General Information about Omeprazole
One of the main benefits of Prilosec is its ability to provide aid from the uncomfortable signs of GERD. By decreasing the quantity of acid in the abdomen, this medicine can help alleviate heartburn and other symptoms associated with the situation. It works by blocking the proton pump, which is answerable for producing acid in the abdomen.
Prilosec is primarily used to treat gastroesophageal reflux disease (GERD), a situation by which stomach acid flows back into the esophagus, inflicting signs corresponding to heartburn, chest pain, and issue swallowing. It can be used to treat different situations corresponding to ulcers, Zollinger-Ellison syndrome, and Helicobacter pylori (H. pylori) infection.
The prescription model of Prilosec is out there in numerous strengths and forms, together with capsules and powder type for oral suspension. The dosage and duration of therapy will rely upon the situation being treated and the individual's response to the medication.
Omeprazole, generally bought under the model name Prilosec, is a medication used to treat varied situations associated to the stomach and esophagus. It belongs to a category of medicine generally identified as proton pump inhibitors (PPIs), which work by reducing the quantity of acid produced within the stomach.
The over-the-counter Prilosec comes within the type of delayed-release tablets and is typically taken once a day for 14 days. It is essential to observe the recommended dosage and length of therapy, as extended use can result in serious unwanted side effects.
While Prilosec is generally thought of protected and effective, it is essential to seek the advice of a well being care provider before utilizing it. Certain medical circumstances and drugs might work together with Prilosec, and it's important to discuss potential risks and advantages with a healthcare skilled.
In conclusion, Prilosec, also called omeprazole, is a widely used medicine for treating various circumstances related to the abdomen and esophagus. Its capability to reduce stomach acid makes it an efficient remedy for GERD and other related circumstances. However, as with all medicine, it's important to make use of Prilosec as directed and to consult a physician before utilizing it. Long-term use might result in critical side effects, so you will need to use Prilosec under medical supervision.
Additionally, Prilosec isn't beneficial for long-term use with out medical supervision. Prolonged use could result in an elevated risk of sure health issues, corresponding to osteoporosis and infections.
Like any medicine, Prilosec could cause unwanted effects in some people. Common side effects embrace headache, stomach pain, nausea, and diarrhea. In uncommon cases, more severe side effects, similar to allergic reactions, liver damage, and vitamin B12 deficiency, could happen. It is crucial to hunt medical consideration if any extreme or persistent side effects are skilled while taking Prilosec.
Prilosec is out there in both over-the-counter and prescription types. The over-the-counter model is used to treat frequent heartburn (occurring two or more days a week), while the prescription model is used for extra serious circumstances similar to GERD.
Both the gums and mucous membranes are observed for bleeding gastritis or ibs buy cheap omeprazole 10 mg on-line, sores, and hydration status. If teeth are present, they should be observed for number, caries, grinding, and occlusion. The bite reflex is demonstrated during infancy by an up-anddown movement of the jaw. It is elicited by placing a tongue blade on the anterior one third of the tongue and gently "walking back" until the tongue "humps" or elevates. This is one of the signs indicating the child can protect the airway during swallowing. At this point, it is usually necessary to soothe and quiet the infant before proceeding. This immature tongue movement pushes solid food out of the mouth when it is placed on the anterior part of the tongue. It can be assessed by placing a small quantity of food on the tongue and observing the tongue movement. The tongue protrusion reflex is one of the reasons why infants should not be fed solid foods for the first 4 to 6 months of life. First assess the mouth and oral cavity, including both structure and function, as mentioned previously. Feeding skills assessment After a general oral sensorimotor examination, a meal observation is required. It is important to replicate normal routines wherever possible to ensure that the observation reflects a normal meal. Modifications in feeding/eating may be trialed-for example, positioning, pacing, a different teat/ utensil or a different texture/viscosity. Again, assess the structure and movement of the mouth and oral cavity, including: n Rooting reflex (disappearing at Birth to 5 Months A meal observation in a young infant should consider suck/swallow/breathe competency, maintenance of physiologic stability, as well as any signs of anatomical or physiological deficits (Thoyre et al. Can the infant 35 months) 292 Dysphagia assessment anD treatment planning: a team approach coordinate swallowing with breathing efficiently throughout a feed Can the infant maintain healthy oxygen saturation and heart rate throughout a meal Inadequate lip or jaw closure makes eating and swallowing difficult because of an inability to create an adequate seal around the bottle/ nipple, resulting in insufficient negative intraoral pressures. Impaired tongue mobility affects both intraoral pressure and oral transfer of a food bolus before swallow. The swallow reflex can be observed or felt by the upward and forward movement of the cricoid cartilage during the introduction of liquids listening for any signs of aspiration (see Aspiration section later in chapter). If an incompetent pharyngeal swallow or respiratory changes are suspected, or the child is at risk for pulmonary compromise, pharyngeal imaging may need to be considered (see criteria for dynamic swallow study [Chapters 68]). An inefficient feed, where the infant continues to feed but the volume per minute is low, may suggest oromotor impairment. The clinician must look out for short or prolonged feeds as well as fatigue effects. Once fluid/food is introduced, the clinician must look for signs of diminished responses, hyperactive responses, and oral sensory defensiveness (Arvedson & Brodsky, 2002). Chil- dren at this development stage begin gaining voluntary oral control by alerting with mouth opening at the sight of food, elevating the tongue, and beginning to manipulate food orally and starting to initiate self-feeding behaviors. To assess voluntary oral control, it will be necessary to offer solid pureed food. When the food is first offered, voluntary alerting and mouth opening to accept food are seen in an infant at this stage. Tongue elevation (tongue pushes back and touches palate) and lateral (side to side) movements should be observed. If tongue elevation is not noted during the oral assessment, it can be assessed by offering food with a spoon. Tongue elevation clears food from the roof of the mouth and is necessary for the infant to eat and swallow pureed foods. Tongue elevation will be seen when the infant loses the protrusion reflex and gains the ability to manipulate and swallow pureed foods given by spoon. Food manipulation or munching involves jaw movements and tongue lateralization (the ability of the tongue to move side to side). Tongue lateralization enables the food to be moved to and from the gums and teeth for swallowing. Many normally developing children will experiment with finger food and soft solids during this stage. The up-and-down jaw movements are followed by lateral jaw movements (and later by mature rotary movements: "rotary grind"). During this initial stage, up-and-down and lateral jaw movements, with tongue lateralization, are normal. Inadequate food manipulation or lack of tongue lateralization makes eating textured food difficult or impossible. Self-feeding at this stage is demonstrated by: n Increasing midline stability to sit food manipulation, chewing skills, and self-feeding skills. The up-and-down and lateral chewing now progresses to the beginning of a mature rotary-type movement. The pincer grasp allows the child to pick up food between his thumb and finger, enabling self-feeding with utensils and the ability to self-feed bite-size pieces of food. These are primarily chewing and further development of fine motor skills and control. In the older child, dentition plays a more important role in mealtime competency, and occlusion patterns and dental health need to be assessed.
Brain activation during oral exercises used for dysphagia rehabilitation in healthy human subjects: A functional magnetic resonance imaging study gastritis symptoms how long do they last purchase omeprazole 20 mg overnight delivery. Exercise using tongueholding swallow does not improve swallowing function in normal subjects. Manofluorographic and functional outcomes after endoscopic laser cricopharyngeal myotomy for cricopharyngeal bar. Effects of enhanced bolus flavors on oropharyngeal swallow in patients treated for head and neck cancer. Effect of citric acid and citric acid-sucrose mixtures on swallowing in neurogenic oropharyngeal dysphagia. Impact of expiratory muscle strength training on voluntary cough and swallow function in Parkinson disease. Changes in pharyngeal corticobulbar excitability and swallowing behavior after oral stimulation. American Journal of Physiology-Gastrointestinal and Liver Physiology, 286, G45G50. Dysphagia in the child with developmental disabilities: Medical, clinical and fam ily interventions. Effect of speech bulb reduction on movement of the posterior wall of the pharynx and posture of the tongue. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Role of pharyngeal propulsion as an indicator for upper esophageal sphincter myotomy. Swallowing disorders in muscular diseases: Functional assessment and indications of cricopharyngeal myotomy. History and principles of exercise-based therapy: How they inform our current treatment. Seminars in Speech and Language: New Frontiers in Dysphagia Rehabilitation, 27, 227235. Proof-of-principle pilot study of oropharyngeal air-pulse application in individuals with dysphagia after hemispheric stroke. Surface electromyographic activity of the submental muscles during swallowing and during expiratory pressure threshold training tasks. Maxillary reshaping prostheses: Effectiveness in improving speech and swallowing in post-surgical oral cancer patients. Cricopharyngeal myotomy normalizes the opening size of the upper esophageal sphincter in cricopharyngeal dysfunction. Sievers Early identification of patients with dysphagia is important to maintain nutritional requirements, to protect the airway during swallow and to prevent untoward complications. In a hospitalized patient, a nurse may be the first person to recognize the signs and symptoms of dysphagia. The nurse also plays a major role in implementing ongoing strategies for treatment, particularly as these relate to alternative feeding methods or monitoring of dietary recommendations and restrictions. It therefore is incumbent on the dysphagia team nurse and the staff nurse to be knowledgeable about the person with dysphagia, including symptoms, risk factors, complications, and overall plan of care. This article addresses, first, the role of the nurse in observing and evaluating patients with, or at risk for, dysphagia and, second, the role of the nurse in the ongoing care and monitoring of dysphagic patients, particularly as it relates to hospitalized patients. More difficult to identify are dysphagic patients with conditions that may not clearly signal dysphagia. Patients recovering from stroke, patients with dementia 221 222 Dysphagia assessment anD treatment planning: a team approach or other mental debilitation, elderly patients, and malnourished or deconditioned patients may fall into this category. All critically ill patients are at risk for dysphagia due to altered levels of consciousness and general deconditioning. This includes weakness of musculature involved in both bolus propulsion and preparation and airway protection during deglutition. Deconditioned patients lack breath support and have a poor cough in response to airway penetration by food or liquid, making them less able to respond effectively to even mild aspiration. Evidence of repeated fevers or pneumonia in a patient should also stimulate concern if there is a possibility that these symptoms could be related to aspiration. Patients with cardiopulmonary pathologies such as cardiomyopathies, pulmonary hypertension, and cardiovascular diseases are also at heightened risk for pulmonary complications from dysphagia (Table 111). Aspiration Pneumonia True aspiration pneumonia has a typical radiographic pattern. The pattern demonstrates infiltration or consolidation first in the right lower lobe, next table 111. Pulmonary Risk Factors Patients with pre-existing pulmonary disease who become dysphagic have a diminished ability to tolerate even mild aspiration. Aspiration insults are very poorly tolerated by an already compromised pulmonary system. Pulmonary diseases include all the smoking-related lung diseases - for example, emphy- · ajorabdominalandthoracic M trauma/surgery. This distribution is a consequence of the angle of the tracheobronchial takeoff into the parenchyma of the right lung. The right lower lobe represents a straight line of descent from the trachea and right main stem bronchus. In a patient who is supine, or lying on the right side, the right upper lobe takeoff from the right main stem bronchus represents a dependent position. These common sites of aspiration are influenced largely by gravity and human anatomy. The diagnosis of aspiration pneumonia in a patient relies on both clinical and radiographic signs. To ensure appropriate treatment, pneumonia related to dysphagia, or difficulty eating and drinking, must be differentiated from a pneumonia related to a single aspiration event or a community acquired pneumonia from other etiologies.
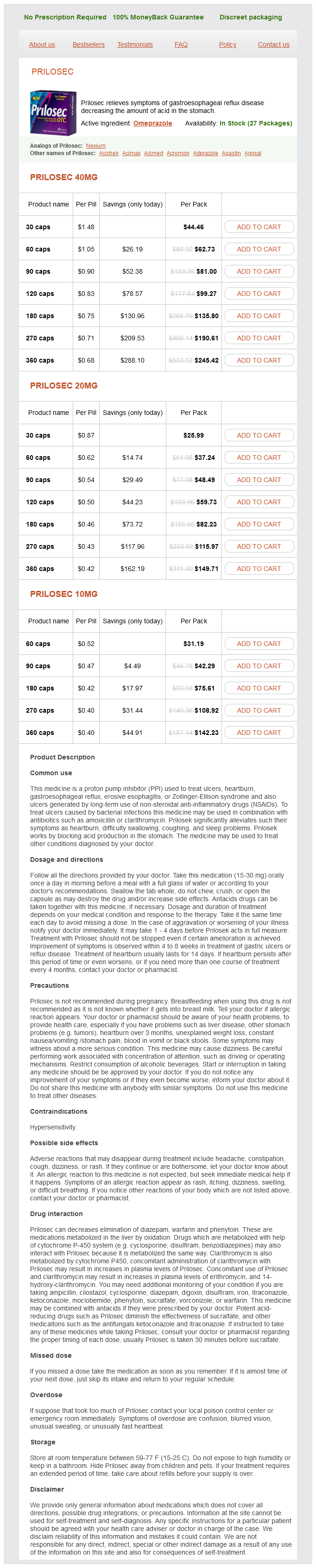
Omeprazole Dosage and Price
Prilosec 40mg
- 30 caps - $44.46
- 60 caps - $62.73
- 90 caps - $81.00
- 120 caps - $99.27
- 180 caps - $135.80
- 270 caps - $190.61
- 360 caps - $245.42
Prilosec 20mg
- 30 caps - $25.99
- 60 caps - $37.24
- 90 caps - $48.49
- 120 caps - $59.73
- 180 caps - $82.23
- 270 caps - $115.97
- 360 caps - $149.71
Prilosec 10mg
- 60 caps - $31.19
- 90 caps - $42.29
- 180 caps - $75.61
- 270 caps - $108.92
- 360 caps - $142.23
Pressure (P) and flow (Q) waveforms measured at any site in the vascular system can be considered as the summation of a forward gastritis diet mayo clinic 10 mg omeprazole order with mastercard, or antegrade, traveling wave and a reflected, or retrograde, traveling wave: P Pf Pr Q Qf Qr (4. With the characteristic impedance determined by a time domain method, forward and reflected waves can also be resolved in the time domain (Li, 1986). This approach is known as the time-domain wave separation method, which has been widely used. Similarly, resolution of flow into its forward and reflected components can be obtained from a set of two equations: Q f (Q P / Zo) / 2 (4. An increase in wave reflection increases the pressure amplitude, but decreases the flow amplitude. This is particularly evident during different spontaneous or induced vasoactive states. Its primary effect is in increasing peripheral vascular resistance and has little cardiac effect. This is a common vasodilator that can profoundly decrease peripheral vascular resistance and increase arterial compliance. It can be seen that the pressure waveform during strong vasodilation more closely resembles that of the flow waveform. Other popularly used vasoactive drugs are phenylephrine and nitroglycerine for inducing vasoconstriction and vasodilation, respectively. It is clear that wave reflection exerts opposite effects on pressure and flow waveforms. The increased reflected pressure component adds to the forward wave to result in the measured pressure waveform. Reflected wave has a more significant Hemodynamics of Arteries 105 effect in mid- to late systole to impede ventricular ejection. Wave reflection decreases the flow, as the reflected component of flow is mostly negative. Notice that wave reflection exerts opposite effects on pressure and flow waveforms, as seen from Qr and Pr. As a consequence, the pulse pressure is significantly increased with a concurrent decrease in flow amplitude. The time that 106 Dynamics of the Vascular System (2nd Edition) takes for forward pressure to reach its peak is not too different from that of the reflected component. Notice the similarity between the pressure and flow waveforms and that the reflected components are small. Pulse pressure amplitude alone often does not indicate the underlying factors governing the morphology of blood pressure pulse waveforms, although its increase has been shown to correlate with an increase in vascular stiffness. Thus, the routine clinically used cuff method for measuring systolic and diastolic pressures cannot be used to infer contributing factors to vascular stiffness or arterial properties. A wave reflection-based distributed model (Zhang and Li, 2009) can be used to resolve the vasoactive from mechanical factors. For the fundamental harmonic, the mean value of the reflection coefficient at control is about 0. The reflection coefficient remains low for higher frequencies during vasodilation. For a vessel with characteristic impedance Zo and terminated with vascular load impedance Z, the reflection coefficient is given by: Z Zo Z Zo (4. Thus, the magnitude and timing of arrival of reflected waves are both important in modifying the propagating pulse. Comparison of time and frequency domain descriptions of the reflection coefficients have been provided by Lei et al. Additionally, the global reflection coefficient presented here is in general, masked by the repeated reflections (Berger et al. Notice the diastolic wave is significantly augmented in vasoconstriction and abolished in vasodilation. Notice Hemodynamics of Arteries 111 that the diastolic pressure wave is abolished during acetylcholineinduced vasodilation and accentuated during norepinephrine-induced vasoconstriction. For the control data (circle), the magnitude of the reflection coefficient ranged from 0. Vasodilation (triangles) decreased the reflection coefficient to a value less than 0. Since frequency domain interpretation of wave reflections is complex and cumbersome to obtain, a simplified index to 112 Dynamics of the Vascular System (2nd Edition) interpret wave reflection in the aorta, in the time domain, was introduced by Murgo et al. Ascending aortic pressure waveforms were defined in terms of their morphological differences and separated into different types. Augmentation index is merely a single number and cannot represent the frequency content of the reflected wave, its timing of arrival or temporal amplitude. In addition, the inflection pressure is often obtained at the early upstroke of the systolic aortic pressure when there are supposedly less reflected waves present. As we have seen earlier that significantly greater amount of reflected waves occurs in mid- to late systole. Some suggest that the major reflection site as seen from the proximal aorta, appears to be in the region of the pelvis or the aorto-iliac branching junction. Others, however, suggest that the first major potential reflecting site is at the aortic arch. Although there is no major agreement on the reflecting sites, the arterioles are recognized as being the principal sites for wave reflection, and the reflection coefficient as being high. There are multiple reflection sites and the effects of repeated reflections on pressure and flow waveforms have been investigated (Berger et al.