General Information about Suhagra
Suhagra is out there in several strengths, ranging from 25mg to 100mg, and is usually taken half-hour to 1 hour earlier than sexual activity. It can be taken with or without food, however it is recommended to keep away from high-fat meals as they could delay the drug's results. Its effectiveness can last as lengthy as four hours, providing ample time for spontaneous sexual activity.
Erectile dysfunction is a typical situation that impacts males of all ages. It is the inability to realize or keep an erection adequate for sexual exercise. This could be a source of great distress and can result in relationship issues, low self-esteem, and even depression. ED could be brought on by various factors such as physical situations, psychological issues, or life-style decisions.
Like any medicine, Suhagra could trigger unwanted effects in some individuals. The most common side effects reported embody headache, facial flushing, upset abdomen, and dizziness. These unwanted effects are gentle and normally subside on their very own. However, if they persist or become bothersome, it is essential to consult a healthcare provider for correct steerage.
Suhagra is a widely used treatment for the remedy of erectile dysfunction (ED) in males and pulmonary arterial hypertension (PAH). It is a potent and efficient drug that has helped countless people improve their sexual health and total well-being.
Suhagra, additionally identified by its generic name sildenafil citrate, belongs to a class of medication called phosphodiesterase kind 5 (PDE5) inhibitors. It works by stress-free the muscles and rising the blood circulate to the penis, allowing for a stronger and longer-lasting erection. This medicine is often prescribed to males who have difficulty attaining or sustaining an erection due to bodily causes similar to diabetes, high blood pressure, or nerve injury.
It is necessary to notice that Suhagra isn't a remedy for ED or PAH. It is a remedy that helps improve the symptoms and permits for a more satisfying sexual experience. It does not defend against sexually transmitted infections, and it shouldn't be used by people who aren't experiencing ED or PAH.
Aside from its use in treating ED, Suhagra can be accredited for the treatment of pulmonary arterial hypertension (PAH). PAH is a situation where the blood vessels within the lungs become slender and put stress on the guts, making it difficult for the heart to pump blood to the lungs. This can result in shortness of breath, fatigue, and chest ache. Suhagra works by enjoyable the blood vessels in the lungs, decreasing the pressure and improving blood move, ultimately easing the signs of PAH.
In conclusion, Suhagra is an effective treatment for the therapy of erectile dysfunction and pulmonary arterial hypertension. It has helped many people reclaim their sexual well being and enhance their overall quality of life. If you may be experiencing signs of ED or PAH, consult your doctor to see if Suhagra is best for you. Remember to all the time follow your physician's directions and by no means take greater than the prescribed dose. With the proper treatment and support, ED and PAH can be managed successfully, allowing for a fulfilling and gratifying life.
This usually leaves several branches intact to the antrum erectile dysfunction diabetes qof suhagra 100 mg with visa, and in combination with preserved right gastric and gastroepiploic arteries, this leads to excellent graft perfusion in most patients. After completing the cervical anastomosis, the graft is gently pulled into the abdomen to eliminate redundancy and sutured to the crura to prevent herniation of abdominal organs into the mediastinum. At this point, the operation is complete with the exception of passing a nasogastric tube and placing a feeding jejunostomy tube. Since the antral innervation has been preserved, no pyloroplasty should be performed. When a gastric pull-up is planned, the vagal-sparing procedure is readily adapted to a fully laparoscopic approach. The gastric mobilization as well as the highly selective vagotomy are straightforward laparoscopic procedures. I have found that the use of a 4-cm incision in the midline with placement of a hand port facilitates stripping the esophagus out (via the hand port) and subsequent dilatation of the mediastinal tract. The graft is pulled up attached to a chest tube, and the cervical esophagogastric anastomosis is accomplished in standard fashion. When a colon graft is used with preservation of the intact, innervated stomach, there are several important technical considerations. First, only the cardia immediately below the gastroesophageal junction is excised, leaving the remaining stomach in place. A highly selective vagotomy is performed along the lesser curvature to reduce acid secretion and provide protection from the development of cologastric anastomotic ulcers. Instead, only the proximalmost one to two short gastric vessels, along with the posterior pancreaticoduodenal vessels, are divided, so that there is an approximately 10 cm window created near the left crus of the diaphragm. Importantly, the colon graft is passed up posterior to the stomach through this window, into the hiatus, and then up through the posterior mediastinum. In patients with achalasia, where only the mucosa was stripped out through an anterior gastrotomy, the entire muscular tube of the native esophagus remains intact, and a sufficient-sized hole must be cut into the residual muscular tube along the left lateral aspect near the hiatus to allow the colon graft to be pulled up inside. If all layers of the esophagus have been stripped out, as in patients with high-grade dysplasia or intramucosal cancer, then that issue does not exist since the muscular wall of the esophagus is gone and only the mediastinal tract is present at the hiatus. The esophago-colo anastomosis is done either with a stapled or hand-sewn technique in an end-to-end fashion. If the muscular tube of the esophagus has been preserved, it can be pulled up like a sheath to cover the anastomosis proximally. The colon is then pulled firmly down into the abdomen to eliminate any redundancy and sutured to the left crus of the diaphragm to prevent twisting of the graft or herniation of abdominal contents into the mediastinum. In particular, sutures should be placed between the colon graft and the posterior aspect of the hiatus near crural decussation since herniation can occur underneath the colon graft if these sutures are omitted. The colon is divided approximately 10 to 15 cm distal to the hiatus, taking care not to injure the vascular arcade. Next, the colocolostomy is accomplished in standard fashion, with care taken to avoid traction on the left colic vessels or the marginal artery supplying the graft. Typically this requires that the right colon be brought up into the left upper quadrant. It is nearly always a "one and done" therapy that eliminates the diseased mucosa and the need for further interventions, and offers reduced side effects and better functional outcome compared with other types of esophagectomy. A vagal-sparing procedure is only an option with patients at low risk for lymph node metastases, since no formal lymphadenectomy is performed. Therefore any nodules or lesions in a patient with Barrett or squamous cell cancer must first undergo endoscopic resection to confirm if they are malignant and to pathologically determine the depth of invasion. Long-term good outcome can be achieved using either the tubularized stomach with pyloric innervation maintained or a colon interposition to the intact, innervated stomach for esophageal replacement. Indications and technique of colon and jejunal interpositions for esophageal disease. The term minimally invasive can refer to performing either or both the thoracic and abdominal phases of the operation with either laparoscopic or robotic assistance. The surgeon sits at a console some distance from the patient, who is positioned on an operating table close to the robotic unit with its four robotic arms. The robotic arms incorporate remote center technology, in which a fixed point in space is defined, and about it the surgical arms move so as to minimize stress on the thoracic or abdominal wall during manipulations. The small proprietary Endowrist instruments attached to the arms are capable of a wide range of high-precision movements. The image comes from a maneuverable highdefinition stereoscopic camera (endoscope) attached to one of the robot arms. The console also has foot pedals that allow the surgeon to engage and disengage different instrument arms, reposition the console "master" controls without the instruments themselves moving, and activate electric cautery. The Xi system is newer and features an overhead beam that permits rotation of the instrument arms, allowing for greater flexibility in terms of direction of approach of the robot to the patient. Compared with the Si, the Xi also has thinner instrument arms, longer instruments themselves, and the option to switch the camera to any arm/port. The need to perform an en bloc resection of aorta or intrathoracic trachea or carina along with the esophagectomy, which has been safely applied to selected patients, would generally be considered a contraindication to robotic esophagectomy. Comorbidities or poor functional status that would otherwise make patients suboptimal candidates for esophagectomy generally would also apply to offering robotic esophagectomy, although robotic esophagectomy may permit surgeons to offer esophagectomy to somewhat older and sicker patients by decreasing the perioperative complication rate (especially respiratory complications). Smoking cessation should be encouraged and alcohol use should be noted to screen for cirrhosis and warn of possible withdrawal issues in the perioperative period. We consider any patient that is a candidate for esophagectomy to be a candidate for robotic esophagectomy as well. Robotic techniques can be applied to Ivor Lewis, modified McKeown, or transhiatal esophagectomies. We describe our technique for the abdominal and thoracic phases (performed robotically), and cervical phase, of these operations.
Chronic prolapse is seen at times with surprisingly large protrusions of the distal stomach up and over the edge of the gastric band erectile dysfunction other names discount suhagra 50 mg without prescription. Prolapse can occur at any time after the procedure, and its incidence slowly rises with duration of the band being in place. If doubt exists, a low-volume Gastrografin or barium swallow will confirm the diagnosis. This will, in most cases of acute prolapse, provide enough reduction in the restriction of the prolapsed stomach to allow it to slip back down through the band and resume its normal position. However, if removal of all fluid does not produce immediate relief of symptoms by the patient, a swallow study is indicated. If the swallow shows a large and persistent prolapse, emergent surgical therapy is indicated to laparoscopically reduce the prolapse and prevent gastric ischemia. A laparoscopic approach to freeing the buckle of the band, unbuckling the system, reducing the prolapse to its appropriate location, and repositioning and rebuckling the band is quite feasible. Chronic stenosis or band placement too high onto the distal esophagus may produce esophageal obstruction and dilation. Resolution of the obstruction will usually result in the esophagus regaining its normal size. Failure to secure the port to the fascia can result in the port turning in the subcutaneous space and being unable to be accessed for further adjustments. When such adjustments are made, a good rule of thumb is to have the patient drink several swallows of water quickly after the adjustment is made. If the patient feels the water stop and give a sensation of partial blockage, then the adjustment is too tight and must be loosened. Optimal restriction varies from patient to patient, but in general a goal of restriction to one cup of food or less at a meal and production of satiety for at least a few hours after eating are the goals of an optimal adjustment. It achieved initial popularity in the mid 1970s and has remained a standard operation since that time. The technique of creating the gastrojejunostomy and the length and location of the Roux limb has varied from surgeon to surgeon. No optimal technique or configuration has emerged, although some differences have been shown. Its performance using a laparoscopic approach has clearly been an improvement over the open approach, as with all other operations where minimal access has been used. Elimination of incisional hernias, decreased pain and recovery time, and decreased overall complication rates and mortality have all been confirmed with using the laparoscopic approach. Failure of a trial of dieting and mental stability are also considered standard criteria. Other criteria vary among surgeons and institutions, including upper and lower age limits, size limits, and requirements of cessation of addictive habits. The mesentery is then further divided with the Harmonic scalpel to obtain as deep a division of the mesentery as possible without encountering the very large vessels at the base of the mesentery. The proximal end of the Roux limb is then marked by suturing a small Penrose drain to it. Then the mesenteric defect at the enteroenterostomy is closed with a running permanent suture. The transverse colon mesentery is now grasped and elevated, exposing the lower portion of the mesentery near the ligament of Treitz. A defect is made in the mesentery to the left and a few centimeters above the ligament of Treitz. This location usually avoids major vessels, but the surgeon must be aware of the vascular anatomy, if visible, and cautious not to disrupt it unnecessarily. Openings between mesenteric vessels are easier to find than dealing with bleeding from major mesenteric vessels. Once the mesentery has been opened to expose the lesser sac, the posterior surface of the stomach can be seen. It is grasped and pulled out of the mesenteric defect a few centimeters, after which the plane below the stomach is confirmed with a grasper. Usually if one can pass 4 cm of bowel or more past the cut edge of the mesentery, that will suffice for later retrieval. It is very easy to have the bowel twisted a full 180 degrees or more between first passing it to the left upper quadrant then retrieving it to pass it through the transverse colon mesentery. The mesentery of the Roux limb must be visually confirmed without a doubt as being straight and vertical as the limb is passed superiorly through the transverse colon mesentery. The Harmonic scalpel is used to create an opening in the mesentery along the lesser curvature of the stomach. However, for very large patients, creating this opening at the incisura is advisable because the longer gastric pouch is often needed to allow the Roux limb to easily reach the proximal stomach without tension. Then I prefer to size the pouch with an Ewald tube (30 French) and place the stapler close to but not directly adjacent to the tube, which is visible by the contour it creates on the gastric surface. It is important to exclude the fundus from the proximal part of the newly created gastric pouch. Similarly, the anesthesiologist needs to double confirm there are no temperature probes or orogastric tubes in the stomach other than the Ewald tube. If it is not, the inferior surface of the transverse colon mesentery must again be exposed and the Roux limb passed into the retrogastric space again. I continue to use a retrogastric retrocolic location of the Roux limb due to the fact this is the shortest distance from between jejunum and proximal stomach. A more popular approach is to bring the Roux limb directly anterior to both transverse colon and distal stomach and create the gastrojejunostomy. This approach is technically easier, except when the mesentery of the Roux limb is short and there is difficulty in stretching the Roux limb to reach the proximal gastric pouch.
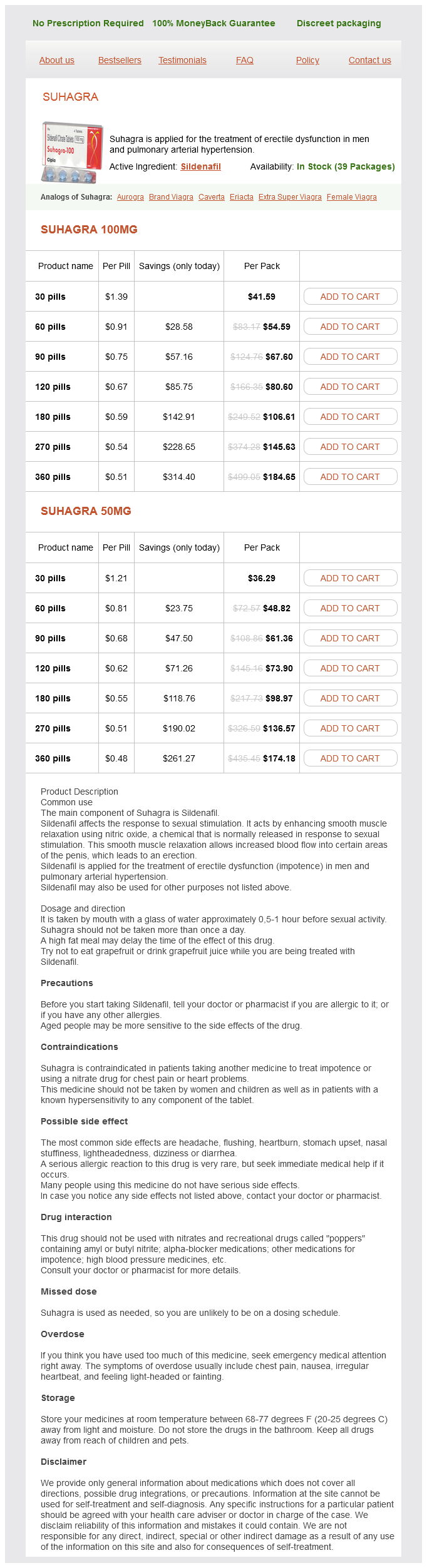
Suhagra Dosage and Price
Suhagra 100mg
- 30 pills - $41.59
- 60 pills - $54.59
- 90 pills - $67.60
- 120 pills - $80.60
- 180 pills - $106.61
- 270 pills - $145.63
- 360 pills - $184.65
Suhagra 50mg
- 30 pills - $36.29
- 60 pills - $48.82
- 90 pills - $61.36
- 120 pills - $73.90
- 180 pills - $98.97
- 270 pills - $136.57
- 360 pills - $174.18
In a setting of cirrhosis impotence after 40 discount suhagra 50 mg overnight delivery, biopsy is usually sufficient to confirm malignancy, when present. Biopsy diagnosis of highgrade dyspla sia is useful to direct increased surveillance. In selected patients, it may be appropriate to treat the lesion with alcohol or radiofrequency ablation immediately follow ing the biopsy. Most errors in clinical diagnosis occur when uncom mon lesions are not considered. The differential diagno sis of spaceoccupying lesions in cirrhotic livers includes dysplastic nodule, hepatocellular carcinoma, cholangio carcinoma, haemangioma, simple cyst, metastasis, arterialized regenerative nodule, and regional parenchy mal extinction. At left is background liver showing increased cytoplasmic glycogen, typical of glycogen storage disease. Thus, hor mones, including oestrogens and androgens, must be stopped whenever possible, whence many lesions will regress. In pregnancy, adenomas commonly enlarge and may rupture and bleed, although with low frequency [1214]. Control of glycogen storage disease may allow lesions to regress and decrease the emergence of new lesions. Surgical excision should be considered for lesions that are symptomatic or measure greater than 5 cm diameter. Adenomas in men should be excised because of the high risk of malignant transformation [6,12]. The dysplastic nodule shows low N/C ratio and plates one to two cells in thickness. The carcinoma shows increased N/C ratio with plates two to four cells in thickness. Women usually present in their reproductive years; the majority have taken oral contraceptives although a pathogenic role has not been proven [2427]. Although most lesions are asymptomatic and discovered incidentally, large lesions may present with pain or an abdominal mass. Histologically, the lesion consists of normal hepatocytes, usually arranged about a central region of fibrous tissue that contains large arteries and proliferating bile ducts. The background liver is usually normal, although hepatic haemangioma is found in 20% of cases. Although usually crypto genic, individual cases have been preceded by a potential cause of venous injury such as trauma, liver transplanta tion [29], tumour infiltration [30], and in children after chemotherapy [31] or stemcell transplant [32]. Molecular studies have usually demonstrated a poly clonal pattern, as would be expected in a reactive lesion [34]. Lesions with adjacent coincident or admixed hepatocellular adenoma also occur rarely [36]. Some nodules arising in the setting of large portal vein anomalies have expression or mutation profiles suggestive of adenomas. These complex examples sug gest that vascular events may initiate hyperplasia and occasionally adenomas or adenomalike proliferations. Diagnosis A confident diagnosis can be made by imaging when there is a hypervascular mass supplied with a single central artery and centrifugal blood flow [5]. In its absence, confusion with hepatocellular adenoma, hepatocellular carcinoma, or other lesions may occur. Biopsy is recom mended when clinical diagnosis is in doubt, especially when growth is observed. Reports of malignant transformation are rare and may reflect misdiagnosis or coincident lesions. Surgery may be considered when the diagnosis is not certain or if the lesion is large, pedunculated, or symptomatic. The lesion is composed of benignappearing hepatocytes supplied by altered portal tracts. This enzyme is strongly expressed near hepatic veins but not in periarterial regions, giving the classic maplike pattern. Nodular regenerative hyperplasia this condition is defined histologically by the presence of micronodules 12 mm in diameter delineated by regions of atrophy and without fibrous septa [43]. Patients with portal hypertension present with splenomegaly and varices, and less often with ascites [46]. However, the possibility of hepatocellular or metastatic carcinoma should be considered. Liver biopsy is useful when the clinical situation demands exclusion of cirrhosis. A needle biopsy less than 2 cm in length may not be sufficient to exclude macronodular cirrhosis, incomplete septal cirrhosis, or regressed cirrhosis. Focal fatty change and focal fatty sparing Regional variation in amount of liver cell fat can produce entities called pseudolesions or pseudotumours, usually discovered during imaging [48]. Focal fatty change gen erally occurs near the hilum, possibly as a response to insulin delivery from a pancreatic vein into the parabil iary plexus of Couinaud [49]. The reverse effect of focal fatty sparing in an otherwise fatty liver can occur when a region near the hilum is perfused with lowinsulin blood from a pyloric vein [48]. Because focal fatty sparing can only occur in the presence of fatty liver disease, most of these patients have obesity or alcoholism.