General Information about Pepcid
Pepcid has been confirmed efficient within the treatment of a variety of circumstances related to abdomen acid, including gastric and duodenal ulcers, hyperacidity, and heartburn related to hyperchlorhydria. It can be used in the management of symptomatic and stress-induced ulcers of the gastrointestinal tract. This huge scope of usage is a testomony to the effectiveness of Pepcid in bettering the well being and functioning of the abdomen and its protecting mechanisms.
The really helpful dosage of Pepcid can vary relying on the particular condition being treated. It is available in varied forms, including oral tablets, suspension, and injections, making it convenient for sufferers to take as prescribed. It is mostly well-tolerated and has a low danger of side effects when taken accurately. However, like all medication, it is essential to observe the directions of your physician or pharmacist and inform them of any existing medical situations or medicines that you're taking.
One of the essential roles of gastric mucosa is to protect the abdomen from its own acidic environment. When this protective layer is broken, it can result in the formation of gastric ulcers. Pepcid plays a major position in enhancing the protective mechanisms of the gastric mucosa by increasing the manufacturing of gastric mucus and glycoproteins. These substances act as a physical barrier between the abdomen lining and the acidic gastric juices, preventing the formation of ulcers.
The major motion of Pepcid is to dam the H2 receptors located on the surface of sure cells in the stomach. These receptors are responsible for stimulating the production of stomach acid, which can lead to digestive problems. By blocking these receptors, Pepcid reduces the manufacturing of acid, offering reduction to those affected by hyperacidity and heartburn.
In conclusion, Pepcid is a vital medication within the remedy of gastric ulcers, hyperacidity, and different digestive disorders. It works by enhancing the protective mechanisms of the gastric mucosa, selling therapeutic, and stopping additional harm to the stomach. With its confirmed effectiveness and minimal unwanted facet effects, Pepcid is a trusted alternative for tens of millions of people battling gastrointestinal issues. If you might be experiencing any of the situations mentioned above, consult your doctor to see if Pepcid is the best option for you.
Moreover, Pepcid also stimulates the secretion of bicarbonate – a natural acid neutralizer, and endogenous prostaglandins, which are answerable for repairing and healing the injured gastric mucosa. This is particularly beneficial in the case of stress ulcers, where the constant psychological or physical stress can significantly injury the gastric lining. By selling therapeutic of those accidents, Pepcid also can stop the event of extra extreme situations, corresponding to scarring of the gastric mucosa or gastrointestinal bleeding.
Pepcid is a medicine commonly used for the therapy of various conditions related to the gastrointestinal tract. It is a member of the H2 receptor antagonist family and is understood for its capability to reinforce the protecting mechanisms of the gastric mucosa. It is extensively utilized by medical doctors and patients alike for its effectiveness in combating gastric ulcers, hyperacidity, heartburn, and other gastrointestinal issues.
The methyltetrahydrofolate then is trapped by the lack of sufficient vitamin B12 to accept and transfer methyl groups symptoms carpal tunnel pepcid 40mg with visa, and subsequent steps in folate metabolism that require tetrahydrofolate are deprived of substrate. This process provides a common basis for the development of megaloblastic anemia with deficiency of either vitamin B12 or folic acid. The mechanisms responsible for the neurological lesions of vitamin B12 deficiency are less well understood (Solomon, 2007). The terms vitamin B12 and cyanocobalamin are used interchangeably as generic terms for all of the cobamides active in humans. Methylcobalamin is required for the conversion of homocysteine to methionine and its derivative S-adenosylmethionine. When the vitamin B12intrinsic factor complex reaches the ileum, it interacts with a receptor on the mucosal cell surface and is actively transported into circulation. Antibodies to parietal cells or intrinsic factor complex also can play a prominent role in producing a deficiency. Several intestinal conditions can interfere with absorption, including pancreatic disorders (loss of pancreatic protease secretion), bacterial overgrowth, intestinal parasites, sprue, and localized damage to ileal mucosal cells by disease or as a result of surgery. The supply of vitamin B12 available for tissues is Vitamin B12 and Human Health Metabolic Functions. Vitamin B12 Deficiency the plasma concentration of vitamin B12 is the best routine measure of B12 deficiency and normally ranges from 150 to 660 pM (~200900 pg/mL). Inasmuch as the vitamin B12 bound to these transport proteins is relatively unavailable to cells, tissues can become deficient when the concentration of vitamin B12 in plasma is normal or even high. Once a hematopoietic stem cell is committed to enter a programmed series of cell divisions, the defect in chromosomal replication results in an inability of maturing cells to complete nuclear divisions while cytoplasmic maturation continues at a relatively normal rate. This results in the production of morphologically abnormal cells and death of cells during maturation, a phenomenon referred to as ineffective hematopoiesis. In managing a patient with severe megaloblastic anemia, a therapeutic trial using very small doses of the vitamin can be used to confirm the diagnosis. Vitamin B12 has an undeserved reputation as a health tonic and has been used for a number of disease states. Although the combination of oral vitamin B12 and intrinsic factor would appear to be ideal for patients with an intrinsic factor deficiency, such preparations are not reliable. Vitamin B12 is available for injection or oral administration; combinations with other vitamins and minerals also can be given orally or parenterally. The treatment of choice for vitamin B12 deficiency is cyanocobalamin administered by intramuscular or subcutaneous injection, never intravenously. Effective use of the vitamin B12 depends on accurate diagnosis and an understanding of the following general principles of therapy: · Vitamin B12 should be given prophylactically only when there is a reasonable probability that a deficiency exists or will exist. The initial diagnosis usually is suggested by macrocytic anemia or an unexplained neuropsychiatric disorder. Such patients require supplemental blood transfusions and immediate therapy with folic acid and vitamin B12 to guarantee rapid recovery. If there is an additional illness or a condition that may increase the requirement for the vitamin. The first objective hematologic change is the disappearance of the megaloblastic morphology of the marrow. Full correction of precursor maturation in marrow with production of an increased number of reticulocytes begins about the second or third day and peaks 35 days later. The degree and rate of improvement of neurological signs and symptoms depend on the severity and the duration of the abnormalities. When a defect has been present for many months or years, full return to normal function may never occur. After absorption, PteGlu is rapidly reduced at the 5, 6, 7, and 8 positions to tetrahydrofolic acid (H4PteGlu), which then acts as an acceptor of a number of one-carbon units. This reaction requires tetrahydrofolate as an acceptor of a methylene group from serine and uses pyridoxal phosphate as a cofactor. In uncomplicated pernicious anemia, in which the abnormality is restricted to a mild or moderate anemia without leukopenia, thrombocytopenia, or neurological signs or symptoms, the administration of vitamin B12 alone will suffice. In this situation, a therapeutic trial with small amounts of parenteral vitamin B12 (110 g per day) can confirm the presence of an uncomplicated vitamin B12 deficiency. In contrast, patients with neurological changes or severe leukopenia or thrombocytopenia associated with infection or bleeding require emergency treatment. X represents additional residues of glutamate; polyglutamates are the storage and active forms of the vitamin. This pathway may provide 200 g or more of folate each day for recirculation to tissues. Many food sources are rich in folates, espe- eases of the small intestine that interferes with the absorption of folate cially fresh green vegetables, liver, yeast, and some fruits. However, lengthy cooking can destroy up to 90% of the folate content of such food. Folate supplementation also is being considered in patients with elevated levels of plasma homocysteine. Folates present in food are largely in the form of reduced polyglutamates, and absorption requires transport and the action of a pteroylglutamyl carboxypeptidase associated with mucosal cell membranes. Because most absorption occurs in the proximal portion of the small intestine, it is not unusual for folate deficiency to occur when the jejunum is diseased.
A major concern for folate deficiency is in pregnancy where the folate requirement is increased and inadequate folic acid intake results in low birth rates and neural tube defects medicine used to stop contractions cheap pepcid 20 mg on line. Alcohol intake compounds the problem by increasing urinary folate excretion, impeding liver storage of folate, and decreasing folate absorption, which occurs primarily in the duodenum and jejunum. Some medications, such as methotrexate and trimethoprim, cause folate deficiency by altering its metabolism. The measurement of serum folate level is very sensitive to recent folate intake and thus testing should be performed on fasting samples. Although some have advocated for the use of red cell folate as a more accurate indicator of long-term folate storage, this test has a number of analytical issues (including high coefficient of variation) that make it of limited value; published studies have shown that red cell folate performs no better than fasting serum folate measurements. Vitamin B12 is the common name for either cyanocobalamin or hydroxycobalamin; these compounds are cobalamins, which include a group of molecules with a central cobalt atom bound by tetrapyrrole rings. In serum, methylcobalamin is the major form, whereas deoxyadenosylcobalamin is the primary form found in the cytosol. Cobalamins are not synthesized by humans but must be acquired in the diet, mainly meat, poultry, seafood, and dairy. The recommended daily allowance of cobalamins is 5 g, and the total body content is about 2 to 5 mg, about 1 mg being present in the liver. Because the daily losses are minute, cobalamin deficiency from diet alone takes years and occurs almost exclusively in strict vegetarians. Therefore, in adults, the main cause of vitamin B12 deficiency is impaired absorption. Food cobalamin binds to a substance in gastric juice called R protein (haptocorrin) and is released by pancreatic enzymes when it reaches the second portion of the duodenum. Vitamin B12 then binds to intrinsic factor, a glycoprotein produced by the parietal cells in the fundus and cardia of the stomach, and the complex then travels to the distal ileum. Intrinsic factor receptors are present on the ileal mucosa, especially in the terminal ileum, where cobalamin is specifically absorbed from the cobalamin-intrinsic factor complex in a receptor-mediated process. The latter disorder, pernicious anemia, occurs primarily in older adults, often with a family history of the disease; northern European descent; or concurrent 151 radiologyme. About 90% of patients with pernicious anemia have antibodies to parietal cells, compared with 5% in the general population, and approximately 60% have antibodies to intrinsic factor, which are rare in healthy people. Malabsorption of cobalamin also can occur with pancreatic insufficiency, when inadequate pancreatic enzymes fail to release cobalamin from the R proteins. Another cause of cobalamin deficiency is its consumption in the small intestine by a fish tapeworm, Diphyllobothrium latum, found mostly in fish from Canada, Alaska, and the Baltic Sea, and acquired by humans by eating undercooked fish or fish roe. Excessive intestinal bacteria in diseases associated with impaired motility, or intestinal stasis, such as systemic sclerosis, extensive diverticula, or surgical blind loops, also can consume enough cobalamin to cause vitamin B12related macrocytic anemia. The Schilling test had previously been used to help distinguish among the causes of cobalamin deficiency. Unfortunately, because of technical difficulties producing and measuring the cobalt radioisotopes required, this test is no longer available in the United States. These assays typically first convert serum cobalamins to cyanocobalamin and then quantify this species. Homocysteine is increased in both vitamin B12 and folate deficiency because methionine synthesis is impaired by deficiency of either. This testing has higher sensitivity because the increase occurs earlier in nutritional deficiency. When both are elevated, cobalamin deficiency is confirmed, although concurrent folate deficiency is possible. If cobalamin deficiency is present, the presence of antibody against intrinsic factor confirms the diagnosis of pernicious anemia. Another source of mild macrocytosis is reticulocytosis, an increase in young erythrocytes released early from the marrow, in hemolysis. The presence of a few reticulocytes is common on normal smears, but numerous polychromatophilic cells, representing a stress erythropoiesis, can result in mild macrocytosis. The cause may be deficiency of folic acid or vitamin B12 due to poor nutrition, but this anemia 152 radiologyme. In addition, there are a number of inherited dyserythropoietic anemias or marrow failure states, which are characterized by macrocytosis, such as Fanconi syndrome, dyskeratosis congenita, or congenital dyserythropoietic anemia. However, marrow erythropoiesis may be inadequate in normocytic anemias due to intrinsic bone marrow disease, insufficient iron availability, or inadequate erythropoietin effect. Insufficient iron availability results from either absence of iron (iron deficiency) or from poor iron utilization (such as during inflammatory states). Anemia of Chronic Renal Disease Anemia typically occurs with chronic renal disease only after the creatinine clearance decreases below 40 mL/min, which corresponds to a serum creatinine of about 2. Studies have shown that anemia of chronic renal disease can be more accurately assessed with cystatin C compared to creatinine. The anemia tends to worsen as the renal function decreases, but it usually stabilizes at a hematocrit of 15% to 30%. The cause of the kidney disease is not usually important in determining the severity of anemia, but anemia is typically less severe with polycystic kidney disease possibly due to erythropoietin production by the renal cyst epithelial cells. Several factors contribute to the anemia of chronic renal disease, the most important, however, being inadequate renal production of erythropoietin, a glycoprotein hormone synthesized in the kidney and responsible for the proliferation, maturation, and differentiation of erythrocytes in the bone marrow. In addition, red cell survival is shortened in uremia, and various toxins ordinarily excreted by the kidney accumulate in the serum and appear to depress erythropoiesis.
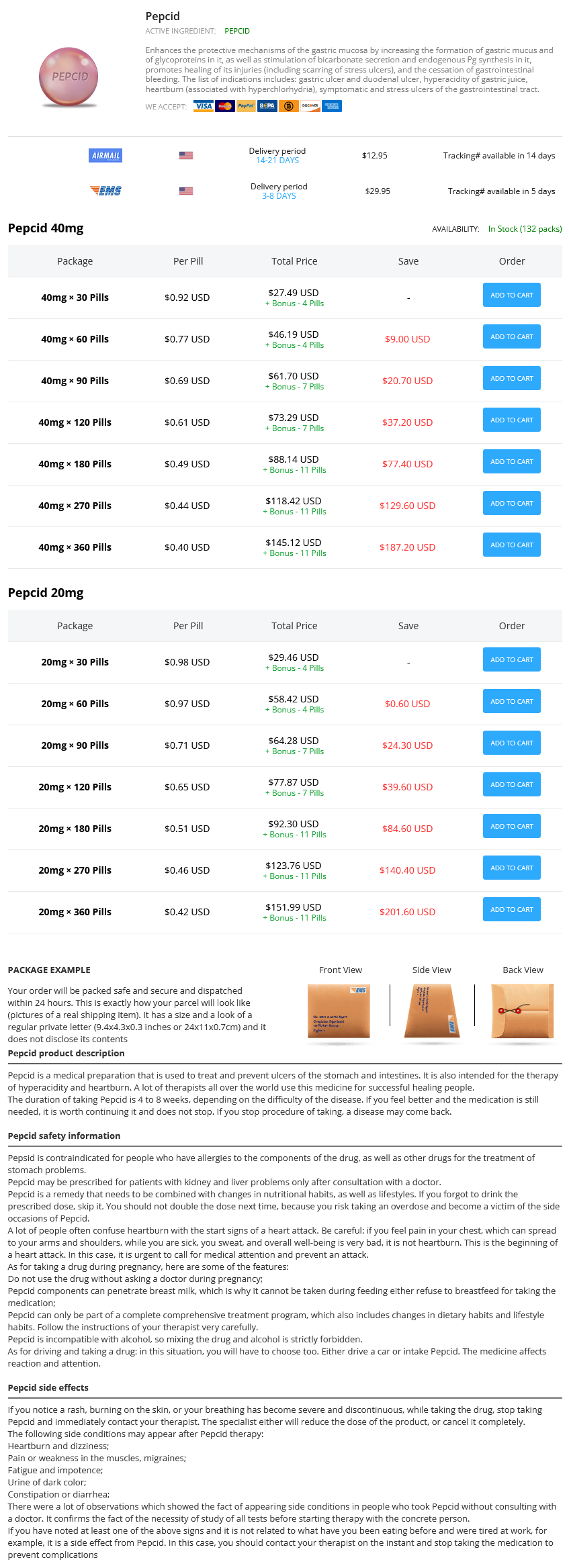
Pepcid Dosage and Price
Pepcid 40mg
- 30 pills - $27.49
- 60 pills - $46.19
- 90 pills - $61.70
- 120 pills - $73.29
- 180 pills - $88.14
- 270 pills - $118.42
- 360 pills - $145.12
Pepcid 20mg
- 30 pills - $29.46
- 60 pills - $58.42
- 90 pills - $64.28
- 120 pills - $77.87
- 180 pills - $92.30
- 270 pills - $123.76
- 360 pills - $151.99
Frequent measurement of plasma lidocaine concentration and dose adjustment to ensure that plasma concentrations remain within the therapeutic range (1 medications safe in pregnancy buy pepcid with a visa. These findings may explain why some patients require and tolerate higher-than-usual total plasma lidocaine concentrations to maintain antiarrhythmic efficacy. In atrial fibrillation, the conversion rate is lower in those in whom the arrhythmia has been present for weeks or months compared with those in whom it has been present for days. The major toxicity with ibutilide is torsades de pointes, which occurs in up to 6% of patients and requires immediate cardioversion in up to one-third of these. Therefore, lidocaine no longer is administered routinely to all patients in coronary care units. In vitro studies suggested that lidocaine-induced block reflects an increased likelihood that the Na+ channel protein assumes a nonconducting conformation in the presence of drug (Balser et al. In some studies, lidocaine increased current through inward rectifier channels, but the clinical significance of this effect is not known. Lidocaine can hyperpolarize Purkinje fibers depolarized by low [K]o or stretch; the resulting increased conduction velocity may be antiarrhythmic in reentry. Lidocaine decreases automaticity by reducing the slope of phase 4 and altering the threshold for excitability. While oral Mg2+ supplements may be useful in preventing hypomagnesemia, there is no evidence that chronic Mg2+ ingestion exerts a direct antiarrhythmic action. Procainamide is eliminated rapidly (t1/2 ~ 34 h) by both renal excretion of unchanged drug and hepatic metabolism. N-Acetyl procainamide is eliminated by renal excretion (t1/2 ~ 610 h) and is not significantly converted back to procainamide. Because of the relatively rapid elimination rates of both the parent drug and its major metabolite, oral procainamide usually is administered as a slow-release formulation. In patients with renal failure, procainamide or N-acetyl procainamide can accumulate to potentially toxic plasma concentrations. Clinical Pharmacokinetics Mexiletine Mexiletine is an analogue of lidocaine that has been modified to reduce first-pass hepatic metabolism and permit chronic oral therapy. Mexiletine is approved for treating ventricular arrhythmias; combinations of mexiletine with quinidine or sotalol may increase efficacy while reducing adverse effects. Loading and maintenance intravenous infusions are used in the acute therapy of many supraventricular and ventricular arrhythmias. The major metabolite, N-acetyl procainamide, lacks the Na+ channelblocking activity of the parent drug but is equipotent in prolonging action potentials. Dose-related nausea is frequent during oral therapy and may be attributable in part to high plasma concentrations of N-acetyl procainamide. During long-term therapy, most patients will develop biochemical evidence of the drug-induced lupus syndrome, such as circulating antinuclear antibodies. Therapy need not be interrupted merely because of the presence of antinuclear antibodies. Other symptoms of lupus, including pericarditis with tamponade, can occur, although renal involvement is unusual. The lupus-like symptoms resolve on cessation of therapy Propafenone Propafenone is a Na+ channel blocker with a relatively slow time constant for recovery from block (Funck-Brentano et al. Its major electrophysiological effect is to slow conduction in fast-response tissues. Chronic therapy with oral propafenone is used to maintain sinus rhythm in patients with supraventricular tachycardias, including atrial fibrillation; like other Na+ channel blockers, it also can be used in ventricular arrhythmias, but with only modest efficacy. In most subjects ("extensive metabolizers"), propafenone undergoes extensive first-pass hepatic metabolism to 5-hydroxy propafenone, a metabolite equipotent to propafenone as a Na+ channel blocker but much less potent as a adrenergic receptor antagonist. In extensive metabolizer subjects receiving such drugs or in poor metabolizer subjects, plasma propafenone concentrations of more than 1 g/mL are associated with clinical effects of adrenergic receptor blockade, such as reduction of exercise heart rate. It is recommended that dosage in patients with moderate-to-severe liver disease should be reduced to approximately 20%30% of the usual dose, with careful monitoring. In contrast to other adverse responses to quinidine therapy, cinchonism usually is related to elevated plasma quinidine concentrations and can be managed by dose reduction. Studies in the early 20th century identified quinidine, a diastereomer of the antimalarial quinine, as the most potent of the antiarrhythmic substances extracted from the cinchona plant, and by the 1920s, quinidine was used as an antiarrhythmic agent. However, in most patients with congestive heart failure, quinidine is well tolerated, perhaps because of its vasodilating actions. Quinidine prolongs refractoriness in most tissues, probably as a result of both prolongation of action potential duration and Na+ channel blockade. In intact animals and humans, quinidine also produces adrenergic receptor blockade and vagal inhibition. Thus, the intravenous use of quinidine is associated with marked hypotension and sinus tachycardia. Quinidine undergoes extensive hepatic oxidative metabolism, and approximately 20% is excreted unchanged by the kidneys. Concentrations of unbound 3-hydroxyquinidine equal to or exceeding those of quinidine are tolerated by some patients. Other metabolites are less potent than quinidine, and their plasma concentrations are lower; thus, they are unlikely to contribute significantly to the clinical effects of quinidine. Some of this variability may be assay dependent because not all assays exclude quinidine metabolites. In patients with advanced renal disease or congestive heart failure, quinidine clearance is decreased only modestly. Diarrhea usually occurs within the first several days of quinidine therapy but can occur later. Occasional cases occur at low dosages, often in patients with renal dysfunction, because sotalol is eliminated by renal excretion of unchanged drug. The other adverse effects of sotalol therapy are those associated with adrenergic receptor blockade (see previous discussion and Chapter 12).