection that is caused by the yeast Malassezia furfur. This fungus is naturally found on wholesome skin, but in some circumstances, it might possibly overgrow and trigger discolored patches on the pores and skin. These patches can be lighter or darker than the surrounding skin and may be accompanied by gentle itching. Tinea versicolor is more frequent in warm and humid climates and may have an result on folks of any age, however is most commonly seen in adolescents and younger adults.
Terbinafine is mostly well-tolerated, and most people expertise few unwanted side effects. The most common unwanted side effects that have been reported include rash, itching, and gastrointestinal issues corresponding to nausea and diarrhea. Rarely, more critical unwanted side effects such as liver damage have been reported, so it may be very important follow the prescribed dosage and monitor any adjustments in your well being while taking terbinafine.
In conclusion, terbinafine is an effective medication for treating fungal infections, notably tinea versicolor. With its capability to inhibit the expansion of fungi and clear up skin infections, it has turn out to be a well-liked choice for both docs and patients. However, it's important to make use of this treatment as directed by a healthcare skilled and to be aware of any potential unwanted aspect effects. If you're experiencing symptoms of a fungal an infection, consult along with your physician to find out if terbinafine will be the right remedy possibility for you.
Terbinafine, marketed under the model name Lamisil, is an anti-fungal antibiotic that is commonly used to deal with fungal infections. It is primarily used to deal with tinea versicolor, a common pores and skin infection attributable to yeast, but may also be efficient against different kinds of fungal infections.
Terbinafine works by inhibiting the expansion of the fungus responsible for the infection. It does this by interfering with the production of ergosterol, a vital part of fungal cell membranes. Without ergosterol, the fungal cells are weakened and ultimately die, allowing the an infection to clear up.
In addition to treating tinea versicolor, terbinafine has also been found to be effective in treating different types of fungal infections similar to athlete's foot, jock itch, and ringworm. These infections occur when fungi invade the top layer of the pores and skin, causing it to turn out to be purple, itchy, and infected. By destroying the fungal cells, terbinafine might help to clear up these infections and provide relief from uncomfortable signs.
Lamisil is out there as each an oral medication and a topical cream. The oral kind is often prescribed for tinea versicolor, as it can effectively reach the deeper layers of the pores and skin the place the fungus may be current. It is taken once a day for a interval of two to four weeks, depending on the severity of the an infection. The topical cream is usually prescribed for milder instances or as a upkeep treatment to prevent future outbreaks. It is utilized directly to the affected areas a couple of times a day, depending on the instructions supplied by the physician.
It is important to note that while terbinafine is effective against fungal infections, it doesn't have any effect on bacterial or viral infections. Therefore, it shouldn't be used to deal with circumstances corresponding to colds or the flu. It can be not recommended to be used in pregnant or breastfeeding ladies, as the results on the unborn youngster are not totally understood.
Sometimes antifungal cream prescription cheap terbinafine 250 mg with amex, however, they burst into the tube or into the peritoneal cavity or a neighboring organ, such as the rectum or the bladder. Gradually, the follicular components and the specific ovarian stroma are completely destroyed in such ovaries, and the thick wall of the ovarian abscess consists merely of callous connective tissue which is poor in blood vessels and is infiltrated by leukocytes, lymphocytes, and plasma cells, which are accumulated in the inner, granulating lining of the abscess wall. Follicular and corpus luteum abscesses more often perforate into the tube than do interstitial ovarian abscesses. They may heal after discharging their content into the tube or may be transformed into tuboovarian abscesses, with progressive destruction of the ovarian parenchyma. Ovarian and tuboovarian abscesses have little tendency to spontaneous healing because of the thickness of their walls. However, intravenous administration of broad-spectrum antibiotics may result in resolution of the infection. They can be emptied either from the posterior vaginal fornix or from the abdomen if they are large, and can be reached in this way without exposing the free peritoneal cavity to contamination with the purulent content of the abscess. A definite cure can, however, be achieved only by complete removal of the diseased adnexa, usually in connection with the uterus. In rare instances, a tuboovarian abscess may finally change into a tuboovarian cyst. Fully developed abscess Ovary Large tuboovarian cyst Cyst Uterus Fallopian tube times also some red blood cells and leukocytes. As a rule, the tuboovarian cyst is a benign structure, changing very little in the course of time. Tuberculosis is a frequent cause of chronic pelvic inflammatory disease and infertility in other parts of the world and may be encountered in immigrants, especially those from Asia, the Middle East, and Latin America. Both tubes almost always are involved in the tuberculous disease, whereas the uterus is affected in slightly more than 50%. As a rule, the infection is carried to the tubes by the hematogenous route from a primary focus in the lung or the hilar lymph nodes. Pelvic tuberculosis may be produced by either Mycobacterium tuberculosis or Mycobacterium bovis. However, in the majority of cases, it is impossible to determine whether the infection has spread from the peritoneum to the tube or from the tube to the peritoneum. The possibility of an infection of the tubes by intracavitary or lymphatic ascent of tubercle bacilli introduced into the vagina by coitus with a tuberculous male cannot be denied. Changes in the fallopian tube as a result of an infection with tubercle varies to a great extent. In more advanced cases of tuberculous endosalpingitis, the miliary nodules coalesce to form an exudate that also infiltrates the outer layers of the tube, causing marked thickening of the tubal wall. Because the tuberculous process occurs in separate foci and not diffusely, the tube appears nodular ("rosary" form), with increased sinuosity. In more favorable cases, the granulation tissue may become fibrotic, shrunken, and calcified. Note the miliary nodules and the fibrous adhesions sometimes request medical advice only because of sterility. The course of the disease becomes stormy if diffuse peritonitis intervenes or if a caseous pyosalpinx becomes secondarily infected by pyogenic bacteria. It consists of glandular ramified projections of the mucosa into the thickened tubal wall. They may be epithelial in nature such as papillomas, adenomas, carcinomas, and chorioepitheliomas, or they may be mesenchymal tumors such as fibromas, myomas, lipomas, chondromas, osteomas, and angiomas. Endosalpingosis occupies an intermediary position between inflammatory and neoplastic diseases. Foci of endometrial tissue are commonly found in the endosalpinx and are particularly frequent in the interstitial portion of the tube. In the interstitial and the adjoining isthmic region, they may produce a nodular thickening of the tube similar to that caused by chronic inflammatory irritation. In primary tubal carcinoma, the tube forms an elastic or firm, sausage- or pear-shaped tumor, which is usually adherent to its surroundings and filled with papillomatous, cauliflowerlike or villous, friable masses of grayish-red or grayishwhite neoplastic tissue. Extension of the carcinoma takes place via the lymph or bloodstream, along the peritoneal surface, or by contiguity. The ovaries and the uterus are frequently involved in the disease, and invasion of the iliac and lumbar lymph nodes is common. Burning or darting pains in the lower abdomen, hemorrhages, and clear or turbid, serous or serosanguineous discharge may be present. Approximately 50% of patients with fallopian tube cancer present with vaginal bleeding. Abnormal cervical cytology is occasionally present, with a reported range of 10% to 40%. The former, called paraovarian or epoöphoron cysts, may be small and may represent simple retention cysts; some, however, are true blastomas, which grow continuously and may finally attain an enormous size. Exceptionally, the cyst is fixed to its surroundings by dense inflammatory adhesions or, instead of expanding upward toward the peritoneal cavity, it may grow downward toward the pelvic floor or into the mesosigmoid. As a rule, the tube encircles the tumor by running around it from the anterior to the posterior surface of the cyst, where it reaches the flattened and elongated ovary with its fimbriated end. Paraovarian cysts do not have true pedicles, but if they continue to project into the peritoneal cavity, some kind of pedicle develops; this consists of the tube, the proper ovarian ligament, and the suspensory ligaments. It consists of a dense, lamellated outer and a loose, reticular inner layer of connective tissue and an innermost single-layered epithelial lining. The connective tissue is intermingled with elastic fibers and sparse smooth muscle fibers. The rugose appearance of the cyst wall is due to the retractability of its elastic constituents. Sometimes the inner surface of the cyst is puckered, and in isolated cases even studded with papillary, cauliflower-like excrescences.
When bilateral adrenalectomy cures hypercortisolism fungus puns buy discount terbinafine on-line, there is less negative feedback on the corticotroph tumor cells with physiologic glucocorticoid replacement, and the adenoma may grow. However, when pituitary-dependent Cushing syndrome is caused by a corticotroph macroadenoma (>10 mm in largest diameter), the risk of tumor enlargement after bilateral adrenalectomy is high. If feasible, gamma knife radiosurgery is the treatment of choice for Nelson corticotroph tumors. However, unlike most pituitary adenomas, these neoplasms may demonstrate aggressive growth despite radiotherapy. Extensive cavernous sinus involvement may result in multiple cranial nerve palsies. Despite the concern about potential development of Nelson syndrome, clinicians should never hesitate to cure Cushing syndrome with bilateral laparoscopic adrenalectomy when transsphenoidal surgery has not been curative. Untreated Cushing syndrome can be fatal, but Nelson syndrome is usually manageable. Immunohistochemical studies on resected pituitary adenomas can determine the adenohypophyseal cell of origin. Suprasellar extension of the pituitary adenoma causes compression of the optic chiasm, resulting in the gradual onset of superior bitemporal quadrantopia that may progress to complete bitemporal hemianopsia (see Plate 1-11). Because the onset is gradual, patients may not recognize vision loss until it becomes marked. Additional mass-effect symptoms from an enlarging sellar mass include diplopia (with cavernous sinus extension and oculomotor nerve compression), varying degrees of pituitary insufficiency (related to compression of the normal pituitary gland by the macroadenoma), and headaches. Nonfunctioning pituitary macroadenomas are often associated with mild hyperprolactinemia. Currently, no effective pharmacologic options are available to treat patients with clinically nonfunctioning pituitary tumors. Observation is a reasonable management approach in elderly patients who have normal visual fields. Transsphenoidal surgery (see Plate 1-31) can provide prompt resolution of visual field defects and a permanent cure. The glandular cells have receptors for oxytocin and cause myoepithelial contraction when activated. In the absence of oxytocin, only approximately 30% of stored milk is released during nursing. There is a latent period of approximately 30 seconds between the onset of suckling and commencement of milk flow. Changes in estrogen and progesterone at the time of parturition help modulate the lactation response both by affecting oxytocin synthesis and secretion and by impacting oxytocin receptors. Oxytocin is a powerful uterotonic stimulant for contractions, and oxytocin secretion increases with the expulsive phase of parturition. During pregnancy, the uterus is maintained in a quiet state by the actions of progesterone and relaxin. The initiation of labor is accomplished by a relative increase in estrogen activation and a decrease in progesterone activation. Synthetic oxytocin administration is a clinically proven method of labor induction. Oxytocin is administered intravenously at an escalating dose until there is normal progression of labor, strong contractions occurring at 2- to 3-minute intervals, or uterine activity reaches 150 to 350 Montevideo units (the peak strength of contractions in mm Hg measured by an internal monitor multiplied by their frequency over 10 minutes). The secretion and action of vasopressin are regulated by osmotic and pressure/volume factors. The osmoreceptors are outside the bloodbrain barrier, are located in the organum vasculosum of the lamina terminalis (adjacent to the anterior hypothalamus near the anterior wall of the third ventricle), and are perfused by fenestrated capillaries. Ninety percent of the filtered water is reabsorbed in the proximal tubule without the help of vasopressin. The countercurrent multiplier system in the loop of Henle generates a high osmolality in the renal medulla. The ascending, or distal, limb of Henle loop actively transports sodium without water from the tubular urine to the interstitial fluid of the renal medulla, making it very hypertonic. The water impermeability of this limb of Henle loop renders the urine entering the distal tubule hypotonic with respect to plasma. In the absence of vasopressin, the distal tubule and collecting ducts remain largely impermeable to water, and very dilute urine leaves the kidney. Activation of the collecting duct V2 receptor increases water permeability to allow for osmotic equilibration between the urine and the hypertonic medullary interstitium. The sensation of thirst is typically triggered by a 2% increase in plasma osmolality. When seen in the outpatient clinic, these patients usually have a large thermos of ice water by their side. This sequence of events can be avoided by advising the patient to "drink for thirst only for the first 2 weeks" after a pituitary operation. Normal Langerhans cells-located in the epidermis, lymph nodes, thymic epithelium, and bronchial mucosa-process antigens and then migrate to lymphoid tissues, where they function as effector cells stimulating T-cell responses. When localized, the presenting findings may include bone, skin, or lymph node involvement. In infants, brown-purplish papules may be evident, which are usually associated with a benign and self-healing course in the first year of life.
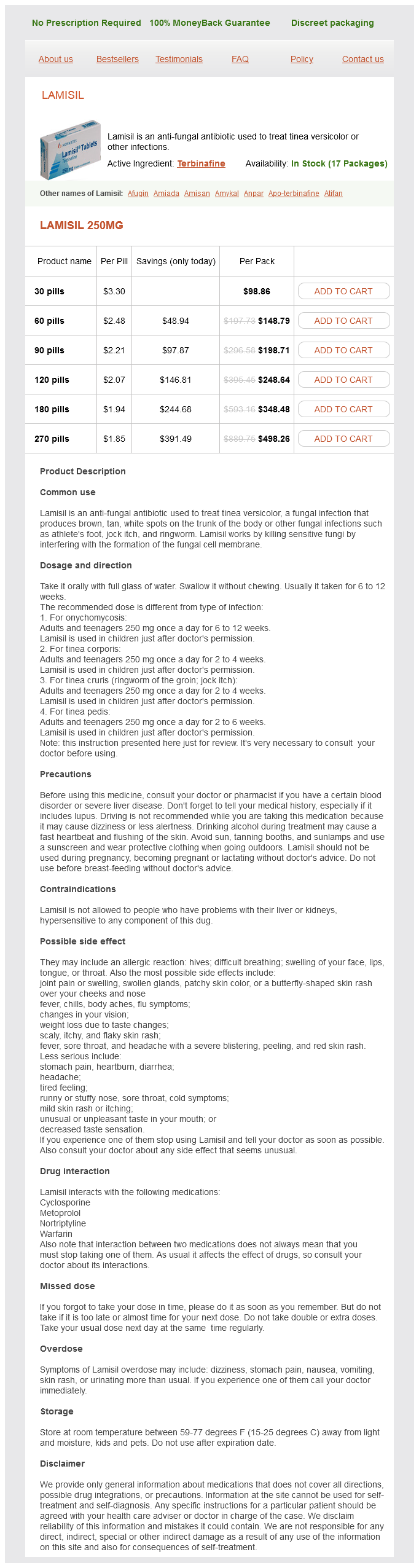
Terbinafine Dosage and Price
Lamisil 250mg
- 30 pills - $98.86
- 60 pills - $148.79
- 90 pills - $198.71
- 120 pills - $248.64
- 180 pills - $348.48
- 270 pills - $498.26
T4 and T3 are stored in the colloid as part of the Tg molecule-there are 3 to 4 T4 molecules in each molecule of Tg antifungal drug list generic terbinafine 250 mg fast delivery. T4 and T3 are then transported from the phagolysosome across the basolateral cell membrane and into the circulation. This action is inhibited by large amounts of iodine, a finding that can be used therapeutically in the treatment of patients with hyperthyroidism caused by Graves disease. There is approximately 250 g of T4 for every gram of thyroid gland-approximately 5 mg of T4 in a 20-g thyroid. Graves disease occurs more commonly in females than in males (8:1) and more frequently during the childbearing years, although it may occur as early as in infancy and in extreme old age. Rarely in a patient with Graves disease, there is no palpable enlargement of the thyroid gland. The hyperplastic thyroid functions at a markedly accelerated pace, evidenced by an increased uptake and turnover of radioactive iodine and increased levels of T4 and T3, which cause an increased rate of oxygen consumption or increased basal metabolic rate and decreased serum total and high-density lipoprotein cholesterol concentrations. The increased levels of T4 and T3 cause a variety of physical and psychologic manifestations. Patients with this malady are usually nervous; agitated; restless; and experience insomnia, personality changes, and emotional lability. The skin of patients with this disease is warm and velvety (because of a decrease in the keratin layer); it may also be flushed and is often associated with marked perspiration caused by increased calorigenesis. Onycholysis (known as Plummer nails)- loosening of the nails from the nail bed and softening of the nails-occurs in a minority of patients with Graves disease. Infiltrative dermopathy (pretibial myxedema) is the skin change that sometimes occurs in the lower extremities or on the forearms in patients with severe progressive ophthalmopathy. It presents as a rubbery, nonpitting swelling of the cutaneous and subcutaneous tissues, with a violaceous discoloration of the skin on the lower third of the legs. Graves disease is also associated with clubbing of the fingers and of the toes (thyroid acropachy). Hyperthyroidism has mixed effects on glucose metabolism, but affected patients typically have fasting hyperglycemia. The increase in serum sex hormonebinding globulin concentrations is also observed in hyperthyroid men, reflected in high serum total testosterone concentrations, low serum free testosterone concentrations, and mild increases in serum luteinizing hormone concentrations. Patients with Graves disease manifest the symptoms and signs of profound muscle changes known as thyroid myopathy. Atrophy of the temporal muscles, the muscles of the shoulder girdle, and the muscles of the lower extremities-notably the quadriceps femoris group-is typical. Muscular weakness is present, and these patients are often unable to climb steps or to lift their own weight from a chair. The effect on cortical bone density is usually greater than that on trabecular bone density. Thus, patients with long-standing hyperthyroidism are at increased risk for bone fracture and osteoporosis. Characteristically, patients with hyperthyroidism report a variety of cardiac symptoms and signs. Cardiac output is increased, and those who develop heart failure present the manifestations of high-output failure characterized by a shorter than normal circulation time despite elevated venous pressure. Enlargement of the heart is Eyelid lag Muscles Tremor Heart Infiltrative dermopathy (pretibial myxedema) Increased rate Increased cardiac output (unless heart failure develops) Usually little or no enlargement hyperthyroidism. Atrial fibrillation occurs in approximately 15% of patients and is more common in patients older than age 60 years. In most patients, the atrial fibrillation spontaneously converts to normal sinus rhythm when euthyroidism is established. Thus, a peripheral -adrenergic blocker will control most of the circulatory manifestations, reduce sweating, and diminish eyelid retraction-all independent of any effect on circulating levels of T4 and T3. The heart does not show any characteristic anatomic or microscopic changes that can be attributed to hyperthyroidism. Most patients with hyperthyroidism (regardless of the cause) have retraction of the eyelids (caused by contraction of the eyelid levator palpebrae muscles), which leads to widened palpebral fissures and a stare. Although the stare may give the appearance of proptosis, it must be confirmed with an exophthalmometer (see following text). There also may be globe lag- the eyelid moves upward more rapidly than does the globe as the patient looks upward. When the patient is requested to look in one direction or another, a significant weakness of one or more of the extraocular muscles may be noted. The patient may complain of blurred vision, or even of diplopia on looking either upward or to the side. If the distance, measured with an exophthalmometer, from the canthus to the front of the cornea exceeds 20 mm in white patients and 22 mm in black patients, proptosis is present. Testing the eye and the orbital contents for resiliency to pressure is also useful. Normally, the eyeball can be pushed back easily and without resistance; in patients with severe ophthalmopathy, however, a significant decrease in resiliency is evident, and in some patients, it is impossible to push the eyeball back at all-a poor prognostic sign of progressive ophthalmopathy. The progression may be so rapid and extensive that the eyelids cannot be closed over the eyes, so that ulcerations of the cornea may result. Cigarette smoking has been clearly shown to increase both the risk for and the severity of ophthalmopathy.