General Information about Omnicef
Omnicef, additionally known by its generic name cefdinir, is a powerful antibiotic that's commonly used to deal with a broad range of bacterial infections. It belongs to a category of drugs known as cephalosporins, which work by interfering with the expansion and copy of micro organism. Omnicef is on the market in both oral suspension and capsule form, making it a flexible and convenient possibility for sufferers.
In conclusion, Omnicef is a flexible and potent antibiotic that's used to treat a variety of bacterial infections. It is particularly effective in treating situations similar to bronchitis, ear infections, throat and tonsil infections, pneumonia, sinus infections, and skin infections. While it could have some unwanted aspect effects, Omnicef is a priceless device in the struggle in opposition to bacterial infections and has helped numerous sufferers recover from these sicknesses.
Throat and tonsil infections, corresponding to strep throat, are also generally handled with Omnicef. These types of infections are brought on by streptococcus micro organism and may lead to a sore throat, problem swallowing, and fever. Omnicef works by attacking and killing the micro organism, relieving signs and serving to the patient get well.
While Omnicef is generally properly tolerated, like all medicine, it does have potential side effects. Common unwanted facet effects embody nausea, diarrhea, and headaches. These side effects are usually mild and can be managed by taking Omnicef with meals or adjusting the dosage. In rare instances, more serious unwanted effects similar to allergic reactions or extreme diarrhea might happen, and sufferers ought to seek medical attention if these happen.
Sinus infections, also referred to as sinusitis, are one other frequent reason for an Omnicef prescription. These infections occur when the sinuses, the air-filled cavities behind the nostril and cheeks, become inflamed and contaminated. Omnicef is in a position to successfully treat sinusitis by focusing on the micro organism liable for the infection and restoring health to the sinuses.
One of the most typical makes use of of Omnicef is for the therapy of acute bacterial flare-ups of chronic bronchitis. This situation occurs when the bronchial tubes, which carry air to and from the lungs, turn out to be infected and contaminated. Omnicef is particularly effective in treating this type of infection due to its capacity to target and get rid of the micro organism liable for the flare-up. Patients sometimes see an enchancment in their symptoms within a few days of starting the treatment.
In addition to bronchitis, Omnicef can additionally be generally prescribed for center ear infections, also recognized as otitis media. This kind of infection happens when the middle ear turns into infected and fills with fluid, causing ache and discomfort. Omnicef is efficient in treating most of these infections as a end result of it could penetrate the thick mucus current within the center ear and attain the positioning of an infection.
It is essential to notice that Omnicef is simply efficient against bacterial infections and will not be efficient in opposition to viral infections just like the widespread chilly or flu. Using Omnicef unnecessarily or not finishing the complete course of therapy can lead to antibiotic resistance, making it harder to treat future infections.
For patients with pneumonia, Omnicef is often prescribed as a first-line therapy. Pneumonia is a lung infection that may be brought on by numerous micro organism. Omnicef is effective against lots of the bacteria that generally trigger pneumonia, making it a useful tool in preventing this probably serious an infection.
Omnicef can be helpful in treating skin infections. This consists of bacterial infections such as impetigo, folliculitis, and cellulitis, among others. Omnicef is ready to penetrate the layers of skin to reach the site of infection and eliminate the bacteria inflicting the situation. This results in sooner healing and a reduction in symptoms corresponding to redness, swelling, and pain.
It is most common following gynaecological surgery but is also seen in patients with gynaecological malignancy or post radiotherapy bacteria normally carried by about a third of the population order omnicef 300 mg on line. In parts of the world where obstetric services are scarce, prolonged obstructed labour can be a common cause of vesicovaginal fistulae. Continual incontinence may also be seen in infants with congenital ectopic ureters. Occasionally, stress incontinence is so severe that the patient leaks continuously. The mainstay of treatment for urge incontinence is bladder retraining, which involves teaching patients to hold more urine voluntarily in their bladder, assisted by anticholinergic medication. Surgery may be required in patients who have severe daytime incontinence despite conservative treatment. Patients with overflow incontinence due to bladder obstruction should be treated surgically or with long-term catheterisation (intermittent or continuous). Incontinence secondary to neurological diseases can be managed by intermittent self-catheterisation. The incidence of urge incontinence increases with age, occurring in 1015% of the population aged over 65 years and in approximately 50% of patients requiring nursing home care. It is also seen in men with lower urinary tract obstruction and most often remits after the obstruction is relieved. Urine flow rates and full urodynamic assessment by cystometrography may be required to diagnose the type of incontinence and are indicated in selected cases when the diagnosis is unclear on clinical grounds. Some patients present suddenly with acute urinary retention, when they are unable to micturate and develop a painful, distended bladder. This is often precipitated by excessive alcohol intake, constipation or prostatic infection. Once a baseline value is established, any improvement or deterioration may be monitored on subsequent visits. Here, the bladder slowly distends due to inadequate emptying over a long period of time. Patients with chronic retention can also develop acute retention: so-called acute-on-chronic retention. This condition is characterised by pain-free bladder distension, which may result in hydroureter, hydronephrosis and renal failure (high-pressure chronic retention, of which nocturnal incontinence is a pathognomonic symptom). Abdominal examination may also reveal evidence of bladder enlargement in patients with urinary retention. A score of 07 indicates mild symptoms, 819 moderate symptoms and 2035 severe symptoms. Prostate cancer rarely occurs before the age of 50 and has a mean age at presentation of 70 years. Patients who present with acute retention require urgent treatment and should undergo immediate catheterisation to relieve the obstruction. The first-line treatments are 1A-adrenoceptor blockers such as tamsulosin, which reduce the tone of smooth muscle cells in the prostate and bladder neck, thereby reducing the obstruction. The 5-reductase inhibitors finasteride and dutasteride inhibit conversion of testosterone to the nine times more potent dihydrotestosterone in the prostate and so cause the prostate to reduce in size. Patients who fail to respond to a single drug may be treated with a combination of -blockers and 5-reductase inhibitors, since this is more efficacious than either agent alone. Symptoms that are resistant to medical therapy require surgical treatment to remove some of the prostate tissue that is causing urethral obstruction. Metastatic spread to pelvic lymph nodes occurs early and metastases to bone, mainly the lumbar spine and pelvis, are common. Genetic factors are known to play an important role in pathogenesis, m ok s ok ok ok ks ks oo Nocturia How many times did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning Frequency fre How often have you had to urinate again less than 2 hours after you finished urinating Objective assessment of obstruction is possible by urodynamics but this is seldom required. Seminomas arise from seminiferous tubules and represent a relatively low-grade malignancy. Metastases can occur through lymphatic spread, however, and typically involve the lungs. Teratomas arise from primitive germinal cells and tend to occur at a younger age than seminomas. Welldifferentiated tumours are the least aggressive; at the other extreme, trophoblastic teratoma is highly malignant. Leydig cell tumours are usually small and benign but secrete oestrogens, leading to presentation with gynaecomastia (p. The need for radical treatment of localised prostate cancer is still not established; radical treatments have significant potential morbidity and mortality, yet early identification and treatment of prostate cancer may save lives. Symptoms and signs due to metastases are much less common at the initial presentation but may include back pain, weight loss, anaemia and obstruction of the ureters. Prostatic cancer, like breast cancer, is sensitive to steroid hormones; metastatic prostate cancer is treated by androgen depletion, involving either surgery (orchidectomy) or, more commonly, androgen-suppressing drugs. Androgen receptor blockers, such as bicalutamide or cyproterone acetate, may also prevent tumour cell growth. This initially causes an increase in testosterone before producing a prolonged reduction, and for this reason the initial dose must be covered with an androgen receptor blocker to prevent a tumour flare. Chemotherapy with docetaxel can then be effective and provide a modest (around 3 months) survival advantage. Radiotherapy is useful for localised bone pain but the basis of treatment remains pain control by analgesia (p. Provided that patients do not die of another cause, the 10-year survival rate of patients with tumours localised to the prostate is 95%, but if metastases are present, this falls to 10%.
Pregnant women should avoid contact with cases of parvovirus B19 infection; if they are exposed antibiotics with alcohol buy cheap omnicef 300 mg online, serology should be performed to establish whether they are non-immune. Passive prophylaxis with normal immunoglobulin has been suggested for non-immune pregnant women exposed to infection but there are limited data to support this recommendation. The pregnancy should be closely monitored by ultrasound scanning, so that hydrops fetalis can be treated by fetal transfusion. The classic exanthem (erythema infectiosum) is preceded by a prodromal fever and coryzal symptoms. Infected individuals have a transient block in erythropoiesis for a few days, which is of no clinical consequence, except in individuals with increased red cell turnover due to haemoglobinopathy or haemolytic anaemia. These individuals develop an acute anaemia that may be severe (transient aplastic crisis; p. Infection during the first two trimesters of pregnancy can result in intrauterine infection and impact on fetal bone marrow; it causes 1015% of non-immune (non-Rhesus-related) hydrops fetalis, a rare complication of pregnancy. Most infections are spread by the respiratory route, although spread via contaminated blood is also possible. Arthropathies Adults and occasionally children fre Symmetrical small-joint polyarthropathy. In children it tends to involve the larger joints in an asymmetrical distribution co m 10% risk of congenital defects, most commonly deafness Gloves and socks syndrome Young adults Fever and an acral purpuric eruption with a clear margin at the wrists and ankles. The rash progresses from small pink macules to vesicles and pustules within 24 hours. Infectivity lasts from up to 4 days (but usually 48 hours) before the lesions appear until the last vesicles crust over. Due to intense itching, secondary bacterial infection from scratching is the most common complication of primary chickenpox. Adults, pregnant women and the immunocompromised are at increased risk of visceral involvement, which presents as pneumonitis, hepatitis or encephalitis. Manifestations are more severe in adults, pregnant women and the immunocompromised. Infection is almost universal, with approximately 95% of children acquiring this virus by 2 years of age. Rarely, older children or adults may develop an infectious mononucleosis-like illness, hepatitis or rash. In the immunocompromised, infection is rare but can cause fever, rash, hepatitis, pneumonitis, cytopenia or encephalitis. Antivirals are, however, used for uncomplicated chickenpox in adults when the patient presents within 2448 hours of onset of vesicles, in all patients with complications, and in those who are immunocompromised, including pregnant women, regardless of duration of vesicles (Box 11. More severe disease, particularly in immunocompromised hosts, requires initial parenteral therapy. Immunocompromised patients may have prolonged viral shedding and may require prolonged treatment until all lesions crust over. Children receive one dose after 1 year of age and a second dose at 46 years of age; seronegative adults receive two doses at least 1 month apart. Geniculate ganglion involvement causes the Ramsay Hunt syndrome of facial palsy, ok s oo oo ipsilateral loss of taste and buccal ulceration, plus a rash in the external auditory canal. Granulomatous cerebral angiitis is a cerebrovascular complication that leads to a stroke-like syndrome in association with shingles, especially in an ophthalmic distribution. Post-herpetic neuralgia causes troublesome persistence of pain for 16 months or longer, following healing of the rash. Oral aciclovir 200 mg 5 times daily or 400 mg 3 times daily for 5 days Famciclovir 125 mg twice daily for 5 days Valaciclovir 500 mg twice daily for 35 days or 2 g twice daily for 1 day. Chickenpox within 5 days of delivery leads to severe neonatal varicella with visceral involvement and haemorrhage. Post-herpetic neuralgia requires aggressive analgesia, along with agents such as amitriptyline 25100 mg daily, gabapentin (commencing at 300 mg daily and building slowly to 300 mg twice daily or more) or pregabalin (commencing at 75 mg twice daily and building up to 100 mg or 200 mg 3 times daily if tolerated). Although controversial, glucocorticoids have not been demonstrated to reduce post-herpetic neuralgia to date. Enteroviral infections are discussed further under viral infections of the skin (see below). Rashes may occur in these conditions but differ from those seen in exanthems or are not the primary presenting feature. Vaccination has reduced the incidence in children but incomplete coverage and waning immunity with co. Infection is seasonal, and variation in the haemagglutinin (H) and neuraminidase (N) glycoproteins on the surface of the virus leads to disease of variable intensity each year. Management and prevention co Enteroviral exanthems the diagnosis is usually clinical. In atypical presentations without parotitis, serology for mumps-specific IgM or IgG seroconversion (fourfold rise in IgG convalescent titre) confirms the diagnosis. Classical tender parotid enlargement, which is bilateral in 75%, follows a prodrome of pyrexia and headache. Rare complications include encephalitis, transient hearing loss, labyrinthitis, electrocardiographic abnormalities, pancreatitis and arthritis. Approximately 25% of post-pubertal males with mumps develop epididymo-orchitis but, although testicular atrophy occurs, sterility is unlikely. Administration of neuraminidase inhibitor, oral oseltamivir (75 mg twice daily) or inhaled zanamivir (10 mg twice daily) for 5 days, can reduce the severity of symptoms if started within 48 hours of symptom onset (or possibly later in immunocompromised individuals). Resistance can emerge to all of these agents and so updated local advice should be followed with regard to the sensitivity to antivirals of the circulating strain. Prevention relies on seasonal vaccination of the elderly, children 27 years of age and individuals with chronic medical illnesses that place them at increased risk of the complications of influenza, such as chronic cardiopulmonary diseases or immune compromise, as well as their health-care workers. Avian viruses, such as H5N1, possess alternative haemagglutinin antigens to seasonal influenza strains.
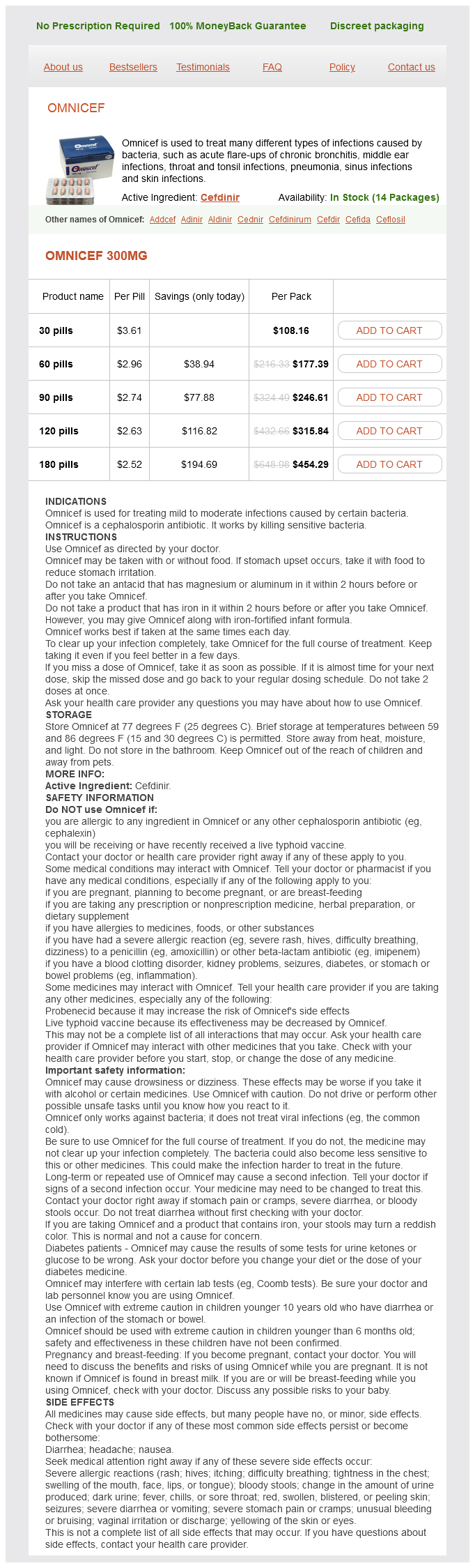
Omnicef Dosage and Price
Omnicef 300mg
- 30 pills - $108.16
- 60 pills - $177.39
- 90 pills - $246.61
- 120 pills - $315.84
- 180 pills - $454.29
Following the identification of hyperglycaemia and subsequent diagnosis of diabetes antibiotics for uti while trying to conceive omnicef 300 mg buy mastercard, the initial management involves a careful clinical assessment of the patient to decide whether immediate treatment is required and, with appropriate investigation, to establish the aetiology of the diabetes, as this will determine subsequent diabetes treatment. If the aetiological diagnosis is in doubt, it is important not to delay insulin treatment, which can be withdrawn subsequently if necessary. The classical clinical features of type 1 and type 2 diabetes are compared in Box 20. Symptoms of polydipsia, polyuria, nocturia and rapid weight loss are prominent in type 1 diabetes but are often absent in patients with type 2 diabetes, many of whom are asymptomatic or have nonspecific complaints such as chronic fatigue and malaise. Uncontrolled diabetes is associated with an increased susceptibility to infection and patients may present with skin sepsis (boils) or genital candidiasis, and complain of pruritus vulvae or balanitis. While the distinction between type 1 and type 2 diabetes is usually obvious, overlap occurs, particularly in age at onset, duration of symptoms and family history. Islet autoantibodies are detectable at high titre in many patients with type 1 diabetes, so a negative result should prompt consideration of other aetiologies. A history of pancreatic disease, particularly in patients with a history of alcohol excess, makes insulin deficiency more likely. Thus, diabetes may be first suspected when a patient visits an optometrist or podiatrist, or presents with hypertension or a vascular event such as an acute myocardial infarction or stroke. Blood glucose should therefore be checked in all patients presenting with such pathology. The detailed investigation and management of diabetic complications are described on page 755. Physical signs in patients with type 2 diabetes at diagnosis depend on the mode of presentation. In Western populations, more than 80% are overweight and the obesity is often central (truncal or abdominal). Although dyslipidaemia is also common, skin lesions such as xanthelasma and eruptive xanthomas are rare. Regular clinical and biochemical review is essential, particularly during the first 24 hours of treatment. Early specialist involvement is recommended for highrisk groups such as older people, young adults (1825 years), pregnant women, and those with heart or kidney failure or other serious comorbidities. In the fulminating case, the striking features are those of salt and Management oo Clinical assessment oo k the presence of one or more of the features listed in Box 20. Potassium loss is exacerbated by secondary hyperaldosteronism as a result of reduced renal perfusion. When this exceeds the capacity to metabolise acidic ketones, these accumulate in blood. The resulting metabolic acidosis forces hydrogen ions into cells, displacing potassium ions. About half the deficit of total body water is derived from the intracellular compartment and occurs comparatively early in the development of acidosis with relatively few clinical features; the remainder represents loss of extracellular fluid sustained largely in the later stages, when marked contraction of extracellular fluid volume occurs, with haemoconcentration, a decreased blood volume, and finally a fall in blood pressure with associated renal ischaemia and oliguria. Plasma potassium may even be raised initially due to disproportionate loss of water, catabolism of protein and glycogen, and displacement of potassium from the intracellular compartment by H+ ions. However, soon after treatment is started, there is likely to be a precipitous fall in the plasma potassium due to dilution of extracellular potassium by administration of intravenous fluids, the movement of potassium into cells induced by insulin, and the continuing renal loss of potassium. The magnitude of the hyperglycaemia does not correlate with the severity of the metabolic acidosis; moderate elevation of blood glucose may be associated with lifethreatening ketoacidosis. Conversely, in other situations, hyperglycaemia predominates and acidosis is minimal, with patients presenting in a hyperosmolar state (p. Mental apathy, delirium or a reduced conscious level may be present, although coma is uncommon. Indeed, a patient with dangerous ketoacidosis requiring urgent treatment may walk into the consulting room. In fact, it is imperative that energetic treatment is started at the earliest possible stage. In infected patients, pyrexia may not be present initially because of vasodilatation secondary to acidosis. Exceptionally, if intravenous administration is not feasible, soluble insulin can be given by intramuscular injection (loading dose of 1020 U, followed by 5 U hourly), or a fastacting insulin analogue can be given hourly by subcutaneous injection (initially 0. The blood glucose concentration should fall by 36 mmol/L (approximately 55110 mg/dL) per hour, or blood ketone concentrations fall by at least 0. A more rapid decrease in blood glucose should be avoided, as this might precipitate hypoglycaemia and the serious complication of cerebral oedema, particularly in children. Failure of blood glucose to fall within 1 hour of commencing insulin infusion should lead to a reassessment of insulin dose. Ketosis, dehydration, acidaemia, infection and stress combine to produce severe insulin resistance in some cases, but most will respond to a lowdose insulin regimen. When the blood glucose has fallen, 10% dextrose infusion is introduced and insulin infusion continued to encourage glucose uptake into cells and restoration of normal ok s oo oo eb o eb eb In adults, rapid fluid replacement in the first few hours is usually recommended (Box 20. Caution is advised in children and young adults because of the risk of cerebral oedema. Most guidelines favour correction of the extracellular fluid deficit with isotonic saline (0. Introduction of 10% glucose is recommended when the blood glucose falls below 14 mmol/L (252 mg/dL). Restoration of the usual insulin regimen, by subcutaneous injection, should not be instituted until the patient is both biochemically stable and able to eat and drink normally.