General Information about Mesalamine
Mesalamine, commonly known as Asacol, is a vital medication used in the remedy and prevention of inflammatory bowel illness (IBD) particularly ulcerative colitis. It is an anti-inflammatory drug that acts specifically within the intestines to scale back inflammation and different symptoms associated with this persistent illness.
Apart from treating energetic symptoms, Asacol can be used as upkeep remedy to stop flare-ups and preserve remission in sufferers with ulcerative colitis. Studies have shown that long-term use of mesalamine reduces the variety of relapses and helps patients preserve their quality of life. It can also be believed that early use of mesalamine can forestall the development of ulcerative colitis, reducing the dangers of severe complications.
However, like all treatment, mesalamine isn't suitable for everybody. It shouldn't be used by people who're allergic to 5-ASA or any other parts of the medication. Patients with kidney or liver problems, blood disorders, or a historical past of coronary heart illness should seek the guidance of their doctor before starting mesalamine remedy. It can be important to tell the doctor of another medicines or dietary supplements being used to stop potential drug interactions.
Mesalamine has been proven to be an efficient treatment for ulcerative colitis, with minimal unwanted effects. Common unwanted effects embrace nausea, diarrhea, and headache, but they are often minor and subside with continued use. It can additionally be considered secure for long-term use, with studies showing no important antagonistic results even after years of use.
The cause of ulcerative colitis remains to be not totally understood, however it's believed to be because of an irregular immune response within the intestine. This response leads to the manufacturing of chemical compounds that trigger inflammation. This is where mesalamine comes into play, as it acts by blocking the production of those inflammatory chemical compounds.
In conclusion, mesalamine is a vital medicine within the administration of ulcerative colitis. Its capability to minimize back irritation and stop flare-ups has proven to be beneficial for sufferers, serving to them obtain and maintain remission. With its minimal unwanted aspect effects and security for long-term use, it has become a go-to possibility for physicians in treating this continual inflammatory bowel disease. However, it's at all times important to seek the guidance of a physician before taking any treatment to ensure its suitability and to watch for potential opposed effects.
Asacol is on the market in varied forms, including tablets, capsules, and suppositories, to suit different patients' wants. It is taken orally, and the medicine is released within the gut, the place it acts instantly on the inflamed tissue. This makes it a useful choice for sufferers who have issue taking oral medication or those who require rectal remedy.
Ulcerative colitis is a kind of IBD that causes irritation and ulcers within the lining of the big intestine and rectum. This condition is characterised by symptoms such as abdominal ache, rectal bleeding, diarrhea, and weight reduction. It is a persistent illness that can severely influence a person's quality of life, resulting in a number of hospitalizations and surgical procedures in severe instances.
The major mechanism of motion of mesalamine is thru its anti-inflammatory properties. It is a sort of medication called a 5-aminosalicylic acid (5-ASA) that's much like the natural substances present in our physique. It works by interfering with the manufacturing of drugs that promote inflammation, together with prostaglandins, leukotrienes, and cytokines.
Intermediate graft failures include those between 30 days and 2 years and are generally attributed to the proliferation of intimal hyperplasia at the anastomoses or prior valve sites within the graft medications guide generic mesalamine 400 mg visa. The posterior wall (B) and anterior wall (C) are aligned with separate strands of suture to avoid a "purse string" effect on the suture line. This is performed with generous spatulation of each vein hood to create a widely patent vein-to-vein anastomosis. Given their thin-walled nature, arm vein grafts are also quite prone to twisting and kinking, and special care must be taken during the tunneling process to avoid these problems. The more proximal arm veins can be relatively large, and it is often advantageous to use one or more of the segments in a nonreversed fashion to better match the graft to the inflow vessel size. Not surprisingly, the results of reoperative infrainguinal bypass surgery do not match those of primary reconstruction. With autogenous vein, 5-year patency rates of 60% and limb salvage rates of 70% to 80% have been reported. Given the known incidence of graft failure and the potentially dire consequence in terms of limb salvage or preservation of limb function in a patient with limited options for secondary or tertiary bypass, the ability to maintain graft patency through early identification and prompt correction of graft stenoses is of paramount importance. Nevelsteen A, Wouters L, Suy R: Aorto-femoral Dacron reconstruction for aortoiliac occlusive disease: a 25-year survey, Eur J Vasc Surg 5:179, 1991. Paper presented at 17th International Congress of Endovascular Interventions, Phoenix, February 12, 2004. Leriche R, Morel A: the syndrome of thrombotic obliteration of the aortic bifurcation, Ann Surg 127:193, 1948. Caes F, Cham B, Van den Brande P, et al: Small artery syndrome in women, Surg Gynecol Obstet 161:165, 1985. Shareghi S, Gopal A, Gul K, et al: Diagnostic accuracy of 64 multidetector computed tomography angiography in peripheral vascular disease, Catheter Cardiovasc Intervent 75:2331, 2010. Stadler P, Dvoracek L, Vitasek P, et al: Is robotic surgery appropriate for vascular procedures Schanzer A, Mega J, Meadows J, et al: Risk stratification in critical limb ischemia: derivation and validation of a model to predict amputation-free survival using multicenter surgical outcomes data, J Vasc Surg 48:14641471, 2008. Bandyk D, Johnson B, Gupta A, et al: Nature and management of duplex abnormalities encountered during infrainguinal vein bypass grafting, J Vasc Surg 24:430, 1996. Rosenthal D, Dickson C, Rodriquez F, et al: Infrainguinal endovascular in situ saphenous vein bypass: ongoing results, J Vasc Surg 20:389, 1994. A variety of fibromuscular lesions have been described, but the most common is medial fibroplasia. Occasionally, such lesions may be found in the carotid and other vascular beds, but most commonly they are limited to the renal arteries. Most do not progress to impair renal function, although some lead to arterial dissection and/or thrombosis with loss of the kidney. Its presence and severity are related to age and the presence of other atherosclerotic disease of the descending aorta and lower extremities. A corollary observation is that renovascular hypertension resulting from these lesions is now most commonly superimposed gradually upon preexisting essential hypertension. Hence, the blood pressure response and "cure" rates after successful restoration of blood flows to the kidney are limited by preexisting conditions. Thanks to recent advances in vascular imaging, more patients than ever before are being identified with some degree of atherosclerotic or fibromuscular renovascular disease. Many of these lesions are of minor hemodynamic importance at the time of detection. Some reach a degree at which perfusion pressures and intrarenal hemodynamics are altered, leading to changes in blood pressure regulation and renal function. Understanding the pathways by which renovascular disease affects cardiovascular and renal disease is important for both diagnosis and for defining optimal management using tools both to block the renin-angiotensin system and to restore the circulation. This chapter will examine the pathophysiology of renovascular lesions regarding blood pressure control, ischemic nephropathy, and clinical syndromes such as flash pulmonary edema. Specific issues regarding diagnostic evaluation and management are addressed elsewhere (see Chapter 23). A wide range of lesions can affect the renal blood supply, some of which are summarized in Box 22-1. Historically, recognition of renovascular disease resulted from searching for underlying causes of hypertension. This followed the seminal observations of Goldblatt more than 70 years ago2 that renal artery constriction produced a rise in arterial pressure in the dog. These studies were among the first to establish a primary role of the kidney in overall blood pressure regulation. Renovascular hypertension produced by a "clipped" renal artery remains among the most widely studied experimental forms of angiotensin-dependent hypertension. Importantly, a fall in renal blood flow is accompanied by decreased oxygen consumption, partly due to reduced metabolic demands of filtration and tubular solute reabsorption. Alternative terms proposed included azotemic renovascular disease and hypoperfusion injury. Epidemiology of Renal Artery Disease Fibromuscular disease may be identified in 1% to 3% of normal kidney donors subjected to angiography before donor nephrectomy. Data indicate that activation of renal venous renin activity from stenotic kidney (closed circles), nonstenotic kidney (open circles), and aorta (closed squares) occurred only after a translesional gradient between 10 and 20 mmHg was created. Such a gradient usually requires advanced occlusive disease, usually more than 70% lumen occlusion. In some instances, an abrupt fall in poststenotic pressure develops beyond a subcritical range of stenosis. Kidneys with a baseline renal artery disease classification of less than 60% stenosis have 11. Intrarenal vascular lesions are commonly observed in the course of various nephropathies, many of which have an ischemic component.
In most patients and virtually all patients operated on for aortic aneurysmal disease treatment research institute purchase line mesalamine, graft excision without revascularization can be expected to result in lower-extremity amputation. Total Graft Excision with In Situ Replacement Using Prosthetic Graft In situ replacement of an infected graft with a new prosthetic graft is technically the simplest method of revascularization and avoids the potential for aortic stump blowout. However, replacing an infected prosthetic graft with a new prosthesis poses the very real potential for recurrent graft infection. In situ prosthetic replacement may be best used as a salvage operation for unstable patients with either aortoenteric fistula or ruptured proximal pseudoaneurysms. Fortunately, the reported rates of clinically apparent reinfection following in situ replacement for aortoenteric fistula is surprisingly low (<15%). Recurrent infection in the setting of gross graft infection has been disappointing. The authors use in situ replacement with prostheses as a bridge to definitive therapy with autogenous replacement at a later operation. The advent of antibiotic-bonded Dacron grafts appeared to offer improved results for in situ prosthetic replacement. This modality seems to be most appropriate for treatment of graft infections with biofilm-producing S. Similar findings have recently been reported using silver-coated polyester grafts for in situ replacement. In a series of 24 patients with a variety of polymicrobial graft infections, Batt et al. It is not appropriate for patients 59 with early graft infections because the entire graft is almost invariably involved. In our experience, subtotal graft excision can be attempted if the body of the graft is found to be incorporated at the time of surgical exploration. The body of the graft can be explored prior to violating the clearly infected portion. The wound is closed, the infected portion of the graft is removed, and the reconstruction completed. Subtotal graft excision should only be considered in high-risk patients with late-occurring graft infections. Such patients should be followed closely, and infection of the residual graft should be anticipated. Animal studies have demonstrated the allograft is relatively resistant to infection when antibiotic loaded. In three patients, allograft side branch rupture resulted in three aortoenteric fistulas that were uniformly fatal. In a recent study of 110 consecutive patients with aortic infections, Bisdas et al. During a mean follow-up of 36 months, 6% required reoperation for graft deterioration, but no recurrence of infection was noted. Graft Infection Following Endovascular Repair Graft infection following stent graft repair of aneurysm is becoming more frequently reported. As of 2010, there have been 102 reports of abdominal endograft infections in the literature. The typical clinical presentation and radiographic finding associated with stent graft infections are not well described and await a more mature experience with these endovascular techniques. Infected grafts have been associated with highly virulent organisms including Propionobacterium, Staphylococcus, Streptococcus, and Enterobacter. On the other hand, treatment of infected thoracic endografts should include graft excision and bypass with antibiotic-soaked prosthetic graft or cryopreserved allograft if more virulent organisms are present. This conduit has proven to be the most resistant conduit to infection, has unchallenged patency rates, avoids the risk of aortic stump blowout, and rarely degenerates. Patients with overwhelming sepsis may be better served by extra-anatomical bypass and graft excision. The only downside to this management strategy is the length of the operative procedure. Treatment of Peripheral Graft Infections the incidence of graft infection following infrainguinal peripheral arterial reconstruction ranges from 2%-5%. Late infections of autogenous grafts are very rare and most frequently occur in thrombosed grafts. In a series of 68 patients with infected infrainguinal autogenous grafts, Treiman et al. A patient presenting with bleeding from the site of an infrainguinal arterial reconstruction should be considered to have a graft infection, and operative exploration is mandatory. In less obvious cases, the diagnosis of such infections is similar to that of aortic graft infections. Computed tomography scanning is most helpful, and will demonstrate perigraft fluid collections and inflammation. Magnetic resonance imaging can successfully diagnose infected prosthetic grafts that have surrounding perigraft fluid. The grafts are easily accessible, and ultrasound is particularly good at identifying perigraft fluid. The mainstay of therapy is arterial reconstruction through uninfected fields and graft removal. In patients with occluded grafts who do not have limb-threatening ischemia, the graft can be excised without arterial reconstruction. However, patients who were operated on for limb-threatening ischemia who undergo graft excision can be anticipated to need revascularization or face inevitable amputation. In patients who will require concurrent revascularization at the time of infected graft excision, the management options are different for prosthetic grafts versus autogenous graft. In virtually all cases of prosthetic graft infection, the entire graft is involved in the infectious process.
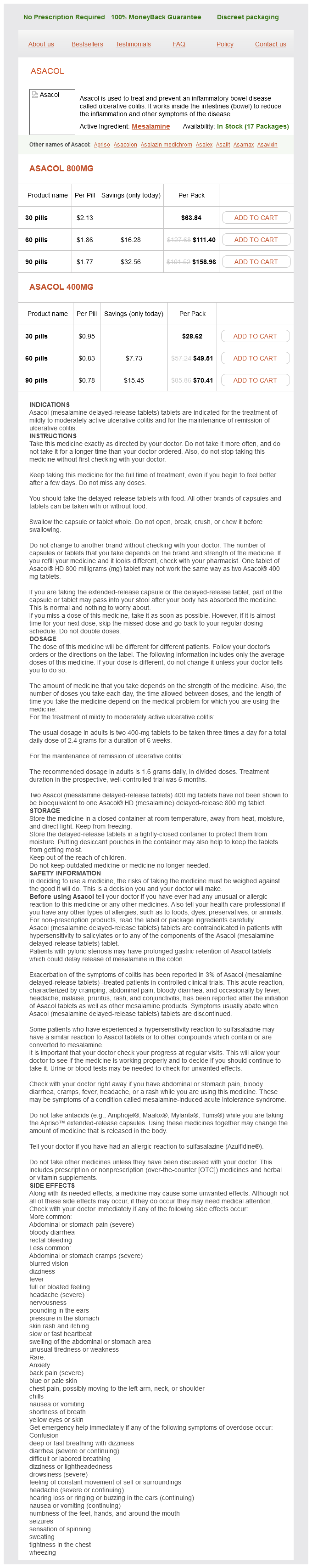
Mesalamine Dosage and Price
Asacol 800mg
- 30 pills - $63.84
- 60 pills - $111.40
- 90 pills - $158.96
Asacol 400mg
- 30 pills - $28.62
- 60 pills - $49.51
- 90 pills - $70.41
Milhaud D medicine ball chair mesalamine 800 mg lowest price, Popp J, Thouvenot E, et al: Mechanical ventilation in ischemic stroke, J Stroke Cerebrovasc Dis 13:183188, 2004. Second European-Australasian Acute Stroke Study Investigators, Lancet 352:12451251, 1998. A science advisory from the American Heart Association/American Stroke Association, Stroke 40:29452948, 2009. Furlan A, Higashida R, Wechsler L, et al: Intra-arterial prourokinase for acute ischemic stroke. Ogawa A, Mori E, Minematsu K, et al: Randomized trial of intraarterial infusion of urokinase within 6 hours of middle cerebral artery stroke, Stroke 38:26332639, 2007. The Penumbra Pivotal Stroke Trial Investigators: the penumbra pivotal stroke trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusion, Stroke 26612666, 2009. Bratane B, Bouley J, Schneider A, et al: Granulocyte colony stimulating factor delays mismatch evolution and reduces final infarct volume in permanent suture and embolic rat focal cerebral ischemia models, Stroke 40:31023106, 2009. Fisher M: New approaches to neuroprotective drug development, Stroke 42:S24S27, 2012. Detre J, Duong T: Magnetic resonance imaging of ischemic penumbra: new techniques: c. In Donnan G, et al, editors: the ischemic penumbra, New York, 2007, Taylor & Francis Inc, pp 234240. Kane I, Carpenter T, Chappell F, et al: Comparison of 10 different magnetic resonance perfusion imaging processing methods in acute ischemic stroke, Stroke 38:31583164, 2007. Azzimondi G, Bassein L, Nonino F, et al: Fever in acute stroke worsens prognosis: a prospective study, Stroke 26:20402043, 1995. Castillo J, Davalos A, Marrugat J, et al: Timing for fever-related brain damage in acute ischemic stroke, Stroke 29:24552460, 1998. Georgiadis D, Schwarz S, Kollmar R, et al: Endovascular cooling for moderate hypothermia in patients with acute stroke: first results of a novel approach, Stroke 32:25502553, 2001. Slotboom J, Kiefer C, Brekenfeld C, et al: Locally induced hypothermia for treatment of acute ischaemic stroke: a physical feasibility study, Neuroradiology 46:923934, 2004. Milhaud D, Thouvenot E, Heroum C, et al: Prolonged moderate hypothermia in massive hemispheric infarction: clinical experience, J Neurosurg Anesthesiol 17:4953, 2005. Vahedi K, Hofmeijer J, Juettler E, et al: Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials, Lancet Neurol 6:215222, 2007. Decompressive surgery for the treatment of malignant infarction of the middle cerebral artery-outcome results [abstract], Int J Stroke 1:s38, 2006. Protocol for a randomised controlled trial of decompressive surgery in space-occupying hemispheric infarction, Trials 7:29, 2006. Britton M, de Faire U, Helmers C, et al: Arrhythmias in patients with acute cerebrovascular disease, Acta Med Scand 205:425428, 1979. Al-Sadat A, Sunbulli M, Chaturvedi S: Use of intravenous heparin by North American neurologists: do the data matter Moonis M, Fisher M: Considering the role of heparin and low molecular-weight heparins in acute ischemic stroke, Stroke 33:19271933, 2002. Sandercock P: Full heparin anticoagulation should not be used in acute ischemic stroke, Stroke 34:231232, 2003. Martí-Fàbregas J, Mateo J: Old and new anticoagulant agents for the prevention and treatment of patients with ischemic stroke, Cerebrovasc Dis 27(Suppl 1):111119, 2009. Abciximab in acute ischemic stroke: a randomized, double-blind, placebo-controlled, dose-escalation study. Abciximab Emergent Stroke Treatment Trial Investigators: Emergency administration of abciximab for treatment of patients with acute ischemic stroke: results of a randomized phase 2 trial, Stroke 36:880890, 2005. Belayev L, Bus to R, Zhao W, et al: Effect of delayed albumin hemodilution on infarction volume and brain edema after transient middle cerebral artery occlusion in rats, J Neurosurg 87:595601, 1997. Belayev L, Liu Y, Zhao W, et al: Human albumin therapy of acute ischemic stroke: marked neuroprotective efficacy at moderate doses and with a broad therapeutic window, Stroke 32:553560, 2001. Belayev L, Pinard E, Nallet H, et al: Albumin therapy of transient focal cerebral ischemia: in vivo analysis of dynamic microvascular responses, Stroke 33:10771084, 2002. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists, Stroke 40:2276, 2009. Kleindorfer D, Panagos P, Pancioli A, et al: Incidence and short-term prognosis of transient ischemic attack in a population-based study, Stroke 36:720723, 2005. Amarenco P, Labreuche J: Lipid management in the prevention of stroke: review and updated meta-analysis of statins for stroke prevention, Lancet Neurol 8:453463, 2009. Rashid P, Leonardi-Bee J, Bath P: Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review, Stroke 34:27412748, 2003. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack, Lancet 358:10331041, 2001. Halliday A, Mansfield A, Marro J, et al: Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomized controlled trial, Lancet 363:14911502, 2004. Brott T, Broderick J, Kothari R, et al: Early hemorrhage growth in patients with intracerebral hemorrhage, Stroke 28:15, 1997. Broderick J, Connolly S, Feldmannn E, et al: Guidelines for the management of spontaneous intracranial hemorrhage in adults, 2007 update, Stroke 38:20012023, 2007. Poungvarin N, Bhoopat W, Viriyavejakul A, et al: Effects of dexamethasone in primary spontaneous intracerebral hemorrhage, N Engl J Med 316:12291233, 1987. Lacut K, Bressollee L, Le Gal G, et al: Prevention of venous thrombosis in patients with acute intracerebral hemorrhage, Neurology 65:865869, 2005. Iyer, Jonathon Habersberger, Jiri Vitek, Christina Brennan, Gary Roubin single-center series of patients. To maximize the luminal result, a long inflation was performed using a 5-mm over-the-wire balloon; the center port of this balloon could accommodate a 0.