General Information about Mentat DS syrup
In addition to these key ingredients, Mentat DS syrup additionally contains different natural herbs and elements like Jyotishmati, Vacha, and Jatamansi, all of which work collectively to enhance neurological functions and promote general well-being.
Neurodegenerative issues are characterised by a progressive decline within the functionality and construction of the central and peripheral nervous system. These problems can manifest in various varieties, together with Parkinson’s illness, Alzheimer’s disease, multiple sclerosis, and Huntington’s disease, to name a quantity of. These circumstances are attributable to the degeneration of neurons, resulting in a decline in cognitive and motor features, which can considerably impact an individual’s high quality of life.
Mentat DS syrup is a product of the renowned pharmaceutical firm Himalaya Herbals, identified for its dedication to offering pure and high-quality products. The syrup is a blend of assorted pure elements, including Brahmi, Ashwagandha, Yashtimadhu, and Shankhapushpi, which are scientifically confirmed to promote healthy brain perform. These components work synergistically to enhance brain perform and improve the activity of neurotransmitters, the chemical messengers that transmit signals between neurons.
Yashtimadhu, generally often known as licorice, is another very important ingredient in Mentat DS syrup. It has been utilized in conventional medication for its antioxidant, anti-inflammatory, and anti-stress properties. Yashtimadhu helps to guard the mind cells from oxidative damage, a standard factor in neurodegenerative problems. It also helps to manage the release of cortisol, the hormone answerable for the body’s stress response, thus promoting a way of calm and relaxation.
Mentat DS syrup is a unique and efficient phytopharmaceutical formulation that has gained reputation in recent times for its potential in enhancing and improving neurological features in people with neurodegenerative issues. It is a specially crafted syrup, derived purely from pure elements and herbs, making it a secure and reliable different to traditional medicines.
Brahmi, also recognized as Bacopa monnieri, is likely certainly one of the key elements in Mentat DS syrup. It has been utilized in conventional Ayurvedic medicine for centuries for its position in improving memory, concentration, and studying capacity. Scientific studies have also proven that Brahmi has a positive effect on brain function, notably in individuals with neurodegenerative problems. It has been discovered to increase the levels of neurotransmitters like serotonin, acetylcholine, and dopamine, which play an important position in regulating mood, memory, and other cognitive capabilities.
Another important ingredient in Mentat DS syrup is Ashwagandha, also known as Withania somnifera. It is famend for its adaptogenic properties, which help the physique to adapt to varied types of stress, together with physical, emotional, and mental stress. Ashwagandha also has neuroprotective results, meaning it helps to guard the brain cells from damage and enhance their function. Studies have proven that it can improve reminiscence, focus, and cognitive performance in people with gentle cognitive impairment.
Mentat DS syrup has been clinically confirmed to be effective in enhancing brain operate and improving the signs of neurodegenerative disorders. It supplies a protected and reliable different to conventional medications, which can often cause adverse unwanted effects. The syrup is suitable for people of all ages and can be utilized as a preventive measure to take care of mind health or as a therapy for current conditions.
In conclusion, Mentat DS syrup is a potent brain tonic that has revolutionized the management of neurodegenerative issues. Its natural and holistic method makes it an ideal selection for these seeking to improve brain perform with out the chance of dangerous unwanted effects. With its unique mix of pure ingredients, Mentat DS syrup is a sworn statement to the rising interest in herbal medication and its potential in improving overall health and well-being.
Shankhapushpi, a herb that grows in the Himalayas, is another key ingredient that offers Mentat DS syrup its unique properties. Shankhapushpi has been used traditionally as a brain tonic, revered for its ability to improve cognitive functions and enhance memory. It also helps to cut back the levels of stress and anxiety, which might considerably affect brain operate.
Bifocal spectacles may also be necessary for some forms of accommodative esotropia medicine logo buy cheap mentat ds syrup 100 ml on line. Esotropia caused by paralysis of a lateral rectus muscle, a 6th cranial nerve palsy, occurs much more frequently in children than in infancy. An older child may present with complaints of diplopia or a face turn or closure of 1 eye to avoid diplopia, whereas a younger child may present with only the esotropia because of rapid development of suppression to eliminate diplopia. Neurologic investigation is indicated if the history does not support a benign etiology or the paralysis does not spontaneously abate in a few weeks (a so-called benign 6th nerve palsy believed to be postviral in origin) or if the child demonstrates other neurologic impairment or has papilledema. Infantile exotropia presents as a large deviation of the eyes prior to 6 months of age. It is, however, commonly associated with craniofacial disorders or neurologic impairment. Surgery may be done early in life, but these patients are less likely to obtain good binocular vision than infantile esotropes. Because the child maintains the ability to keep the eyes aligned part of the time, amblyopia is uncommon. Diplopia is prevented by active cortical suppression of input from the portion of the retina of the deviated eye that overlaps the central view of the fixating eye. When the eyes are straight, the child generally maintains normal binocular function, including stereopsis. Treatment options include part-time patching, additional minus power spectacles in patients with myopia, orthoptic exercises, and surgery. A small vertical deviation in association with a larger amount of horizontal strabismus, however, is common, and is managed in conjunction with the horizontal deviation. If the left eye is not aligned, it will need to move to look at the fixation target. If there is no movement of the left eye, the test needs to be repeated by occluding the left eye and watching for movement of the right eye. The deviation is completely controlled with glasses at both distant (middle) and near (bottom) fixation distances. The incidence and degree of myopia increase with age, especially during growth spurts, as in adolescence. There is a complex interaction between genetic and environmental factors in the development of myopia. The incidence of myopia varies with ethnicity and geographic regions and has been increasing in prevalence over the past 50 years. There have been several genetic markers linked to myopia but the increasing frequency among younger generations suggests environment plays an important role. The increase in prevalence from 10-90% in some populations is a public health concern, particularly with high myopia. Myopia can be associated with increased risk of retinal detachment, early cataract, and glaucoma. This can result in decreased vision even with spectacle or contact lens correction. Myopia may be associated with other ocular abnormalities, such as keratoconus (central conical protrusion of the cornea), cataracts, ectopia lentis (dislocated lens), spherophakia (overly spherical lens), glaucoma, and medullated (myelinated) nerve fibers. Children with high degrees of myopia may have an underlying systemic association, such as Marfan, Stickler, Noonan, or Down syndromes. If myopia is sufficient to produce visual symptoms, spherical concave (minus) lenses in the form of spectacles or contact lenses are prescribed to correct the refractive error. Prescription changes may be needed every 1-2 years and more often during growth spurts. In some children, the "paralysis" is actually caused by an anatomic abnormality of the superior oblique tendon. Acquired causes of a superior oblique palsy include trauma, central nervous system abnormalities, or brain tumors. Children with a superior oblique paralysis of any cause frequently present with a head tilt and face turn toward the side opposite the paralyzed superior oblique muscle. If there is a question as to the timing of the onset of the superior oblique palsy, a review of pictures at a younger age may be helpful in determining chronicity. An eye muscle disorder needs to be ruled out in any child with a chronic abnormality of head position. The anomalous head position and hypertropia caused by a superior oblique paralysis can be improved by eye muscle surgery in most instances. Refractive errors may be similar (isometropia) or different (anisometropia) between the 2 eyes. Myopia In patients with myopia, the parallel rays of light in the resting (nonaccommodating) eye are focused in front of the retina. The process of accommodation (focusing), which alters the shape of the lens, can compensate for some degrees of hyperopia. Because most children have a tremendous range of accommodation, mildly hyperopic children can see clearly without any visual symptoms. Moderate to severely hyperopic children may be unable to fully compensate through accommodation. The greater accommodative effort may lead to symptoms of "eyestrain," which consist of headaches, fatigue, or eye rubbing. These symptoms may lead to a lack of interest in reading or in prolonged close work. Some children have a decreased ability to accommodate, or accommodative insufficiency, and are symptomatic even with low degrees of hyperopia. If hyperopia produces symptoms or causes esotropia, spherical convex (plus) lenses usually in the form of glasses are prescribed to correct the refractive error.
Family history often reveals another relative with the disease or recalls a death from an infection in a young child medications 512 order 100 ml mentat ds syrup otc. The diagnosis is made by performing neutrophil function tests, such as dihydrorhodamine or nitroblue tetrazolium testing, which demonstrate the defective neutrophil oxidation. Positive findings on neutrophil function tests are confirmed via immunoblot or genetic assays. Most adenitis caused by mycobacteria in the United States is caused by atypical strains that are not serious pathogens in the immunocompetent host. Several historical and clinical criteria can be used to differentiate tuberculous adenitis from atypical mycobacterial infections. Most children with tuberculosis have a history of exposure to an adult with active tuberculosis. Infection with atypical mycobacteria is more common in the southern parts of the United States. Children with tuberculous adenitis may have hilar lymphadenopathy because the lungs are usually the source of primary infection. Evidence of extralymphatic disease is also common in children with tuberculosis; such disease includes pneumonia, pleural effusions, bone marrow suppression, liver function abnormalities, and miliary disease. Disseminated (miliary) tuberculosis may manifest with diffuse lymphadenopathy and should be considered if pulmonary infiltrates and systemic symptoms are present. The most common mycobacterial infection in children in the United States is the infection of the lymph nodes with the atypical mycobacteria, primarily M. The lymph nodes involved are usually tender, unilateral and cervical in most infections, presumably because the organism enters via the oropharynx. Most frequently, a previously healthy child presents with a mass that is really unilateral lymphadenitis or adenopathy in the cervical, submandibular, or submaxillary region. Although fever may be present, other significant systemic symptoms are usually not present. In a small number of patients, the affected node spontaneously ruptures and drains before the visit to the physician. The drainage is not usually grossly purulent and may be a clue that atypical mycobacteria are the cause of the infected node. The gold standard for diagnosis of lymphadenitis caused by atypical mycobacteria is acid-fast staining and culture of the excised node. Incision and drainage or needle aspiration of these nodes may lead to chronically draining sinus tracts, which may leave scars; thus, this method is contraindicated. The usual scenario involves a young, preschool-aged child with an enlarged cervical node that responds poorly to antibiotics. A tuberculin skin test often yields 5-9 mm of induration because atypical mycobacteria have antigens cross-reactive to those of tuberculosis. This amount of induration is considered indeterminate for tuberculosis in low-risk patients and suggests that the adenopathy is caused by an atypical mycobacterium. Skin tests with antigens from the various atypical mycobacteria are very sensitive and specific for infection; however, these antigens are not consistently available. Axial contrast-enhanced computed tomography image shows a cluster of enlarged nodes in the left neck containing low-attenuation necrotic centers (arrow). Gradual resolution of lymphadenitis sometimes occurs in children with atypical mycobacterial infections. Excisional biopsy is not necessary if the diagnosis is made presumptively from skin test results of less than 10-mm induration, if other infections are ruled out, if resolution occurs, and if the child is at low risk for infection with M. If the node does not improve, continues to enlarge, or spontaneously drains, excision is recommended and is usually curative. Fine-needle aspiration (for culture and acid-fast staining) may also be used, if the node is in an area where excision is impractical. Many other animals, including humans, can be incidentally and chronically infected hosts in which the parasite cannot complete its life cycle. Human acquisition of toxoplasmosis can result from contact with cat feces or soil that contains oocysts, which infect the host upon ingestion. Alternatively, the ingestion of raw or undercooked meat containing tissue cysts, particularly lamb or pork, may lead to infection. Adults in the United States are more likely to be infected from ingestion of raw meat than from contact with oocysts in cat feces or soil. Finally, infection can be transmitted to the fetus, especially when a pregnant woman is acutely infected with toxoplasmosis. Although many fetal infections are asymptomatic, transplacental infection with toxoplasmosis can result in severe neurologic damage, chorioretinitis, aseptic meningitis, and significant systemic illness manifesting with the classic triad of hepatosplenomegaly, intracranial calcifications, and hydrocephalus. The most common symptoms in children who acquire toxoplasmosis are lymphadenopathy, fever, malaise, myalgia, and pharyngitis. The most commonly affected nodes include the anterior and posterior cervical and axillary, which may be tender; involvement is usually bilateral. The lymph node enlargement seen in toxoplasmosis is caused by reticular hyperplasia and inflammation. In neonatal infections, tests measuring IgM have become more sensitive and specific. Antigen tests and cultures that grow the parasite are also available but primarily on an investigational level. Syphilis, caused by the spirochete Treponema pallidum, is common in the United States (see Chapter 18). The natural course of noncongenital syphilis includes 3 major clinical manifestations: · Primary syphilis, in which the individual develops a painless chancre at the site of inoculation · Secondary syphilis, in which the organism disseminates hematogenously to many organs · Tertiary syphilis, in which gummatous lesions develop in end organs, such as the brain, heart, and bones Lymphadenopathy can be seen as 1 of the manifestations of syphilis in several situations.
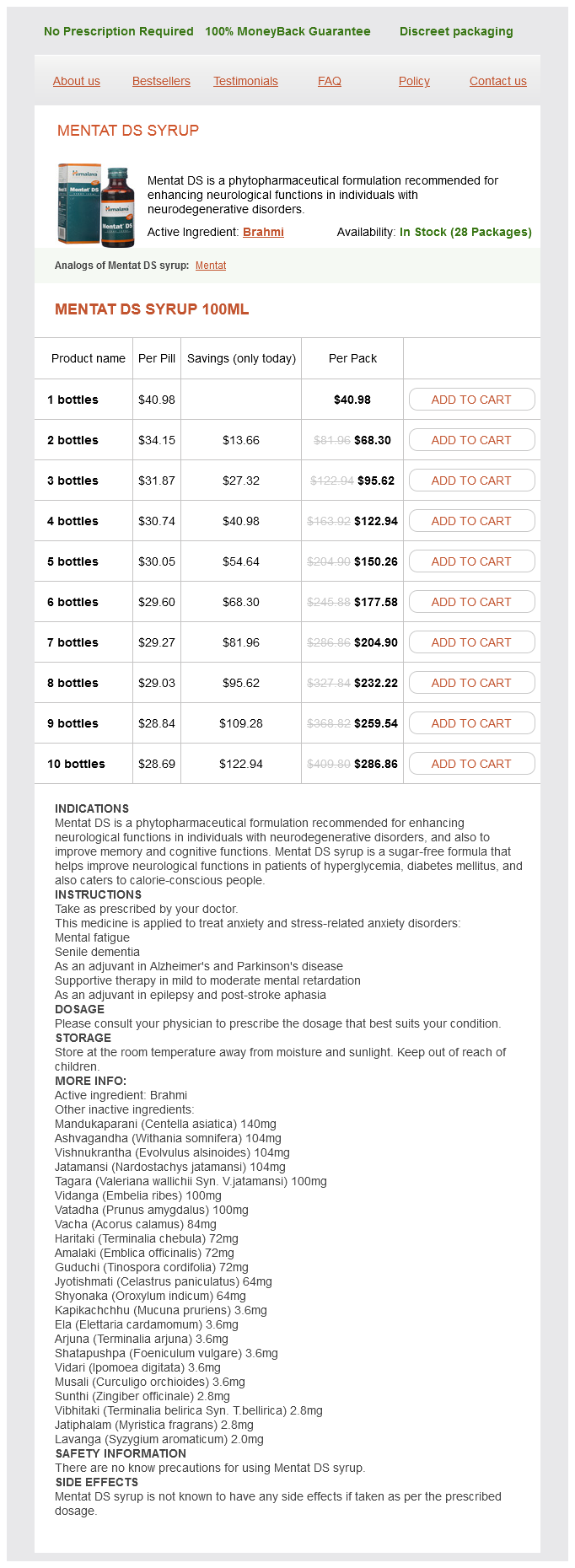
Mentat DS syrup Dosage and Price
Mentat DS syrup 100ml
- 1 bottles - $40.98
- 2 bottles - $68.30
- 3 bottles - $95.62
- 4 bottles - $122.94
- 5 bottles - $150.26
- 6 bottles - $177.58
- 7 bottles - $204.90
- 8 bottles - $232.22
- 9 bottles - $259.54
- 10 bottles - $286.86
Other congenital infections offer less opportunity for treatment to influence the outcome; extrarenal manifestations of these infections are much more serious than kidney disease medications medicaid covers cheap 100 ml mentat ds syrup otc. Primary renal disease causing nephrotic syndrome in early infancy is most often caused by either congenital nephrotic syndrome or diffuse mesangial sclerosis (Table 19. In both diseases, the prognosis for survival is poor unless aggressive supportive therapy and kidney transplantation are undertaken. Whether an evaluation should be performed depends on whether the proteinuria is both persistent and nonorthostatic. For a child younger than 7 or 8 years of age who has persistent proteinuria, normal total protein and serum albumin levels, normal complement, and no other signs of renal disease, there are two options. One option is to observe the patient carefully with repeated urinalyses every 3-6 months and to counsel the parents with regard to swelling and/or ascites, which may develop in association with influenza or an upper respiratory infection. If there is evidence of overt nephrotic syndrome with edema, a decrease in serum albumin and an increase in serum cholesterol, a trial of daily prednisone therapy is indicated. It is good practice to give the pneumococcal vaccine to patients who have persistent proteinuria but no evidence of edema or nephrotic syndrome, because of the risk of pneumococcal peritonitis if nephrotic syndrome develops. The other option involves instituting prednisone therapy to document that proteinuria has disappeared; this confirms the suspicion that the patient has steroid-responsive nephrotic syndrome. The rationale for withholding prednisone unless symptoms develop is that the natural history of minimal change disease is to remit; this may occur with or without prednisone administration. If the patient has a more serious lesion, symptoms will develop, at which time evaluation and therapy may be undertaken. In a patient older than 8 or 9 years, once the presence of persistent and nonorthostatic proteinuria is established, the next step is to quantify the amount of protein in a 24-hour specimen. If urinary protein excretion is greater than 8 mg/kg/day, a renal biopsy may be considered. Alternatively, these patients can also be treated with steroids and the response assessed. If proteinuria does not clear after 6-8 weeks of therapy, renal biopsy is then indicated. Hence, for an average 8-year-old patient who weighs 30 kg and is 1 m2 tall, proteinuria by these definitions is a level of 96 mg/day, and nephrotic syndrome is at a level of 960 mg/day. Renal biopsy can be considered at a Congenital Nephrotic Syndrome Congenital nephrotic syndrome is an autosomal recessive disorder resulting from mutations in the gene encoding the protein, nephrin (see Table 19. Infants with congenital nephrotic syndrome are often premature, with a low birthweight, placentomegaly, increased amniotic fluid -fetoprotein levels, and hypogammaglobinemia (decreased immunoglobulin G levels). Ascites and edema, caused by massive proteinuria, are usually present in affected infants during the first few weeks after birth. Infections and thrombosis are the two major complications; they cause considerable morbidity and mortality. Because of the massive proteinuria, patients fail to thrive; they require nasogastric feeding with a high-calorie, highprotein formula. Nephrectomy and peritoneal dialysis are often necessary to control protein losses and allow for adequate growth and control of uremia so that the infant can reach a size and nutritional state sufficient for renal transplantation. Proteinuria Both positive for protein Day/Night split 24-hr urine One negative Repeat ×2 (one in a. This has led to therapies that reduce proteinuria, thereby decreasing the risk of a progressive loss of renal function. The traffic of protein across the glomerular capillary membrane appears to stimulate a cascade of inflammatory events that cause interstitial fibrosis. This guideline helps avoid a biopsy for the patient with minimal proteinuria but does not require fullblown nephrotic syndrome to develop before a definitive work-up is initiated. However, the incidence of focal segmental sclerosis is much higher in adolescents than in younger children. Low molecular protein, such as 2-microblobulin, 1microglobulin, lysozyme, and retinol-binding protein can be seen in urine in tubular disorders, such as Fanconi syndrome or Dent disease. If associated with acidosis, hypokalemia, and hypophosphatemia, Fanconi syndrome should be considered. In males, if proteinuria is associated with hypercalciuria and nephrocalcinosis, Dent disease, an X-linked proximal tubulopathy that eventually leads to end-stage renal disease, should be considered, and the urine should be tested for 2microblobulin. Significant proteinuria with edema suggests nephrotic syndrome, which in most children suggests minimal change nephrotic syndrome. An age younger than 1 year or older than 10 years plus significant hematuria, azotemia, and hypertension are red flags that suggests a cause of nephrosis other than the more benign minimal change disease. Fever and abdominal pain in a patient with nephrotic syndrome should suggest spontaneous primary bacterial peritonitis. Changing patterns in the histopathology of idiopathic nephrotic syndrome in children. Plasmapheresis treatment for recurrent focal sclerosis in pediatric renal allografts. The prevalence of heavy proteinuria and progression risk factors in children undergoing urinary screening. Nephrotic syndrome in children: Prediction of histopathology from clinical and laboratory characteristics at time of diagnosis. Genetic causes of focal segmental glomerulosclerosis: implications for clinical practice.