General Information about Prazosin
Like another medicine, prazosin also has potential side effects. Some of the widespread side effects embrace dizziness, drowsiness, headache, nausea, and constipation. These unwanted aspect effects are usually gentle and will go away because the body adjusts to the treatment. In some cases, prazosin may cause low blood pressure, particularly when first beginning the treatment or when the dosage is increased. This might lead to symptoms similar to fainting, dizziness, and weakness. It is important to consult a doctor if these signs persist or become severe.
Prazosin is a medication that belongs to a group of drugs known as alpha-blockers. It is usually used to deal with hypertension (hypertension) and to enhance signs of benign prostatic hyperplasia (BPH), a condition by which the prostate gland turns into enlarged, causing issue in urination. In this text, we will delve into the details of this versatile drug, the means it works, its makes use of, and potential unwanted effects.
In conclusion, prazosin is a commonly prescribed treatment for the remedy of hypertension and symptoms of BPH. Its ability to chill out blood vessels and muscular tissues around the urethra makes it an efficient drug for these circumstances. However, it's essential to comply with the dosage directions carefully and seek the assistance of a health care provider if any unwanted effects are skilled. With proper use, prazosin can considerably improve the standard of life for people suffering from hypertension and BPH.
Prazosin is available in the type of tablets and is usually prescribed to be taken a few times a day, relying on the situation being treated. It is important to take it at the identical time each day to maintain a consistent degree of the drug within the body. The dosage may differ relying on the patient's age, medical historical past, and response to therapy, and should be determined by a health care provider.
Prazosin shouldn't be taken by pregnant ladies or those making an attempt to conceive, as it may cause hurt to the unborn child. It is also not beneficial for individuals with liver or kidney illness, as they may have a better threat of experiencing unwanted effects.
Prazosin can also be commonly prescribed to alleviate the symptoms of BPH, which embrace difficulty in starting urination, weak urine circulate, and the want to urinate incessantly. It helps to chill out the muscles within the bladder and the prostate, making it easier to urinate. It could take up to 6 weeks to see the full benefits, and it is crucial to keep taking the medication, as stopping it abruptly may cause a sudden enhance in blood stress.
Prazosin works by blocking the motion of a chemical referred to as norepinephrine within the body. Norepinephrine is a hormone and neurotransmitter that's answerable for inflicting blood vessels to slender and the muscular tissues across the urethra to contract. By inhibiting this chemical, prazosin causes the blood vessels to chill out, allowing for easy blood circulate and subsequently decreasing blood pressure. It also helps to loosen up the muscle tissue around the urethra, reducing the obstruction and bettering the flow of urine.
The most typical use of prazosin is for the remedy of hypertension. When prescribed for this objective, it ought to be taken frequently, even when the person feels nicely, as it has been shown to decrease the chance of stroke and heart attack. It may take a few weeks to see the complete results of the medication, and it is important to proceed taking it as directed, except suggested otherwise by a doctor.
Details of positioning the patient cholesterol and food labels buy 2.5 mg prazosin amex, incision, exposure, surgical details (having done this before I was able answer the details of this). History, examination looking for common sites of origin (prompted decreased air entry on left lower lobe), investigation, local and distant staging. Had been inadequately resuscitated and also had open femoral fracture which I picked up from history/examination and secondary survey. Smith Petersen: describe the approach, including incision, internervous plane, structures at risk, etc. Basic science oral General comments `The examiners managed to take me through a huge amount in 15 min, scratching the surface to seemingly check I could say something about everything. Spent the first 15 min of viva chatting about laminar flow, theatre design, theatre discipline, antibiotic prophylaxis, ring fencing elective beds, washing hands. Wedges for reconstruction of tibial defect; how wedges work; why wedges and not cement for build up, etc. What is the metal of screw, what metals can be used, metal allergy, modulus of elasticity, etc. Given two types of self-tapping screws (one normal, one reverse cutting as well as self-tapping) describe these implants. Materials Explain how you would choose your ideal knee arthroplasty implant and why. Arthroplasty Given fractured femoral component of Oxford partial knee arthroplasty and worn tibial component. In depth basic science about stress risers and fatigue of metal (anterior well cemented, posterior not), interdigitation of cement, etc. Cement Picture of broken cement mantle reasons for this, mantle thickness, asked what would you inform your juniors too little or too much cement How to make it extensile Approaches to hip: had to list them and then when I got to anterior had to describe in detail Anterior approaches to knee: step-by-step. All, including anterolateral, where do you use them what are advantages and disadvantages etc. Axial midthigh transection label muscles/nerves/vessels Axial midtibial transection label muscles/nerves/vessels. If you are designing a test, what would you want it to be sensitive or specific Asked to draw a graph of bacterial multiplication (time versus bacterial growth) Does your hospital have an infection control policy Shown a slide of plated agar with inoculation and antibiotic sensitivities test what is this, which is sensitive Describe the mechanism of action of antibiotics in relation to this picture bell went! Relative/absolute stability Slide of diaphyseal fracture with callus formation asked about primary and secondary bone healing, types of callus, cutting cones. Stressstrain curve label all the points, axis and nomenclature and describe what the areas underneath signify. Pick three items from a display in front of me that match those stressstrain curves. Hand and paediatric oral General points `The paeds examiner repeatedly said things like: "the mother is very concerned about the appearance she wants something done". How would you manage from first meeting the child to definitive stabilization (everything). I was asked about associations and eventually realized that the examiner wanted to talk about leg length discrepancy. In severe cases of the slip, this might be impossible, hence the indication for open reduction (there is still some controversy about this). I fell in to the trap of doing a closed reduction after 4 weeks of an irreducible hip wrong! Wanted to hear emergency and surgical approach in detail splint afterwards re anterior dislocation if capsule left open. Gallows traction Picture what is it, what is it used for, from what age you should not use it and why Clinical picture then X-ray diagnosis, management, risk of cancer, Maffucci, etc. Counsel parents on the risk of transmission Genu valgum 3-year-old: discussion of pathological/normal and management. Radial club hand Classification of upper limb congenital abnormalities (aplasias): transverse/longitudinal, pre/postaxial/central, etc. A sketch of the hand with a flexor aspect wound principles of exploration, extension, tendon repair. Pho to of hand, swollen and lots of little ragged wounds (dog bite): assessment, size of skin wounds belies underlying damage, check tendons, collection. I expressed concerns of flexor sheath infection and proceeded to mention six cardinal signs of Kanavel (there are only four! This was a farmyard injury, talked about management of laceration (wound toilet, toxoid, tetanus immunoglobulins and antibiotics) and management of the flexor tendon repair. Discussion about carpal instability patterns, then how would you treat volar dislocation of lunate. I initially went down the line of infection and osteomyelitis before realizing this was a malignancy. Pathology and adult reconstruction oral General comments `This was the only time in the entire exam I was asked about a classification system! Likely cause talked out my thought process and they were happy nerve root comes out below pedicle so L4/5 disc or L3/4 far lateral. What is the differential diagnosis, what is most likely cause in a 60-year-old patient Fortunately I discovered it was a renal cell metastasis before discussing nailing! Multiple myeloma: presented as fracture through cystic lesion of greater trochanter. Non-union femoral neck and shaft A bit complicated talked about valgus osteotomy proximal femur, possible strategies to manage shaft non-union at same time. Sessile osteochondroma of humerus Clinical examination, diaphyseal achalasia, incidence of malignant transformation in both, clues to malignant transformation (increase in size, pain, etc. I mentioned need to exclude infection so this led to further discussion re Ix for infected implants (bloods, imaging, bone scan timing, etc. Further management re-fuse with bone graft (discussed different graft options) or excision arthroplasty (discussed pros and cons).
Fracture description Always look at two orthogonal views that are well centred determination of cholesterol in eggs buy prazosin american express, adequate, with good exposure and of the correct patient. There is no role for prosthetic replacement unless radiographs show associated advanced osteoarthritis. For example, femoral shaft fracture patella fracture, femoral neck fracture and hip dislocation Closed reduction technique on a fracture table, gentle flexion, adduction, axial traction and hip is brought back in to extension and abduction, maintaining traction (Leadbetter technique), and reduction is assessed clinically by heels on palm test and by image intensifier. Whichever technique is used, it should be minimally traumatic to avoid further damage to the femoral head blood supply. Repeated attempts at closed reduction could increase the risk of damage to the femoral head blood supply. Open reduction technique anterolateral approach and use K-wire in the femoral head as a joystick to reduce the fracture. Definitive treatment is with cannulated screws or a sliding hip screw with derotation screw. Short- or long-threaded screws do not seem to make any difference in fracture healing. Furthermore, there are several other factors involved in the development of avascular necrosis: initial fracture displacement causing damage to blood supply, quality of fracture reduction or loss of reduction post surgery and fracture non-union. Follow up for at least 2 years to assess for radiological features of avascular necrosis of femoral head. Management options Serious complications Loss of reduction and implant failure Avascular necrosis of femoral head 6. Type I a trial of non-operative management, percutaneous cannulated screws fixation, two-holed sliding hip screw with a derotation screw. Management principles are to rule out infection, revise the fixation by open reduction, valgus trochanteric osteotomy and stabilize with a 135 -angled blade plate with or without bone graft. Management of femoral head avascular necrosis is given in the adult pathology section. Management principles are to rule out infection, valgus trochanteric osteotomy, stabilization with 135 -angled blade plate and bone graft. If fixation is deemed to be sound, then there is the option of augmenting fracture healing with bone graft or vascularized quadratus femoris bone graft. Managing complications of femoral neck fracture fixation should be undertaken by a subspecialist, but principles of that management should be discussed. Cemented hemiarthroplasty is preferred over uncemented hemiarthroplasty owing to reduced anterior thigh pain as the stem is secured to the femoral shaft. However, it increases the risk of cardiopulmonary dysfunction and revision surgery is more demanding. Uncemented hemiarthroplasty is performed in patients with very limited mobility and significant cardiopulmonary disease. Complications Complications of internal fixation are infection, avascular necrosis of the femoral head, non-union, implant failure and increased rate of revision surgery. Femoral neck fracture associated with femoral shaft fracture Typical history motor vehicle accident About 5% of femoral shaft fractures are associated with femoral neck fractures 399 Section 7: the trauma oral Radiological assessment any femoral shaft fracture should always be assessed for associated femoral neck fracture or knee fractures or hip dislocation. Options Single device to stabilize both fractures or two separate devices for each fracture: Single device cephalomedullary nail (trochanteric entry point) one or two screws in to femoral head does not matter but make sure that femoral shaft fracture is not distracted. The disadvantage with use of a single device to stabilize both fractures is the displacement of either of the fractures while introducing the nail4 Two devices cannulated screws or sliding hip screw for femoral neck fracture and retrograde nail for femoral shaft fracture. If the femoral neck fracture is displaced or displaces when nail fixation is performed, open reduction may be required as manipulation would usually be futile. At the end of the procedure, always assess the knee joint for ligamentous integrity. Postoperative rehabilitation varies from nonweightbearing for 6 weeks to weightbearing as tolerated straight away. External fixation can be safely converted to nail fixation for up to 2 weeks without increased risk of infection. If the hip joint cannot be manipulated, then open reduction is performed depending on the direction of dislocation. For anterior dislocation, a Smith Peterson approach is used; posterior dislocation requires a posterior approach. Postoperative rehabilitation after nail fixation allows weightbearing as tolerated; after plate fixation there is no weightbearing for up to 34 months. Assess for posterior or anterior acetabular wall fracture, femoral head or neck or shaft fracture, patellar fractures. If there are large intra-articular fragments, definitive open debridement could be planned. Femoral shaft fracture with hip dislocation Typical history motor vehicle accident, fall from motor cycle, fall from height Radiological assessment direction of hip dislocation, level and type of femoral shaft fracture, rule out any associated femoral neck fracture or acetabular fracture. Posterior dislocation of hip (Thompson and Epstein classification) Management Initial Thomas splint, analgesia, frequent assessment for sciatic nerve and distal vascular status. Definitive management Requires urgent closed reduction and skin or skeletal traction. Reduction of anterior hip dislocation is by axial and lateral traction and posterior hip dislocation is reduced by axial traction with the hip in adduction and internal rotation. Assessment for instability is by figure-of-four for anterior dislocation and flexion with adduction and axial loading for posterior dislocation. If closed reduction fails, then open reduction is carried out depending on the direction of dislocation. If closed reduction is not possible, which is often the case, then a couple of Schanz pins are inserted in to the proximal femoral fragment in the linea aspera, avoiding the femoral canal if possible.
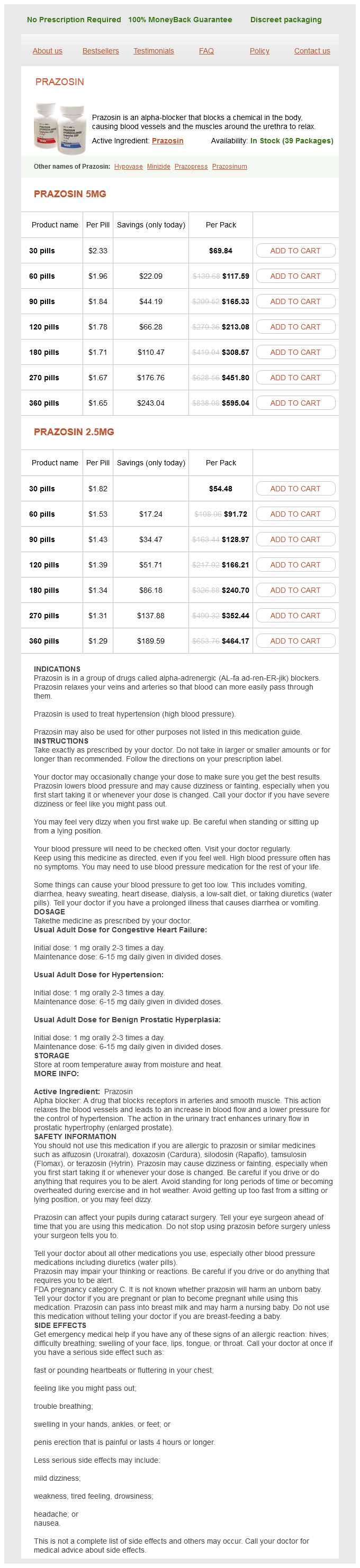
Prazosin Dosage and Price
Prazosin 5mg
- 30 pills - $69.84
- 60 pills - $117.59
- 90 pills - $165.33
- 120 pills - $213.08
- 180 pills - $308.57
- 270 pills - $451.80
- 360 pills - $595.04
Prazosin 2.5mg
- 30 pills - $54.48
- 60 pills - $91.72
- 90 pills - $128.97
- 120 pills - $166.21
- 180 pills - $240.70
- 270 pills - $352.44
- 360 pills - $464.17
Furthermore cholesterol medication nightmares generic 2.5 mg prazosin fast delivery, make sure that the instrument pierces the capsule posteriorly rather than posterolaterally because otherwise the full thickness of the trochanter with the insertions of the gluteus medius and minimus will not be removed. Osteotomize the trochanter with a Gigli saw and reflect it upwards with the attached gluteus medius and minimus muscles. Retract the trochanter with attached gluteus medius and minimus and the underlying capsule posteriorly. Longitudinal incision in to the capsule of the hip joint Dislocate the hip by adducting the thigh and, to a lesser extent, by external rotation. After the hip has been dislocated use a Gigli saw to perform an osteotomy of the femoral neck. Trochanteric approach Advantages Excellent exposure of acetabulum and proximal femur. Disadvantages Increased bleeding Trochanteric bursitis Technical difficulty wiring back the trochanter Wire breakage and non-union of the trochanter. Position the patient is positioned supine, close to edge of the operating table so that the buttock hangs over the sandbag under the buttock. Extensile approach the skin incision can be extended down the lateral aspect of the thigh, splitting vastus lateralis to gain access to the lateral aspect of the femur. This makes the greater trochanter more prominent and moves the tensor fascia lata anteriorly. A straight 15-cm longitudinal incision is made, centred on the tip of the greater trochanter. The incision crosses the posterior third of the trochanter before running down the shaft of the femur. Advantages Easier No damage to the hip abductors Good access to the femur and particularly the acetabulum. Place a retractor deep to gluteus medius and minimus and bluntly dissect the fat pad off the anterior portion of the joint capsule. Gluteus maximus Gluteus medius Piriformis Gemelli Obturator externus Quadratus femoris Fascia lata Obturator internus Sciatic nerve Position Lateral position, affected limb uppermost. When the leg is straightened, the incision is curved Alternatively, a 1520-cm curved incision centred over the posterior aspect of the greater trochanter. Internervous plane There is no true internervous plane as the gluteus maximus is split in the line of its fibres, but is not significantly denervated because its nerve supply is well medial to the split. Superficial surgical dissection Incise fascia lata on the lateral aspect of the femur to uncover the vastus lateralis. Retract the split edges of fascia lata and gluteus maximus with a Charnley bow retractor. The short external rotators of the hip lie under a layer of fat; a useful landmark to locate them is the posterior border of the gluteus medius. Internally rotate the leg to put the short external rotators on stretch and to pull the operative field away from the sciatic nerve. Identify and protect the sciatic nerve lying on the short external rotators encased in fatty tissue. Identify piriformis and detach it sharply with a scalpel fairly close to the femur origin or you may have difficulty reattaching it at the end of the procedure. Detach the muscles close to their femoral insertions and reflect them backwards, laying them over the sciatic nerve. Try not to detach all of quadratus femoris if possible as the muscle contains vessels from the lateral circumflex artery, which can cause persistent bleeding. The capsule of the hip joint is now exposed and can be excised with a T-shaped incision. The exposure can be extended distally by detaching all of quadratus femoris and inserting the gluteus maximus tendon on to the proximal femur. It can be further extended by dissecting behind the vastus lateralis to expose a fracture or to perform an extended trochanteric osteotomy (osteotomize one-third of the lateral femur to a length of 1214 cm from the tip of the greater trochanter). The posterior column can be reached by dissecting behind the gluteus medius at the proximal extent of the exposure. Structures at risk Sciatic nerve Branches of the inferior gluteal artery are invariably injured when the gluteus maximus is separated. Mention your own preferred incision if asked by the Deep surgical dissection the short external rotators are seen on the posterolateral aspect of the femur (piriformis, superior gemellus, obturator internus, inferior gemellus, quadratus femoris). Mentioning the different variations described may unnecessarily complicate your answer and confuse the examiners. Structures at risk the anterior and posterior branches of the obturator nerve lie on either side of adductor brevis and are at risk during the dissection. The medial femoral circumflex artery passes around the medial side of the distal part of the psoas tendon; it is in danger, especially in children, if the psoas tendon is not isolated and cut under direct vision. Position the patient is positioned supine with the affected hip flexed, abducted and externally rotated. The sole of the foot on the affected side should lie along the medial side of the contralateral knee. Incision A longitudinal incision is made which is 1520 cm in length and centred over the greater trochanter. Deep dissection is in the plane between the gluteus medius (superior gluteal nerve) and piriformis (n. Superficial surgical dissection Incision A longitudinal incision is made on the medial side of the thigh starting at a point 3 cm below the pubic tubercle. The incision runs down over the adductor longus as long as is required for exposure of the femur. A Charnley bow retractor is inserted in to the anterior and posterior borders of the fascia lata.