General Information about Prochlorperazine
In conclusion, prochlorperazine, also identified as Compazine, is a strong and versatile medication that's extremely effective in treating both psychological well being disorders and bodily signs corresponding to nausea and vertigo. With its lengthy historical past of successful use and minimal side effects, it continues to be a most well-liked remedy possibility for sufferers and healthcare professionals alike. If you may be experiencing symptoms of schizophrenia, bipolar dysfunction, or nausea and vertigo, speak to your physician about whether prochlorperazine could additionally be an appropriate treatment for you.
Prochlorperazine belongs to a category of medications known as phenothiazines, which work by blocking sure neurotransmitters within the brain. These neurotransmitters, specifically dopamine and serotonin, play a key position in regulating mood and conduct. By blocking their motion, prochlorperazine helps to stabilize the brain's chemical stability and reduces the severity of psychotic signs.
It is necessary to note that prochlorperazine could work together with different drugs, so it's essential to tell your physician of any other medicines you take earlier than starting treatment. It also wants to be averted by individuals with certain medical situations similar to liver disease, low blood stress, and a historical past of seizures.
Prochlorperazine works by blocking certain receptors in the mind which are answerable for triggering the sensation of nausea and dizziness. It is considered to be a highly efficient anti-emetic (anti-vomiting) medication and is often prescribed for folks undergoing chemotherapy or surgery, in addition to those experiencing nausea as a end result of other medical situations.
Prochlorperazine, also identified by its brand name Compazine, is a flexible medicine that is primarily used to treat psychotic disorders similar to schizophrenia. However, it is also commonly used within the treatment of nausea and vertigo. First developed within the Nineteen Fifties, prochlorperazine has been a mainstay in the subject of psychological health and has been proven to be highly efficient in relieving signs related to psychotic disorders.
As with any medication, there are some potential unwanted effects associated with prochlorperazine. These can include drowsiness, dry mouth, constipation, and blurred vision. However, these unwanted side effects are typically mild and may be managed by adjusting the dosage or switching to a unique type of treatment.
Apart from its use in mental health, prochlorperazine is extensively used within the treatment of nausea and vertigo. Nausea is a standard symptom that might be caused by a variety of elements, including movement illness, treatment unwanted effects, and other medical conditions. Vertigo, however, is a sensation of dizziness and spinning that can additionally be brought on by various factors corresponding to inner ear issues, head injuries, and medicine unwanted facet effects.
One of the first makes use of of prochlorperazine is in the remedy of schizophrenia, which is a persistent psychological disorder characterised by hallucinations, delusions, and disordered thinking. It is estimated that approximately 1% of the global inhabitants suffers from schizophrenia, and prochlorperazine has been confirmed to significantly enhance the quality of life for those affected.
In addition to schizophrenia, prochlorperazine may additionally be used in the treatment of other psychotic disorders corresponding to bipolar dysfunction, in which individuals expertise extreme shifts in temper and habits. It can be effective within the management of acute agitation and aggression in sufferers with psychological well being circumstances.
When taken for the remedy of nausea, prochlorperazine may be administered through oral tablets or suppositories, which are inserted into the rectum. For vertigo, it is usually given via injections or as a pores and skin patch. The dosage and type of the treatment prescribed will rely upon the affected person's situation and medical history.
It remains stable with cooking at high temperature but is inactivated by ascorbic acid medicine dictionary purchase 5 mg prochlorperazine. In the acidic pH of stomach, Cbl is released by enzymatic digestion from protein complexes in food. Also a small fraction (< 1%) of a large oral dose gets absorbed passively from the oral, gastric and small intestinal mucosa. In presence of concurrent iron deficiency or thalassemia trait, macrocytosis may get masked. The nuclear chromatin of the erythroid precursors appears loose giving the characteristic appearance of the megaloblast. There is asynchronicity in maturation of the nucleus and cytoplasm leading to nucleus appearing less mature than the cytoplasm. It can help to rule out other disorders such as aplastic anemia, leukemia and myelodysplasia. Marrow is hypercellular, myeloid:erythroid ratio changing from 3:1 to 1:1 due to increased erythropoiesis. Dyserythropoiesis is evidenced by nuclear remnants, bi- and trinucleated cells, Howell-Jolly Serum homocyteine and serum methylmalonic acid levels are useful in differentiating between folate and Cbl deficiency. In folate deficiency, only homocysteine is raised with normal methylmalonic acid levels while in Cbl deficiency, levels of both are significantly raised. Methylmalonic acid and total homocysteine levels are sensitive indicators of vitamin B12 deficiency and correlate with clinical abnormalities and therapeutic response. However, care should be taken in interpreting these results as they are not specific to vitamin B12 deficiency. Serum folate and cobalmin levels are easily available tests but have high-false positivity and negativity. Also, the levels normalize fairly rapidly with replacement therapy or even with normal hospital diet. Serum vitamin B12 level Normal values 200Â800 pg/mL, vitamin B12 deficiency levels less than 80 pg/mL. Serum and red cell folate levels Red cell folate normal levels: 74 640 ng/mL; serum folate: normal levels: greater than 5Â6 ng/mL; borderline: 3Â5 ng/mL; low: less than 3 ng/mL. It reflects increased turnover of cells in the marrow due to ineffective erythropoiesis. For excluding orotic aciduria, urinary excretion of orotic acid should be assessed. Folate Deficiency With 100Â200 µg folic acid per day, optimal response may be seen in most patients. With administration of high-dose folate, the hematologic features of Cbl deficiency may reverse, but the neurologic manifestations can progress. So, it is important to rule out Cbl deficiency before treating solely with folate. The appetite improves and a sense of well-being returns within 1Â2 days of the treatment. Within the marrow, megaloblastic changes diminish in 24Â48 hours, but large myelocytes, metamyelocytes, and band forms may be present for several days. Folic acid is usually given for several months till a new population of red cells has been formed. If the underlying disease is treated appropriately, there is no need to continue folic acid for life. In some situations, it is advisable to continue the folic acid to prevent recurrence, for example, in chronic hemolytic anemia such as thalassemia or in patients with malabsorption who do not respond to a gluten-free diet. For treating nutritional folate deficiency, an improved diet or a folate supplement, or both may be required. For patients who have folate malabsorption, 5Â15 mg/day of folate should yield normal or high serum and erythrocyte folate levels. Folic acid deficiency is relatively easy to treat; added folate in the diet of the patients may be sufficient to treat. In some patients with vitamin B12 deficiency, parenteral therapy may be necessary. Vitamin B12 deficiency may be associated with severe neurologic abnormalities which may be long lasting and may not improve even with appropriate therapy. Megaloblastic anemia is characterized by the presence of macrocytes in the blood and megaloblasts in the bone marrow. Common causes of megaloblastic anemia in childhood are deficiency of folate or vitamin B12 (Cbl) or defects in their metabolism. With appropriate investigations, underlying cause of the megaloblastic anemia should be established. Successful treatment of patients with folate and Cbl deficiency involves: Correction of the deficiency, identifying and treating the causative disorder, improvement of the diet, follow-up evaluations to monitor the clinical status and to prevent the recurrences. Cobalamin Deficiency Daily dose of 25Â100 g may be used to start therapy along with potassium supplements. Conventional therapy in megaloblastic anemia due to vitamin B12 deficiency has been 1,000 g of cyanoCbl or hydroxyCbl by injection daily for 1 week, followed by 100 g of cyanoCbl weekly for 1 month and then monthly thereafter. Patients with methylmalonic aciduria with defects in the synthesis of Cbl coenzymes are likely to benefit from massive doses of vitamin B12. However, not all patients in this group benefit from administration of vitamin B12. Congenital methylmalonic aciduria can be diagnosed in utero by measurements of methylmalonate in amniotic fluid or maternal urine. In vitamin B12-responsive megaloblastic anemia, the reticulocytes start to rise on the 3rd or 4th day, peak on the 6th to 8th day, and gradually fall to normal by about the 20th day.
Risk factors for persistence of wheeze into adulthood include female sex medications diabetes buy generic prochlorperazine, atopy, airway hyperresponsiveness, poor lung function in childhood and smoking. The physical examination in the preschool child with wheeze may be normal at consultation as intermittent symptoms are most common at this age. If symptomatic at the time of examination, physical findings commonly include polyphonic expiratory wheeze as a manifestation of diffusely narrowed small airways. During an acute exacerbation, labored breathing with intercostal, suprasternal and substernal retractions may be present, along with an audible wheeze. In the preschool child who is asymptomatic on examination, the diagnosis is dependent on a careful history of previous symptoms. Within the syndrome of preschool wheeze, several phenotypes have been proposed, as shown in Box 1. These phenotypes are used to study risk factors, prognosis and response to treatment. However, these phenotypes probably represent different facades of the same entity, as there is significant overlap between the phenotypic categories. From the few studies that used bronchial biopsies or bronchoalveolar lavage, it is clear that the inflammatory reactions in preschool children with wheeze differ from those in older children with established asthma. Two cross-sectional studies have suggested that in preschool wheezers, there may be a window of around 18 months between symptom onset and development of airway wall changes consistent with asthma. In the first study, infants (median age 12 months) were investigated for severe respiratory symptoms, using infant lung function, bronchodilator reversibility and rigid bronchoscopy. A thorough history in a wheezy child that includes details of the wheezing episode, such as onset, duration and associated factors often provides clues to allow prioritization of diagnostic possibilities listed in Table 1. In a child with a clear history of episodic (viral) or multiple-trigger wheeze, no initial investigations are necessary. A chest X-ray is not generally required, but may be helpful if other diagnoses need to be considered. A trial of bronchodilator through a spacer may be diagnostic and therapeutic in a child who is seen while symptomatic. Pulmonary function testing, a valuable tool in aiding asthma diagnosis is not frequently used in preschoolers, but can be successfully performed in children as young as 3 years. Further evaluation with investigations as listed in Table 1 can be considered in a step-wise manner in wheezers with a more complex history and in those not responsive to a trial of inhaled corticosteroids. However, when symptoms are severe or frequent, initiating preventive treatment will reduce symptoms and improve quality of life. Treatment options include intermittent montelukast for episodic (viral) wheezers and prophylactic low-dose inhaled corticosteroids with bronchodilators (as per need) and montelukast for multiple-trigger wheeze. Several randomized controlled trials show that early use of inhaled corticosteroids, whether continuously or intermittently with viral colds, does not affect progression of disease and treatment should be solely focused on control of current symptoms. Acute symptoms are treated with short-acting beta-agonists, systemic corticosteroids and oxygen in severe cases. Oral steroids are not indicated in preschool children with attacks of wheeze who are well enough to remain at home and in many such children, especially those with episodic viral wheeze, who are admitted to hospital. Preventive Therapy the use of inhaled or oral corticosteroids in preschool wheezers is common in clinical pediatric practice. Airway obstruction in asthma results from a combination of bronchospasm, mucosal edema and mucus plugging. This leads to increased resistance to airflow through the larger airways and decreased flow through the smaller airways due to narrowing and early closure resulting in hyperinflation and retention of air. Due to regional differences in the resistance and uneven circulation to the alveoli, there exists a ventilation-perfusion mismatch. They have a high negative predictive value and a poor positive predictive value (typically positive predictive values 44Â54, negative 81Â88). Several phenotypes of preschool wheezers are described based on wheeze onset and duration, symptom pattern and atopic status. It is difficult to predict which infants and preschoolers with wheeze will subsequently develop asthma. Scoring systems are available but are of limited predictive value, and may not apply at individual level. Inhaled corticosteroids control symptoms and exacerbations in recurrent wheezers, but are not disease modifying. Genetically predisposed individuals are shown to react to certain inducers Table 4), which generate an immune response. Th2 cytokine-mediated predominance is seen with a chronic activation of different cell lines which include inflammatory cells like mast cells, eosinophils, lymphocytes, macrophages and dendritic cells and structural cells like epithelial cells and smooth muscle cells. The role of anti-inflammatory therapy and immunotherapy is targeted at this stage of pathogenesis. Triggers Table 4) are agents that stimulate symptoms in a child predisposed to wheezing due to prior sensitization with these inducers. As per the Hygiene Hypothesis, this induction can be prevented by avoidance of allergens or early exposure to endotoxins. Definition, assessment and treatment of wheezing disorders in preschool children: an evidence-based approach. Classification and pharmacological treatment of preschool wheezing: changes since 2008. Episodic viral wheeze and multiple trigger wheeze in preschool children: a useful distinction for clinicians? Allergens There are numerous indoor and outdoor allergens of clinical significance which are shown to be associated with asthma.
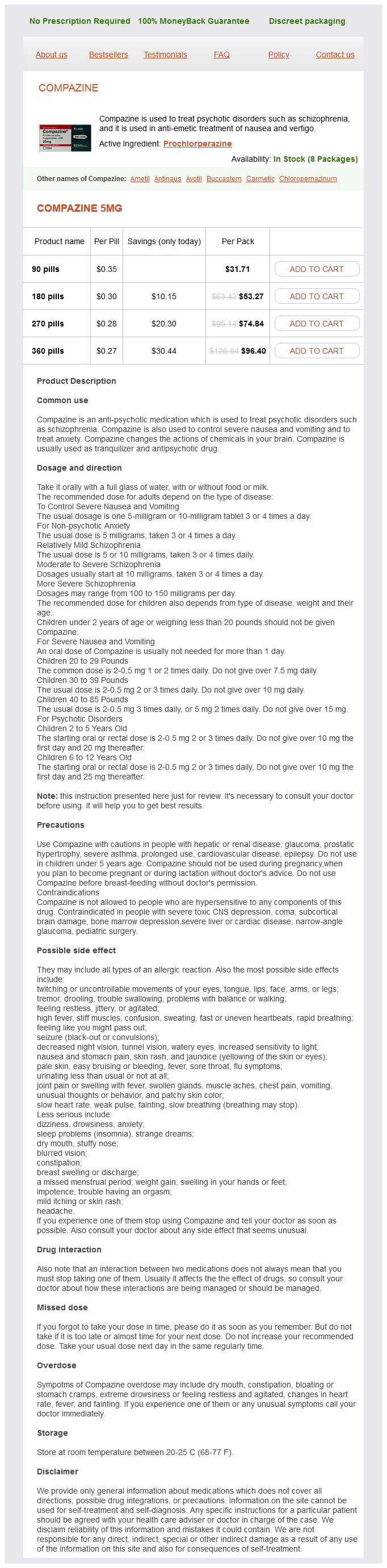
Prochlorperazine Dosage and Price
Compazine 5mg
- 90 pills - $31.71
- 180 pills - $53.27
- 270 pills - $74.84
- 360 pills - $96.40
Hence it must be stored at 4Â8°C after reconstitution and discarded after 4 hours medications on nclex rn cheap prochlorperazine 5 mg. Transplacentally-acquired maternal antibodies protect not only the infants against the disease but also neutralize the immunogenic property of the vaccine if administered during infancy. Hence it should be administered at an age when majority of infants would have lost these antibodies and are susceptible to develop the disease. Therefore, in developing countries the recommended minimum age is 9 months when almost 85Â95% of those vaccinated get seroconverted. Depending upon the strain of vaccine virus, 10Â20% of vaccines may develop mild to moderate fever about 6Â8 days after receiving measles vaccine. One to five percent of children may develop a few red spots on the trunk during this period. The vaccine is contraindicated in pregnancy, significantly immunocompromised states such as leukemia, administration of antimetabolites, radiations or corticosteroids, and recent administration of immune-globulin within last 3 months. Hypersensitivity to eggs and neomycin is a contraindication for vaccine prepared from chick embryo cells but not for the one prepared from human diploid cell cultures. In case of an outbreak, post-exposure immunization with live measles vaccine within 72 hours of exposure to a case may modify the illness and provide protection in certain cases. Laboratory confirmation of the disease is not required in regions where the disease is common. Serum IgM becomes positive after 2Â3 days after the onset of rash and persists for next 4Â5 weeks. In case the sample is collected within first 3 days of onset of rash, demonstration of a fourfold rise in IgG in convalescent sera, i. The total lymphocyte count is reduced with a greater reduction in lymphocytes as compared to neutrophils during the illness. Acute phase reactants like erythrocyte sedimentation rate and C-reactive protein are generally not altered. Infectious mononucleosis should be suspected if there is generalized lymphadenopathy and hepatosplenomegaly. Children with dengue fever have a rash that is confluent and also involves palms and soles. Meningococcal and streptococcal rash are characterized by petechiae, purpura, associated with a generalized toxic look. Rash of rosella infantum (caused by herpesvirus-6) typically starts from trunk and is associated with periorbital edema. Hence the treatment is mainly symptomatic and directed toward managing fever, cough, Passive immunization with measles immunoglobulin within 6 days of exposure in a susceptible contact may also prevent or modify the disease. It is indicated for children less than 1 year, pregnant and immunocompromised subjects who are more likely to develop complications of the disease. By utilizing the respiratory route, it is hoped to avoid neutralization by any maternal IgG antibodies that may be present. Immunogenicity and safety of aerosolized measles vaccine: systematic review and meta-analysis. Field effectiveness of live attenuated measlescontaining vaccines: a review of published literature. Introduction of a second dose of measles in national immunization program in India: a major step towards eradication. Surveys have demonstrated that the overall coverage for measles vaccine given between 9 months and 12 months is around 70%. Considering the vaccine efficacy to be around 85% for vaccination at 9 months, only around 60% (70% Ч 85% = 60%) of annual birth cohorts is actually protected against the disease leaving the rest 40% to be susceptible to measles. The second opportunity for immunization represents another opportunity for immunization for children who missed the first dose in the routine program and for children who failed to develop immunity after their first dose. Routine measles vaccination for children combined with mass immunization campaigns in countries with high case and death rates are key public health strategies to reduce global measles deaths. National Technical Advisory Group of the Government of India has recommended strengthening the coverage of routine measles immunization at 9Â12 months of age; reducing the drop outs; vaccination of children at the earliest up to 5 years, who have missed the 9Â12 months schedule and reporting children vaccinated over 1 year. The Group has also laid stress on skillful and standardized management of measles outbreaks. Measles can be eradicated because man is the only reservoir of the virus; the disease occurs due to only one serotype and an effective vaccine is available. Measles is the leading cause of death amongst all the vaccine-preventable diseases. The disease burden is high in India due to poor coverage under routine immunization and nonavailability of a second opportunity for measles vaccination in many of the states. Period of infectivity is usually 4 days before and 5 days after the onset of rash. The illness starts with the prodromal phase followed by enanthematous, exanthematous and recovery phases. Malnutrition, younger age, lack of breastfeeding, underlying malignancy or immunodeficiency, and low serum retinol (vitamin A) levels predispose to a more severe and complicated disease course. The clinical case definition of measles includes generalized maculopapular rash lasting more than or equal to 3 days; temperature of more than or equal to 38. The differential diagnoses of fever with maculopapular rash include rubella, infectious mononucleosis, roseola, fifth disease, group A streptococcal infection, meningococcemia, dengue fever, rickettsial infections, mycoplasma infections, Kawasaki disease and drug eruptions. Uncomplicated measles, like any other acute viral illness, generally resolves on its own within 7Â10 days.