General Information about Nifedipine
In conclusion, nifedipine, also called Adalat, is a generally prescribed medication for hypertension and angina. It works by relaxing the blood vessels and growing blood flow, effectively lowering blood strain and relieving chest pain. It is essential to take nifedipine as prescribed and to pay attention to potential unwanted effects. With correct use, nifedipine can considerably improve the health and well-being of these residing with hypertension and angina.
Nifedipine is a highly efficient medication for treating hypertension and angina. Studies have shown that it could considerably lower blood stress and decrease the frequency and severity of angina attacks. It may also help prevent coronary heart attacks and strokes in people with hypertension.
Nifedipine works by blocking the motion of calcium into the muscle cells of the guts and blood vessels. This causes the blood vessels to loosen up and widen, decreasing the stress against the artery partitions. As a result, blood can move extra easily and efficiently via the physique, reducing blood pressure and relieving angina symptoms.
Nifedipine is on the market in two varieties, immediate-release and extended-release. The immediate-release form is taken 3 times a day, while the extended-release form is taken as soon as a day. It is essential to take nifedipine exactly as prescribed by a healthcare skilled, as it is a sensitive treatment and the dose have to be fastidiously monitored.
In addition to its primary uses, nifedipine has additionally been found to be helpful in treating other situations, such as Raynaud's phenomenon (a condition that causes numbness and pain within the fingers and toes) and excessive altitude pulmonary edema (fluid accumulation within the lungs caused by excessive altitudes).
Hypertension is a condition the place the drive of blood against the artery partitions is just too high and might lead to serious health issues, similar to coronary heart attack, stroke, or kidney illness. Angina is a type of chest pain that occurs when there's a lack of blood move to the guts, often caused by a blockage within the arteries.
Nifedipine, generally recognized by its brand name Adalat, is a medication used to deal with hypertension (high blood pressure) and angina (chest pain). It belongs to a class of medication known as calcium channel blockers, which work by enjoyable the blood vessels and increasing blood move.
The most common aspect impact of nifedipine is a headache, which may be relieved by taking a non-steroidal anti-inflammatory drug (NSAID) like ibuprofen. Other potential side effects embrace nausea, dizziness, and flushing of the face. In uncommon cases, nifedipine may cause extra critical unwanted aspect effects, similar to allergic reactions, irregular heartbeat, and swelling of the hands and toes. If any of those symptoms happen, you will want to seek medical consideration immediately.
It is important to notice that nifedipine shouldn't be taken by individuals who've a history of coronary heart failure, liver problems, or low blood pressure. It also can work together with sure medications, similar to beta blockers, anti-seizure medicine, and antibiotics, so it's essential to inform the doctor of some other medicines being taken.
An unusual finding was the report of hyperplasia of the juxtaglomerular apparatus in one infant arteria austin 20 mg nifedipine order free shipping. This appears to be unique: this finding has not been reported since and was absent from our series of kidney biopsies despite a careful search. The inference that this represents a secondary change is strengthened by the profound electrolytic disturbances in that patient, which, as the author discussed, may have induced a change in the juxtaglomerular apparatus. Although liver transplantation may correct the metabolic derangement in many patients, some biochemical anomalies of renal tubular function may persist [43]. In 9 of 24 patients with tyrosinemia where renal tissue was examined at the H𰩴al Sainte-Justine, there was a mild to moderate degree of glomerulosclerosis and interstitial fibrosis mild glomerulosclerosis being defined as the occurrence of sclerosis in at least 10% of glomeruli accompanied by interstitial changes [9]. Significant glomerular changes have been reported infrequently in hereditary tyrosinemia. In two patients, renal failure accompanied the glomerular changes, the latter attributed to the metabolic disease rather than a consequence of pyelonephritis or an unrelated glomerulopathy [44]. Eight of the nine patients in our series were older than 2 years, and in four the findings were noted in renal biopsies obtained either shortly before or at the time of liver transplantation. Immunofluorescence studies usually did not reveal any significant immune deposits in the glomeruli, although the occasional presence of immunoglobulin A, a non-specific Heart Myocardial hypertrophy has been associated with ultrastructural changes characterized principally by increased numbers of mitochondria in the myocytes [36]; these patients had a significant incidence of cardiomyopathy as detected by echocardiography but a low incidence of clinical heart disease. By comparison, an obstructive cardiomyopathy has been described in two symptomatic patients [36]. Peripheral nerves Three peripheral nerve specimens have been analyzed during the period of recuperation, 2Ͷ weeks following paralytic crises [15]. All three samples revealed axonal degeneration and secondary demyelination, similar to the changes seen in acute intermittent porphyria. Management Nitisinone treatment for tyrosinemia Treatment protocols Nitisinone is started at a daily dosage of 1Ͳ mg/kg. Nitisinone has a long half-life (>50 hours) and is provided in one or two daily doses. The prescription is adjusted to maintain (1) an absence of detectable urinary and blood succinylacetone and (2) plasma nitisinone at >50 mol/L. In non-screened patients who present acutely with symptoms suggestive of tyrosinemia, an initial dose of 2 mg/kg daily is prescribed after adequate diagnostic samples have been obtained (the administration of nitisinone rapidly reduces the levels of succinylacetone in urine and blood, and pretreatment samples are critical for precise diagnosis). Plasma tyrosine is used to adjust dietary prescriptions in nitisinone-treated patients. A tandem mass spectrometrybased assay for simultaneous determination of nitisinone, succinylacetone, tyrosine, phenylalanine, and methionine levels on a dried blood spot has been reported [46]. The above recommendations for nitisinone, succinylacetone, and tyrosine levels are reasonable based upon current knowledge but have not been formally shown to be optimal. The monitoring protocol during nitisinone treatment involves the collection of pretreatment baseline specimens of blood and urine, close observation for immediate adverse effects after initiating nitisinone administration (none has been detected to date), and metabolic monitoring for 1 week in hospital and with decreasing frequency until 6 months, at which time metabolic testing is performed at 3-month intervals (with closer surveillance if clinically indicated). Dietary records for 72 hours are used to calculate phenylalanine plus tyrosine intake every 3 months. Baseline ophthalmologic assessment (see Complications) is done before or soon after beginning treatment and slit lamp assessments are repeated if ocular symptoms develop. Results the results of the first 15 years of the Quebec protocol have recently been analyzed [47]. Patients were divided into those that received nitisinone before 1 month of age ("early" treatment group, 24 patients) and those who received their first dose after 1 month ("late" group, 26 patients) and a historical control group born in the previous decade who never received nitisinone before receiving a transplant or death (28 patients). There were striking differences among these three groups with respect both to acute complications (hospitalizations for tyrosinemia-related reasons and neurologic crises) and to chronic outcomes (transplantation, death). For example, no hospitalizations for acute complications were observed in over 5700 patient-months of nitisinone treatment, compared with 184 hospitalizations in 1312 patient-months without nitisinone treatment (p < 0. Liver transplantation was performed in 20 of the nontreated patients (71%) at a median age of 26 months, versus seven late-treated patients (26%; p < 0. Ten deaths occurred in non-nitisinone-treated patients versus two in treated patients (p < 0. The two deaths in treated patients were caused by complications related to liver transplantation not to tyrosinemia-related complications. It is impossible to conclude whether the development of nodules in late-treated patients represents only the expected repair and regeneration in response to severe pretreatment liver damage or whether there was also a component of true progression of the disease during nitisinone treatment. However, data from the early-treated patients hint at a near-complete suppression of hepatic disease in compliant patients who receive nitisinone. Inclusion of patients for analysis in the early treatment group was restricted to patients with over 5 years of follow-up, in order to assure a follow-up time over twice the median age for liver transplantation of untreated patients. Patients who began nitisinone treatment more recently than that have similar results but were not analyzed because of their shorter follow-up time. Vigilance, meticulous follow-up of individual patients, and ongoing compilation of the world experience with nitisinone treatment will be required to obtain adequate data collection. Should regions other than those at high risk perform neonatal screening for tyrosinemia? The technical obstacles to incorporating succinylacetone determination into expanded neonatal screening are being overcome [48]. Efficient neonatal screening combined with early nitisinone treatment, often makes the difference between presymptomatic initiation of an effective and possibly curative medical treatment and the situation with late detection, often when liver failure or irreversible liver damage has occurred. Complications To date, in our series, the only complication attributable to nitisinone has been ocular. The question mark reflects the unknown course of tyrosinemia with long-term nitisinone treatment. Similar lesions have occurred in other nitisinone-treated patients and occur in rats following tyrosine loading or nitisinone treatment [13,49,50]. Photophobia and ocular inflammation in a nitisinone-treated patient are considered to be indications for emergency ophthalmologic examination to eliminate the presence of corneal crystals.
The febrile response may represent an uncoupling of oxidative phosphorylation secondary to lack of Pi blood pressure chart high diastolic generic 20 mg nifedipine otc. The glucagon results in the excessive formation of glucose 6-phosphate from glycogen. Because of the G6Pase deficiency, a burst of glycolysis results in excess production of reduced cofactors, which normally produce high-energy phosphates. Corby and coworkers examined platelet function in 13 patients, each with deficient hepatic activity of one of the following enzymes: G6Pase, debrancher enzyme, phosphorylase, or phosphorylase kinase [140]. Only the seven patients with G6Pase deficiencies had abnormal platelet aggregation, and four of these also had abnormal platelet adhesiveness. This is at variance with the previously held view that they occur only infrequently. Adenomas develop in most patients during the second decade of life, but they may be found in 3-year-old children. The nodules, which are best demonstrated by ultrasonography and radioisotopic scanning, show increased echodensity and decreased isotope uptake. At laparotomy, they appear as discrete, pale nodules that range in number from one to many and in size from 1 to 5 cm. A number of patients have been found to have solitary hepatocellular adenocarcinomas in individual nodules [142]. The mechanism causing the adenomas or their malignant degeneration is not known, but treatment with portacaval shunting does not prevent their development. The pathogenesis of hepatic adenomas is not known but they are believed to be secondary to chronic stimulation of the liver by hepatotrophic agents such as glucagon. Our own experience with two patients who had adenomas prior to nocturnal feeding showed resolution of these adenomas after 3 years of treatment [143]. A significant difference in progression to hepatocellular adenoma has been shown between two groups based on 5-year mean serum triglyceride concentrations: those with 500 mg/dL having slower progression than those with >500 mg/dL [144]. A similar progression has been observed in experimental hepatocarcinogenesis from exposure to N-nitrosomorpholine. Second, the focal cluster of cells develops a gradual reduction in glycogen content and a concomitant increase in ribosomes, reflected as basophilia by hematoxylin and eosin (H&E) staining. Finally, the foci enlarge and acquire the phenotypic markers of hepatocellular carcinoma. By preventing the decrease in blood glucose with an exogenous supply of glucose, excessive glycolysis and gluconeogenesis are prevented. This results in a net decrease in production of circulating triglyceride, cholesterol, lactate, and uric acid. Therefore, a quantitative determination is necessary to make a diagnosis of excessive glycogen content. Direct assay of hepatic enzyme activity (hydrolysis by G6Pase) in a fresh liver biopsy specimen is advocated. In order to provide some selectivity in the application of this procedure, determination of serial blood glucose and lactate levels during a 4- to 6-hour fast as well as maximum blood glucose response to glucagon is recommended. A deficiency of phosphorylase kinase, which is not routinely measured in liver tissue samples, should be suspected if blood glucose rises more than 30 mg/dL [123]. Glucagon administration typically fails to produce an increase in blood glucose in these patients. Within 20 minutes after administration, however, patients may experience a substantial decrease in blood glucose, followed by development of severe metabolic acidosis. The use of these tests has the advantage of avoiding risks associated with more invasive diagnostic techniques; however, a substantial blood volume is required for completion, and results frequently fail to yield a definitive diagnosis. The lipid content in the liver of an untreated patient is substantially greater than that in the liver of a patient who has been treated, but in either instance, hepatic steatosis is a prominent morphologic feature. This suggested that bypassing the liver with nutrients was not the most important factor in reversing the abnormalities. The hypothesis states that, as blood glucose falls below a critical level, compensatory mechanisms cause glycogen degradation to glucose 6-phosphate. In the absence of G6Pase, glucose 6-phosphate is not hydrolyzed to release free glucose, and the hepatic stimulus for glycogenolysis results in formation of other intermediates such as lactate, triglycerides, and cholesterol. To interrupt the stimulus, treatment with an exogenous source of glucose inhibits the release of hepatotropic stimuli and thus the excess glycogenolysis. In addition, the hypothesis suggests that diversion of portal vein blood flow should dilute hepatotropic agents in the systemic circulation. Theoretically, either portacaval shunting or continuous infusion of a high-glucose diet should be effective in reversing most manifestations of the illness, with the exception that portacaval shunting should have little or no beneficial effect on hypoglycemia. Consequently, portacaval shunting is not recommended as a sole form of treatment for those patients who are expected to have frequent episodes of very low blood glucose or for small children in whom shunts may be more likely to close spontaneously. A more practical method was devised to maintain blood glucose at physiologic concentrations or at levels that would prevent stimulation of excess glycogenolysis and glycolysis. This was given enterally either by nasogastric tube or by gastrostomy during night-time sleep, along with a high-starch diet that was consumed at frequent intervals while the patient was awake. Such a regimen has successfully maintained a large number of patients relatively symptom free for more than 10 years and has provided normal or near-normal growth and development [151]. A number of patients can maintain normal blood glucose levels by taking cold, uncooked cornstarch (2 g/kg) at 6-hour intervals [152].
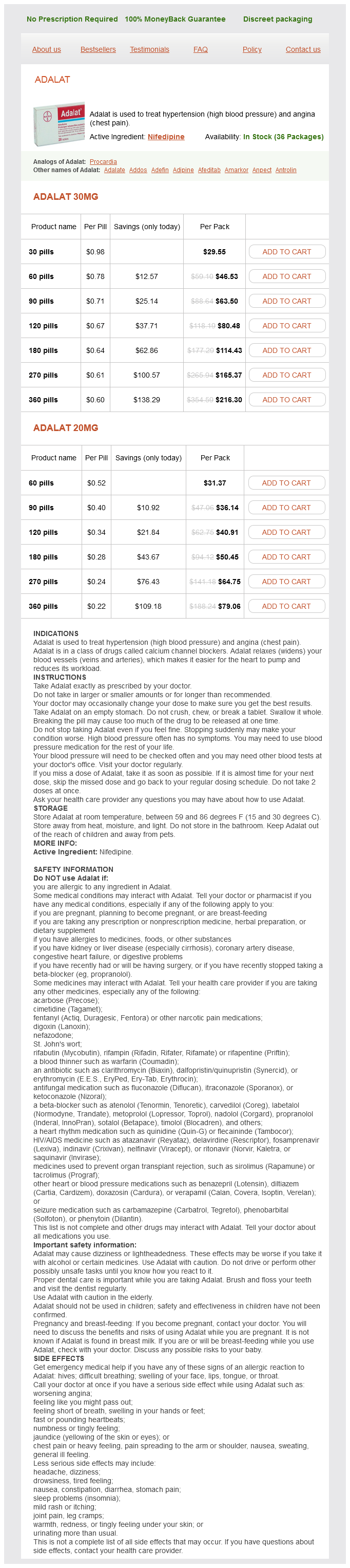
Nifedipine Dosage and Price
Adalat 30mg
- 30 pills - $29.55
- 60 pills - $46.53
- 90 pills - $63.50
- 120 pills - $80.48
- 180 pills - $114.43
- 270 pills - $165.37
- 360 pills - $216.30
Adalat 20mg
- 60 pills - $31.37
- 90 pills - $36.14
- 120 pills - $40.91
- 180 pills - $50.45
- 270 pills - $64.75
- 360 pills - $79.06
Symptoms include fever blood pressure time of day order nifedipine cheap, hepatomegaly, and eosinophilia in approximately 90% of affected patients. Diagnosis is generally made through the demonstration of organisms in percutaneous hepatic biopsy specimens. This section of the liver shows the characteristically cystically dilated bile ducts. Schistosomal organisms infect humans by direct penetration through the skin of cercariae, previously released from a snail host. After penetration, cercariae develop into schistosomulae and eventually migrate to the liver where, in intrahepatic portal venules, they mature and mate. The adult organisms then move within the portal venous system to branches of the inferior (S. Initial T helper 1 and subsequently T helper 2 responses to egg antigens result in the formation of granulomatous lesions which surround the ovum and are composed primarily of eosinophils, epithelioid cells, lymphocytes, and plasma cells [71]. Destruction of small portal radicles occurs, presumably producing the presinusoidal portal hypertension characteristic of hepatosplenic (a) schistosomiasis. Fibrosis and thrombophlebitis of larger portal branches results in the "pipestem fibrosis" described by Symmers [72]. Clinical manifestations of schistosomiasis are protean; distinct clinical syndromes are associated with each stage of infection. Hepatic disease is marked by hepatosplenomegaly; development of hepatic disease appears to correlate with severity of infestation. Symptoms of hepatic disease are few; patients may present with upper gastrointestinal bleeding from esophageal varices as the first sign of disease. Laboratory abnormalities are also few; hypersplenism may result in anemia, thrombocytopenia, and leukopenia. Serum aminotransferases are generally not markedly elevated, while serum alkaline phosphatase may be increased. Ultrasound allows detection and grading of periportal fibrosis, accurate measurement of liver and spleen size, and measurement of portal vein size, as well as detection of intra-abdominal varices. Definitive diagnosis rests upon the isolation of schistosome eggs in stool or urine in S. Numerous eggs are present in the portal tracts (arrows), which are mildly expanded and fibrotic, a reaction to the presence of the eggs. The pharmacologic treatment of choice is praziquantel, 40Ͷ0 mg/kg daily in divided doses. Trials of single-dose combined therapy with ivernectin, albendazole, and praziquantel have also shown promise [73]. Acute variceal hemorrhage is managed in the routine manner; chronic hemorrhage may require variceal banding or, in some cases, shunt placement. The life cycle of these flukes begins when embryonated eggs are ingested by operculate snails. Development into cercariae occurs within this host; after subsequent release the cercariae penetrate fresh water fish and become encysted within their flesh. Injury to the bile ducts occurs and is manifested by adenomatous proliferation and goblet cell hyperplasia [74]. Egg deposition may also be associated with the presence of giant cell reaction in the liver, as well as with portal granulomas. Early or mild disease may be asymptomatic; more severe infections may be with fever, malaise, anorexia, jaundice, and hepatosplenomegaly. Later symptoms involve the consequences of portal hypertension and biliary obstruction. Laboratory findings in late disease include elevations of serum aminotransferases, alkaline phosphatase, and bilirubin. Diagnosis may be made through stool examination, as well as through examination of bile. Endoscopic papillotomy and stone extraction, as well as insertion of endoprostheses, may be required. In long-standing recurrent pyogenic cholangitis, other surgical interventions may be required. Fasciola hepatica Fasciola hepatica is a trematode found worldwide; primary hosts include sheep and cattle. The organisms then migrate through the liver parenchyma until reaching the bile ducts, where they persist. Symptoms and pathologic changes, therefore, reflect not only biliary tract disease as in clonorchiasis but also parenchymal damage, manifested by the presence of necrotic microabscesses within the liver. Endoscopic retrograde cholangiography may also be useful in the biliary phase of disease, both as a diagnostic (identification of eggs and intact flukes, visualization of flukes radiographically) and therapeutic (removal of flukes after sphincterotomy) measure [69]. Because availability of this drug may be an issue, bithionol, 30͵0 mg/kg on alternate days for 10ͱ5 doses may also be used, as may nitazoxanide [24]. Leishmaniasis Visceral leishmaniasis, or kala-azar, caused by Leishmania donovani, is endemic throughout the Mediterranean basin, as well as parts of Africa, South America, Russia, and China. Organisms are inoculated into humans via sandfly bites and are rapidly phagocytosed by dermal macrophages, where they proliferate. Rupture of infected macrophages allows organism spread to reticuloendothelial cells within the liver, spleen, bone marrow, lymph nodes, kidneys, and intestine. The hepatic lesion in older children and adults is characterized by Kupffer cell hyperplasia, many of which contain parasites.