General Information about Moduretic
In the case of high blood pressure, Moduretic helps to minimize back it by lowering the quantity of fluid in the blood vessels. As the quantity of fluid in the blood vessels decreases, the stress on the vessel partitions decreases as nicely. This reduces the workload on the guts, which translates to a lower blood strain studying.
Also, Moduretic isn't suitable for everyone. People who have severe kidney or liver disease, diabetes, or an allergy to sulfa medication should not take this medicine. Additionally, it is important to inform your physician about some other medicines you're taking, including over-the-counter medicine, dietary supplements, and herbal cures, as they could interact with Moduretic.
Amiloride, the other element of Moduretic, is a potassium-sparing diuretic. This signifies that it allows the physique to excrete fluid whereas concurrently retaining potassium. This helps stop a drop in potassium ranges, which can lead to various health problems such as muscle weak point, irregular heartbeats, and fatigue.
The primary operate of Moduretic is to help the physique rid itself of excess fluid, which may trigger swelling and discomfort, in addition to to lower blood strain. So, what exactly makes this medication efficient and the way does it work?
While Moduretic is generally protected for most individuals, like several medicine, it can cause unwanted effects. Some widespread side effects embody dizziness, headache, muscle cramps, increased urination, and nausea. However, if these symptoms persist or turn into extreme, it is essential to seek the assistance of your physician.
It is crucial to notice that Moduretic is a prescription medication and may only be taken under the supervision of a doctor. The dosage and length of remedy will depend upon the severity of your situation and your medical history. It is essential to comply with your physician's instructions carefully and not to alter the dosage or stop taking the medication without consulting them first.
Now, let's delve into how Moduretic works to treat edema and hypertension. Edema is a condition in which excess fluid builds up in the physique and causes swelling. Moduretic works by increasing the production of urine, which allows excess fluid to be drained from the body. This helps reduce the swelling and discomfort brought on by edema.
In conclusion, Moduretic is an effective treatment for treating fluid retention and hypertension. It works by growing urine production and retaining potassium, which helps to alleviate swelling and decrease blood strain. However, it's essential to take this medication as prescribed by your physician and notify them of any concerns or side effects that you could be experience. With proper use and close supervision, Moduretic can present reduction and improve the quality of life for these battling fluid retention and high blood pressure.
To begin with, let's perceive what diuretics are and how they function. Diuretics are drugs that increase the manufacturing of urine, thereby serving to the body get rid of excess fluid. One of the most typical diuretics used to deal with high blood pressure is hydrochlorothiazide. However, the problem with this diuretic is that it can cause potassium ranges in the physique to decrease. This is the place the second active ingredient in Moduretic comes into play.
Moduretic is a prescription treatment that's generally used to treat two medical conditions: fluid retention, also called edema, and high blood pressure. It is a mix drug that contains two lively elements: amiloride, a diuretic, and hydrochlorothiazide, a potassium-sparing diuretic.
Clinical Presentation · Severe and symptomatic hyponatremia should be treated with hypertonic saline (3%) at 1 to 2 mL/kg per hour pulse pressure 95 generic 50 mg moduretic with amex. The objective is to raise sodium by 2 mEq/L per hour (or to >125 mEq/L) until deleterious neurologic symptoms improve. After this, the rate of infusion should be titrated to increase the serum sodium by 0. Acute hyponatremia (<48 hours) may be treated more rapidly than chronic hyponatremia if dictated by neurologic findings. The same parameters apply for rate of sodium correction and monitoring as in conventional therapy. Mild symptoms include headache, nausea, vomiting, confusion, and weakness, which usually occur with a sodium level of less than 129 mEq/L. More severe neurologic manifestations-seizure and coma-are seen usually below a threshold of 120 mEq/L, although there currently is no evidence-based critical sodium level above which neurologic sequelae do not occur. The neurologic manifestations of acute or recurrent symptomatic hyponatremia can be delayed, so continued monitoring is important. In contrast, patients with chronic hyponatremia more often are asymptomatic or have blunted symptoms. In elderly patients with mild chronic hyponatremia, subtle neurocognitive manifestations can occur, with decreased balance, lowered reaction speed, memory loss, and directed gait. Mild hypoosmolar hyponatremia is not independently associated with increased morbidity and mortality. Even so, the underlying etiology needs to be determined because of the potential for other factors. Homeostasis maintains the concentration of sodium in the serum between 138 and 142 mEq/L (normal, 135145 mEq/L) despite variations in water intake. It is one of the most common electrolyte abnormalities found in the inpatient setting, occurring in up to 2. It is not clear whether hyponatremia itself is the cause of a more adverse prognosis or whether it echoes the degree of stress caused by illness. In the Renal Handling of Water the major osmoregulatory hormone is arginine vasopressin, also called antidiuretic hormone, which is synthesized in the paraventricular and supraoptic nuclei of the hypothalamus. It is transported along axons to the posterior pituitary, where it is processed and stored in vesicles. Secretion occurs with a 1% to 2% rise in osmolality (>288 mOsm/kg), as detected by receptors in the anterolateral walls of the hypothalamus adjacent to the third ventricle. Vasopressin secretion is inhibited when the plasma osmolality is lower than 280 mOsm/kg. The major nonosmotic stimulus is a decrease in effective circulating volume, which is detected by baroreceptors in the aortic arch and carotid sinuses. Although this mechanism requires a large drop (10%15%) in blood pressure, the secretory response is more robust than for increases in osmolality. As such, acutely lowered blood pressure can override the inhibitory signal of low osmolality because of the need to maintain perfusion. The renal site of action of vasopressin is the V2 receptors on the basolateral membrane of collecting duct cells in the distal nephron. The hormone-receptor interaction initiates intracellular signaling via cyclic adenosine monophosphatedependent pathways, resulting in translocation of cytoplasmic aquaporon-2 channels to the surface of the collecting duct luminal membrane. A rapid rise in plasma osmolality from aggressive treatment causes water to rapidly shift out of the cells, resulting in demyelination of neurons. In the past, this was termed pontine demyelinosis, but it has also been reported for extrapontine neurons and is now referred to as osmotic demyelination. There is clinical progression from lethargy to a change in affect, to mutism and dysarthria, and finally to spastic quadriparesis and pseudobulbar palsy. Classification and Differential Diagnosis of Hyponatremia 5 Endocrine and Metabolic Disorders Tricyclic antidepressants Selective serotonin reuptake inhibitors Nicotine Adrenaline (epinephrine) High-dose morphine Low-dose morphine Glucocorticoids Fluphenazine (Prolixin) Haloperidol (Haldol) Promethazine (Phenergan) Butorphanol (Stadol) ne t/i nt er na 318 Renal Handling of Sodium In addition to renal water handling, sodium reabsorption and excretion are important for maintenance of water homeostasis. The renin-angiotensin-aldosterone system is activated by reduced arterial perfusion pressure sensed by the juxtaglomerular apparatus of the afferent renal arteriole. Reduced arteriole effective volume (low or perceived) is sensed by the juxtaglomerular apparatus, which secretes renin, activating the renin-angiotensin system. The directly measured osmolality should be Assess clinical volume status Hypovolemic Extrarenal · Gastrointestinal losses · Cerebral salt wasting · Sweat losses · Third spacing losses (burns, pancreatitis, trauma, muscle, peritonitis) Renal · Thiazide diuretic therapy · Cerebral salt wasting · Mineralocorticoid deficiency · Salt wasting nephropathy: · Medullary cystic disease · Chronic interstitial nephritis · Polycystic kidney disease · Analgesic nephropathy · Partial urinary tract obstruction · Chronic glomerulonephritis. The major symptoms and signs of hyponatremia are neurologic in nature and are a clinical manifestation of swelling of the cells in the central nervous system, which results in cerebral edema. The most devastating consequence is herniation due to anatomic limitations on brain volume within the confines of the skull. A major compensatory mechanism in the central nervous system is the extrusion from the cells of intracellular solutes, which prevents further water influx. In the first few hours, inorganic ions (potassium, sodium, chloride) move out of the cell. After a few days of persistent hypoosmolality, the cells further compensate by extruding organic osmoles (glutamate, taurine, inositol). On examination, special attention should be paid to mental status and neurologic abnormalities; manifestations of cardiac, hepatic, or renal disease; and signs of adrenal insufficiency or hypothyroidism. Finally, it should be determined whether the hyponatremia is acute (<48 hours) or chronic, because this can determine the time course of treatment.
These persistently elevated IgG levels can cause some confusion as cross-reactivity to other rickettsia pulse pressure ejection fraction generic moduretic 50 mg with visa. At the time of presentation, a biopsy of rash-involved skin can be performed with immunohistochemical staining of the specimen. The sensitivity of the assay and lack of its wide availability limits the usefulness of this test. Laboratory abnormalities commonly include mild leukopenia, elevated liver transaminases, and total bilirubin. This infection is seen uncommonly in the United States, but is more common in Asia, Africa, and southern Europe. Ehrlichial Infections Ehrlichiosis is a term to define infections caused by bacteria in the family Anaplasmatacea, primarily comprised of the genera Ehrlichia and Anaplasma. The genus Ehrlichia was named after the German-born physician Paul Ehrlich in 1937. In total, three species from the genus Ehrlichia and one species in the genus Anaplasma 1 Other Rickettsial Organisms ed ic 607 Differential Diagnosis Differential diagnosis could include meningococcemia, leptospirosis, measles, mononucleosis, and certain streptococcal and staphylococcal infections. This obligate intracellular pathogen utilizes the nutrients of the cytosol for proliferation and host cell actin elements to propel the organism through the cytosol, to the surface membrane, and onto adjacent endothelial cells. Small and medium-sized blood vessels are most heavily invaded by this pathogen, with invasion of macrophages, monocytes, and hepatocytes to a lesser degree. Invasion of the endothelium results in a local cell injury resulting from oxidative stress. This endothelial injury results in increased vascular permeability and stimulation of inflammatory cytokines, which can progress to multiorgan failure. Unless suffering from multiorgan injury, most patients will defervesce 2 to 3 days after the initiation of treatment, resulting in a typical treatment course of 5 to 7 days of antibiotics. Short courses of doxycycline in young children (<8 years of age),1 as outlined above, have not been associated with discoloration of permanent teeth. Both typically present as an undifferentiated febrile illness, marked by fever, chills, headache, malaise, myalgia, and arthralgia. Patients can present with varying levels of acuity, and rates of complications can vary, depending on the diagnosis. Unfortunately, this is a relatively insensitive assay, with morula found typically in <10% of patients. The diagnosis can also be made by the demonstration of a fourfold change in antibody titers during convalescence; with repeat antibody titers acquired 2 to 4 weeks after symptom onset. However, IgG antibodies may persist for months to years after an infection, thus complicating the interpretation of the assay. Following treatment with doxycycline, a prompt response usually ensues, with marked clinical improvement typically noted within 24 to 48 hours. Pathogenesis Following inoculation, these small organisms spread initially via the lymphatic system to regional nodes, followed by hematogenous dissemination. Dantas-Torres F: Biology and ecology of the brown dog tick, Rhipicephalus sanguineus, Parasit Vectors 3:111, 2010. Mansueto P, Vitale G, Cascio A, et al: New insight into immunity and immunopathology of Rickettsial diseases, Clin Dev Immunol 2012:126, 2012. A typical course of doxycycline is 5 to 10 days, given at least 3 days after defervescence, which typically occurs within 48 hours of initiation of therapy. Diagnosis and Differential Diagnosis Rubella is normally a mild, self-limiting rash-fever illness. Rubella spreads mainly via aerosols, but in contrast to measles, a close and prolonged contact is usually required for transmission. In unvaccinated populations, approximately 15% to 20% of women of childbearing age are susceptible to the disease and can become infected during pregnancy. However, routine rubella vaccination has not yet been introduced in many developing countries in Africa and Asia, and endemic virus continues to circulate in many countries worldwide. Reinfections with rubella virus are possible and have been reported more often after vaccination than after natural primary infection. Normally, reinfections are asymptomatic and congenital malformations seem to be very rare. Laboratory confirmation is necessary to exclude other rash-fever diseases such as infections caused by measles virus, parvovirus B19, human herpesvirus 6, dengue virus, enteroviruses, and group A Streptococcus. Rubella-specific immunoglobulin (Ig) M, which normally persists for 2 to 3 months but occasionally much longer, points to a current or recent infection. False-positive IgM results occur more often with indirect serologic assays than with antibody-capture assays and are sometimes linked to rheumatoid factor or cross-reacting non-rubella IgM antibodies. A significant increase in rubella-specific IgG antibody titer between acute and convalescent phase sera also indicates a recent infection with rubella virus. Fetal infections are usually diagnosed either by rubella-specific IgM in fetal blood or by rubella virus in amniotic fluid. Detection of rubella-specific IgG antibodies at a time when maternal antibodies have normally disappeared also suggests a congenital infection. The incubation period lasts about 2 weeks (range, 1223 days), at the end of which a maculopapular rash can appear, which spreads from the face to the trunk and limbs. Lymphadenopathy can develop before the rash and can persist for up to 2 weeks after rash. Especially in adults, a prodromal phase may be observed with fever, malaise, and other uncharacteristic symptoms. Viremia occurs for about 1 week before onset of rash, and virus can be transmitted from around 1 week before, until up to nearly 2 weeks (and exceptionally longer) after onset of rash. Rubella infection during pregnancy requires a careful laboratory diagnosis, comprehensive risk assessment, and counseling.
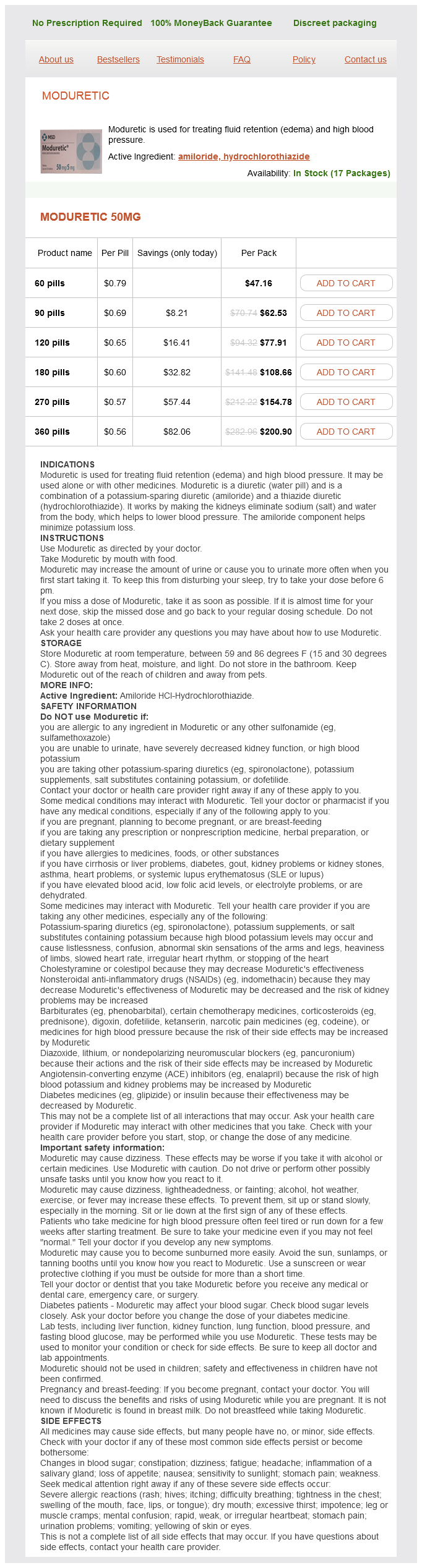
Moduretic Dosage and Price
Moduretic 50mg
- 60 pills - $47.16
- 90 pills - $62.53
- 120 pills - $77.91
- 180 pills - $108.66
- 270 pills - $154.78
- 360 pills - $200.90
During the icteric phase arrhythmia associates of south texas 50 mg moduretic buy with amex, total serum bilirubin rises but generally does not exceed 10 mg/dL. In most patients, jaundice lasts 2 weeks and a complete clinical and biochemical recovery can be expected in 2 to 3 months. Treatment Given the self-limiting nature of acute hepatitis A, treatment is predominately supportive. Caution should be taken when using hepatotoxic medications or medications metabolized predominately in the liver. Rarely, acute liver failure with encephalopathy and impaired synthetic function can occur. Individuals presenting with acute liver failure are more appropriately managed at a liver transplant center. In the United States, the Advisory Committee on Immunization Practices recommends that all children at age 1 year be vaccinated. Development of cirrhosis has been described as a consequence of chronic infection. Interestingly, males are more affected than females in sporadic infections, but this gender bias is not observed during epidemics. Testing is limited to research laboratories and can be obtained through the Centers for Disease Control and Prevention. The incubation period is between 15 and 60 days, and if symptoms arise, they generally consist of anorexia, nausea, vomiting, diarrhea, and abdominal pain. A notable exception to the generally favorable outcome is an increased risk of acute liver failure among pregnant women during the second and third trimesters in endemic regions. Low-income regions (SubSaharan Africa and parts of South Asia) have high endemicity levels and very few susceptible adolescents and adults. The virus is classified into 10 major genotypes (A through J) that have a distinct geographical distribution. Patients who develop acute liver failure should be managed at a liver transplant center. If this is unsuccessful, then antiviral therapy with peginterferon (Pegasys)1 or ribavirin (Rebetol)1 may be considered. In immunocompromised individuals therapy with peginterferon1 or ribavirin1 may be considered. Resolution of acute infection occurs in 95% of persons exposed as adults, but chronic infection ensues in more than 90% of persons exposed as infants. This classification is useful for providing advice on prognosis and need for treatment. Approximately 25% to 40% of persons with chronic infection will be at risk for development of cirrhosis. Once cirrhosis develops, the 5-year cumulative incidence of decompensated liver disease (ascites, variceal hemorrhage, hepatic encephalopathy) is approximately 20%, and the annual risk of hepatocellular carcinoma is 2% to 5%. High endemic areas, defined by greater than or equal to 25% prevalence of sporadic non-A, non-B hepatitis, include parts of Central America and Mexico, Africa, the Middle East, and most of Asia. Endemic areas, defined as less than 25% prevalence of sporadic non-A, non-B hepatitis, include the United States, Europe, Russia, and parts of South America. For persons with evidence of acute liver failure, prompt institution of antiviral therapy with a potent nucleos(t)ide analog and referral to a transplant center is recommended. The decision to treat persons outside these parameters should be individualized based on their risk for complications and risk of therapy. Peginterferon is contraindicated in persons with decompensated cirrhosis, autoimmune illnesses, or active psychiatric illness. This is seen only in persons who acquire the infection at birth or infancy and that persists for two to three decades of life. Acute liver failure is observed more commonly with coinfection than superinfection. Recommendations for Identification and Public Health Management of Persons with Chronic Hepatitis B Virus Infection. Low-prevalence regions include North America, most of Western Europe, and Australia. Liver transplantation with the use of hepatitis B immune globulin is an option for patients with decompensated liver disease. Novel agents blocking viral entry and posttranslational prenylation are currently being investigated in clinical studies. Acknowledgments: this work is supported by the Intramural Research Program of the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. The highest prevalence is observed in Central Africa, Central Asia, and the Amazon. Epidemiology ed ic can be cured after 8 to 12 weeks of safe oral regimens combining antiviral agents. Nosocomial exposure to contaminated blood or blood products and poorly sterilized or reused contaminated medical equipment remains an important risk, especially if strict universal precautions are not instituted. In the United States, it is the leading bloodborne pathogen and infects over 3 million Americans. In the United States, the incidence reached a peak in the 1970s and 1980s and then steeply declined; in the last decade there has been a resurgence of new incident cases linked to a widespread opioid epidemic. There are seven known families of virus, commonly known as genotypes 1 through 7, many with subtypes.