General Information about Prednisolone
Endocrine problems, similar to adrenocortical insufficiency, may additionally be handled with prednisolone. This condition happens when the adrenal glands don't produce enough hormones, causing fatigue, muscle weak spot, and weight reduction. Prednisolone helps to replace these hormones and handle the signs of adrenocortical insufficiency.
Prednisolone is a commonly used medication that belongs to the group of drugs often recognized as corticosteroids. It is a synthetic type of the hormone cortisol, which is of course produced by the body's adrenal glands. This highly effective medicine has a big selection of medical makes use of, including treating allergic reactions, arthritis, breathing issues, sure blood issues, collagen diseases, eye ailments, cancer, endocrine issues, intestinal problems, swelling because of sure situations, and pores and skin conditions.
Prednisolone is also used for the therapy of certain blood issues, corresponding to aplastic anemia and hemolytic anemia. These situations happen when the body does not produce sufficient pink blood cells, leading to fatigue, weak point, and elevated danger of infections. Prednisolone helps to extend the production of purple blood cells, thus improving the symptoms of these blood issues.
Lastly, prednisolone can additionally be used for treating numerous skin conditions, corresponding to psoriasis. Psoriasis is a continual skin illness characterized by red, itchy, and scaly patches on the skin. Prednisolone helps to minimize back the irritation and suppress the immune response, providing aid from the signs of psoriasis.
Prednisolone is also used in the treatment of certain eye illnesses, corresponding to keratitis. This situation is characterised by inflammation of the cornea, which might lead to vision problems. Prednisolone is usually prescribed within the type of eye drops to minimize back irritation and promote healing of the cornea. It may be used to treat other eye conditions, similar to uveitis and conjunctivitis.
In addition to allergies, prednisolone is also commonly used for treating arthritis. Arthritis is a situation that causes irritation within the joints, resulting in ache, stiffness, and decreased mobility. Prednisolone works by lowering this inflammation, providing aid to those who undergo from arthritis. It can also be utilized in mixture with other medications, corresponding to nonsteroidal anti-inflammatory medication (NSAIDs), to handle the symptoms of arthritis.
Collagen diseases, such as lupus, can also be successfully managed with using prednisolone. Lupus is an autoimmune disease in which the physique's immune system attacks its own tissues and organs. Prednisolone helps to suppress the overactive immune response, offering aid from irritation and ache. It is usually prescribed in combination with different medicines to handle the signs of lupus.
Another condition that could be successfully handled with prednisolone is respiratory issues, such as bronchial asthma. Asthma is a persistent lung illness that causes difficulty in breathing, coughing, and wheezing. Prednisolone helps to decrease the inflammation within the airways, making it easier for individuals with bronchial asthma to breathe. It is often prescribed as a short-term remedy throughout bronchial asthma attacks, or as a maintenance medicine for people who have frequent bronchial asthma signs.
Furthermore, prednisolone is used for treating intestinal issues, such as ulcerative colitis. This inflammatory bowel illness causes irritation and ulcers in the digestive tract, resulting in belly ache, diarrhea, and rectal bleeding. Prednisolone helps to reduce this irritation, providing reduction from the signs of ulcerative colitis.
In conclusion, prednisolone is a flexible treatment that's used in the remedy of a variety of medical situations. It works by reducing inflammation and suppressing the immune response, providing relief from various signs. However, as with every medication, you will need to use prednisolone as prescribed by a well being care provider and to comply with all instructions rigorously to keep away from any potential side effects. If you might have any questions or issues about prednisolone, remember to seek the advice of together with your healthcare provider.
One of the primary uses of prednisolone is for the remedy of allergy symptoms. Allergies occur when the physique overreacts to a substance, such as pollen, mud mites, or pet dander. This can lead to symptoms similar to sneezing, itching, and watery eyes. Prednisolone works by reducing the body's immune response, thus offering reduction from these symptoms. It is usually prescribed in circumstances the place different allergy medications haven't been effective.
In some circumstances, prednisolone can also be used as part of cancer therapy. It is commonly prescribed to assist handle the unwanted side effects of chemotherapy, such as nausea, vomiting, and lack of appetite. Prednisolone may be used to treat certain types of leukemia, a sort of most cancers that impacts the blood and bone marrow.
A scoring system is helpful in defining which patients are eligible for percuta neous valvuloplasty allergy medicine infants prednisolone 40 mg buy cheap. One to four points are assigned to each of four observed parameters, with 1 being the least involvement and 4 the greatest: mitral leaflet thickening, mitral leaflet mobility, submitral scarring, and commis sural calcium. Patients with a total valve score of 8 or less respond best to balloon valvuloplasty as long as there is no significant mitral regurgitation. Because echocardiography and careful symptom evalu ation provide most of the needed information, cardiac catheterization is used primarily to detect associated coro nary or myocardial disease-usually after the decision to intervene has been made. Treatment & Prog nosis In most cases, there is a long asymptomatic phase after the initial rheumatic infection, followed by subtle limitation of activity. Pregnancy and its associated increase in stroke volume results in an increased transmitral pressure gradi ent and may precipitate symptoms. Toward the end of pregnancy, the cardiac output continues to be maintained by an increase in heart rate, further increasing the mitral gradient by shortening diastolic time. Patients with moder ate to severe mitral stenosis should have the condition corrected prior to becoming pregnant if possible. Pregnant patients who become symptomatic can undergo successful surgery, preferably in the third trimester, although balloon valvuloplasty is the treatment of choice if the echocardiog raphy valve score is low enough. The onset of atrial fibrillation often precipitates symp toms, which improve with control of the ventricular rate or restoration of sinus rhythm. Once atrial fibrillation occurs, the patient should receive warfarin anticoagulation therapy even if sinus rhythm is restored, since atrial fibrillation often recurs even with antiarrhythmic therapy and 20-30% of these patients will have systemic embolization if untreated. Systemic embolization in the presence of only mild to moderate disease is not an indication for surgery but should be treated with warfarin anticoagulation. Indications for intervention focus on symptoms such as an episode of pulmonary edema, a decline in exercise capacity, or any evidence of pulmonary hypertension (peak systolic pulmonary pressure greater than 50 mm Hg). Some experts believe that the presence of atrial fibrillation should also be a consideration for an intervention. Symptoms or evidence of pulmonary hyper tension should drive the decision to intervene in these patients, not the estimated valve area. Open mitral commissurotomy is now rarely performed and has given way to percutaneous balloon valvuloplasty. Ten-year follow-up data comparing surgery to balloon valvuloplasty suggest no real difference in outcome between the two modalities. Replacement of the valve is indicated when combined stenosis and regurgitation are present or when the mitral valve echo score is greater than 8-10. Repeat balloon valvuloplasty can be done if the morphology of the valve remains suitable. At surgery, a Maze procedure may be done at the same time to reduce recurrent atrial arrhythmias. It involves a number of endocardial incisions across the right and left atria to dis rupt the electrical activity that sustains atrial arrhythmias. Percutaneous balloon valvuloplasty is not effective when bioprosthetic valve stenosis occurs, but stented valve-in valve procedures have been successful and will likely be used more often. Younger patients and those with end stage kidney disease are generally believed to do least well with bioprosthetic heart valves, although data have ques tioned the role of chronic kidney disease as a major risk factor. Endocarditis prophylaxis is indicated for patients with prosthetic heart valves but is not indicated in native valve disease (see Tables 33-4, 33-5, and 33-6). General Considerations Mitral regurgitation places a volume load on the heart (increases preload) but reduces afterload. When to Refer · · Patients with mitral stenosis should be monitored with yearly examinations, and echocardiograms should be performed more frequently as the severity of the obstruction increases. All patients should initially be seen by a cardiologist, who can then decide how often the patient needs cardi ology follow-up. Clinically, mitral regurgita tion is characterized by a pansystolic murmur maximal at the apex, radiating to the axilla and occasionally to the base. The mitral regurgitation murmur due to mitral valve prolapse tends to radiate anteriorly in the presence of posterior leaflet prolapse and posteriorly when the prolapse is primarily of the anterior leaflet. Mitral regurgitation may not be pansystolic but occur only after the mitral click in patients with mitral valve prolapse (until late in the disease process when it becomes progressively more holosystolic). Patients with functional mitra l reg urgitation may improve with biventricular paci ng. Doppler tech niques provide qualitative and semiquantitative estimates of the severity of mitral regurgitation. Echocardiographic dimensions and measures of systolic function are critical in deciding the timing of surgery. Exercise hemodynamics with either Doppler echocardiography or cardiac catheteriza tion may be useful when the symptoms do not fit the ana tomic severity of mitral regurgitation. Pulmonary hypertension development suggests the mitral regurgitation is severe and should prompt intervention. Some patients may become hemodynamically unstable and can be initially treated with vasodilators or intra-aortic balloon counterpulsation, which reduce the amount of retro grade regurgitant flow by lowering systemic vascular resis tance. There is controversy regarding the role of afterload reduction in chronic mitral regurgitation, since the lesion inherently results in a reduction in afterload, and there are no data that chronic afterload reduction is effective. A height ened sympathetic state has led some experts to suggest that beta-blockade be considered routinely. The mitral regurgita tion in patients with tachycardia-related cardiomyopathy may also improve with normalization of the heart rate.
In this setting allergy nasal spray buy cheapest prednisolone, continuing and augmenting the topical anti-inflammatory treatment often improves the dermatitis despite the presence of infection. Guidelines of care for the man agement and treatment of atopic dermatitis with topical therapies. Silvery sca les on bright red, wel l-demarcated plaques, usua l ly on the knees, el bows, and sca lp. Nail findings including pitting and onycholysis (separation of the nail plate from the bed). Psoriasis patients are at increased risk for cardio vascular events, type 2 diabetes mellitus, meta bolic synd rome, and lymphoma. Eczema herpeticum, a generalized herpes simplex infection mani fested by monomorphic vesicles, crusts, or scalloped ero sions superimposed on atopic dermatitis or other extensive eczematous processes, is treated successfully with oral. General Considerations Psoriasis is a common benign, chronic inflammatory skin disease with both a genetic basis and known environmen tal triggers. Obesity worsens psoriasis, and significant weight loss in obese persons may lead to substantial improvement of their psoriasis. Eruptive (guttate) psoriasis consisting of myriad lesions 3 - 1 0 mm in diameter occurs occasionally after streptococcal pharyngitis. Rarely, grave, occasionally life-threatening forms (generalized pustular and erythrodermic psoriasis) may occur. Clin ical Findings There are often no symptoms, but itching may occur and be severe. Occasionally, only the flexures (axillae, inguinal areas) are involved (termed inverse psoriasis). Not all patients have findings in all locations, but the occurrence of a few may help make the diagnosis when other lesions are not typical. Some patients have mainly hand or foot dermatitis and only Nail pitting due to psoriasis. There may be associated arthritis that is most commonly distal and oligoarticular, although the rheumatoid variety with a negative rheuma toid factor may occur. The psychosocial impact of psoria sis is a major factor in determining the treatment of the patient. Differential Diagnosis the combination of red plaques with silvery scales on elbows and knees, with scaliness in the scalp or nail find ings, is diagnostic. Psoriasis lesions are well demarcated and affect extensor surfaces-in contrast to atopic derma titis, with poorly demarcated plaques in flexural distribu tion. In body folds, scraping and culture for Candida and examination of scalp and nails will distinguish "inverse psoriasis" from intertrigo and candidiasis. The cutaneous features of reactive arthritis, pityriasis rosea, systemic lupus erythematosus, and syphilis mimic psoriasis. Certain medications, such as beta-blockers, antimalarials, statins, and lithium, may flare or worsen psoriasis. Even tiny doses of systemic corticosteroids given to patients with psoriasis may lead to severe rebound flares of their disease when they are tapered. Patients with moderate to severe psoriasis should be man aged by or in conjunction with a dermatologist. Methotrexate is very effective for severe psoriasis in doses up to 25 mg once weekly. Administration of folic acid, 1-2 mg daily, can eliminate nausea caused by methotrexate without compromising efficacy. Acitretin, a synthetic retinoid, is most effective for pustu lar psoriasis in dosages of O. Because acitretin is a teratogen and persists for 2-3 years in fat, women of childbearing age must wait at least 3 years after completing acitretin treatment before considering pregnancy. When used as single agents, retinoids will flatten psoriatic plaques, but will rarely result in complete clearing. Cyclosporine dramatically improves psoriasis and may be used to control severe cases. Rapid relapse (rebound) is the rule after cessation of therapy, so another agent must be added if cyclosporine is stopped. Infliximab provides the most rapid response and can be used for severe pustular or erythro dermic flares. Etanercept is used more frequently for long term treatment at a dose of 50 mg twice weekly for 3 months, then 50 mg once weekly. The phosphodiesterase 4 inhibitor apremilast is an approved option for plaque-type psoriasis with minimal immuno suppressive effects. Given the large number of psoriasis treatments available, consultation with a dermatologist is recommended when considering systemic treatment for moderate to severe psoriasis. It is best to restrict the ultra-high potency corticosteroids to 2-3 weeks of twice-daily use and then use them in a pulse fashion three or four times on weekends or switch to a mid-potency corticosteroid. Addi tional measures are therefore commonly added to topical corticosteroid therapy. Initially, patients are treated with twice-daily corticosteroids plus a vitamin D analog twice daily. Calcipot riene usually cannot be applied to the groin or face because of irritation. Treatment of extensive psoriasis with vitamin D analogs may result in hypercalcemia, so that the maxi mum dose for calcipotriene is 100 g/week and for calcitriol is 200 g/week. Calcipotriene is incompatible with many topical corticosteroids (but not halobetasol), so if used concurrently, it must be applied at a different time.
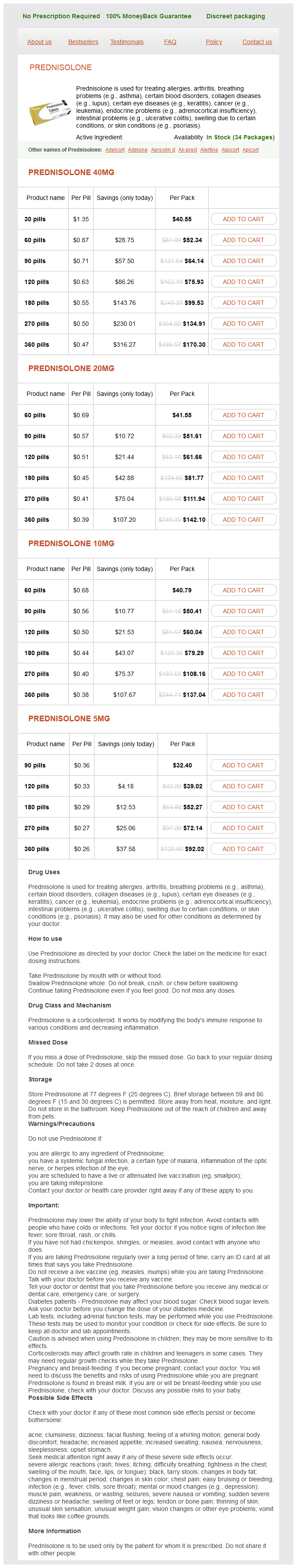
Prednisolone Dosage and Price
Prednisolone 40mg
- 30 pills - $40.55
- 60 pills - $52.34
- 90 pills - $64.14
- 120 pills - $75.93
- 180 pills - $99.53
- 270 pills - $134.91
- 360 pills - $170.30
Prednisolone 20mg
- 60 pills - $41.55
- 90 pills - $51.61
- 120 pills - $61.66
- 180 pills - $81.77
- 270 pills - $111.94
- 360 pills - $142.10
Prednisolone 10mg
- 60 pills - $40.79
- 90 pills - $50.41
- 120 pills - $60.04
- 180 pills - $79.29
- 270 pills - $108.16
- 360 pills - $137.04
Prednisolone 5mg
- 90 pills - $32.40
- 120 pills - $39.02
- 180 pills - $52.27
- 270 pills - $72.14
- 360 pills - $92.02
Eyes at risk for neovascular glaucoma following ischemic central retinal vein occlusion can be treated by panretinal laser photocoagulation prophylactically or as soon as there is evidence of neovascularization allergy blood test zyrtec prednisolone 40 mg with mastercard, the latter approach necessitating frequent monitoring. In branch retinal vein occlusion complicated by retinal neovascular ization, the ischemic retina should be laser photo coagulated. Intravitreal triamcinolone improves vision in chronic macular edema due to nonischemic central retinal vein occlusion, whereas an intravitreal implant containing dexamethasone is bene ficial in both central and branch retinal vein occlusion. Retinal laser photocoagulation may be indicated in chronic macular edema due to branch, but not central, retinal vein occlusion. General Considerations Central and branch retinal vein occlusion are common causes of acute loss of vision with branch being four times more common. The major predisposing factors are the etiologic factors associated with arteriosclerosis. Symptoms and Signs the visual impairment in central retinal vein occlusion is commonly first noticed upon waking. Ophthalmoscopic signs include widespread retinal hemorrhages, retinal venous dilation and tortuosity, retinal cotton-wool spots, and optic disk swelling. Prognosis In central retinal vein occlusion, severity of visual loss ini tially is a good guide to visual outcome. Visual outcome in branch retinal vein occlusion is determined by the severity of macular damage from hem orrhage, ischemia, or edema. Multiple branch retinal artery occlusions, which may be asymptomatic, along with encephalopathy and hearing loss are the characteristic features of Susac syndrome. Symptoms and Signs Central retinal artery occlusion presents as sudden pro found monocular visual loss. Visual acuity is usually reduced to counting fingers or worse, and visual field is restricted to an island of vision in the temporal field. The retinal arter ies are attenuated, and "box-car" segmentation of blood in the veins may be seen. The retinal swelling subsides over a period of 4-6 weeks, leaving a pale optic disk and attenuated arterioles. Branch retinal artery occlusion may also present with sudden loss of vision if the fovea is involved, but more commonly sudden loss of visual field is the presenting complaint. Fundal signs of retinal swelling and adjacent cotton-wool spots are limited to the area of retina supplied by the occluded artery. Identify risk factors for cardiac source of emboli includ ing arrhythmia, particularly atrial fibrillation, and cardiac valvular disease, and check the blood pressure. Clinical features of giant cell arteritis include age 50 years or older, j aw claudication (which is very specific), headache, scalp tenderness, general malaise, weight loss, symptoms of polymyalgia rheumatica, and tenderness, thickening, or absence of pulse of the superficial temporal arteries. When to Refer All patients with retinal vein occlusion should be referred urgently to an ophthalmologist. Drug treatment of macular oedema secondary to central retinal vein occlusion: a network meta-analysis. Risk factors for central and branch retinal vein occlu sian: a meta-analysis of published clinical data. Diagnostic ramifications of ocular vascular occlusion as a first thrombotic event associated with factor V Leiden and prothrombin gene heterozygosity. General Considerations In patients 50 years of age or older with central retinal artery occlusion, giant cell arteritis must be considered (see Ischemic Optic Neuropathy and Chapter 20). Otherwise, even if no retinal emboli are identified on ophthalmoscopy, urgent investigation for carotid and cardiac sources of emboli must be undertaken in central and particularly in branch retinal artery occlusion, so that timely treatment can be given to reduce the risk of stroke (see Chapters 12, 14, and 24). Diabetes mellitus, hyperlipidemia, and sys temic hypertension are common etiologic factors. Migraine, oral contraceptives, systemic vasculitis, congeni tal or acquired thrombophilia, and hyperhomocysteinemia are also causes, particularly in young patients. Internal carotid artery dissection should be considered especially when there is neck pain or a recent history of neck trauma. Acute centra l reti nal artery occlusion with cherry-red spot (arrow) and preserved retina (arrowheads) adjacent to the optic disk due to cilioreti nal a rtery supply. Laboratory Findings Erythrocyte sedimentation rate and C-reactive protein are usually markedly elevated in giant cell arteritis but one or both may be normal. Particularly in younger patients, consider testing for antiphospholipid antibodies, lupus anticoagulant, inherited thrombophilia, and elevated plasma homocysteine. When to Adm it Patients with visual loss due to giant cell arteritis may require emergency admission for high-dose corticosteroid therapy and close monitoring to ensure that treatment is adequate. Risk and risk periods for stroke and acute myocar dial infarction in patients with central retinal artery occlusion. Predictors of prognosis and treatment outcome in central retinal artery occlusion: local intra-arterial fibrinolysis vs. A review of central retinal artery occlusion: clinical presentation and management. Treatment If the patient is seen within a few hours after onset, emer gency treatment-including laying the patient flat, ocular massage, high concentrations of inhaled oxygen, intrave nous acetazolamide, and anterior chamber paracentesis may influence the visual outcome. In giant cell arteritis there is risk-highest in the first few days-of involvement of the other eye. When the diag nosis is suspected, high-dose corticosteroids (oral pred nisolone 1 - 1. A temporal artery biopsy should be performed promptly, and if neces sary, assistance should be sought from a rheumatologist. Patients with embolic retinal artery occlusion and 70-99% ipsilateral carotid artery stenosis and possibly those with 50-69% stenosis should be considered for carotid endarterectomy or possibly angioplasty with stenting to be performed within 2 weeks (see Chapters 1 2 and 24). Cardiac valvular disease and pat ent foramen ovale may require surgical treatment.