General Information about Mectizan
Mectizan belongs to a class of drugs known as macrocyclic lactones, which work by paralyzing and killing the parasites, thus eliminating the an infection from the physique. It is a broad-spectrum drug, which means it can kill a broad range of parasites. This makes it a highly versatile and effective drug for treating numerous parasitic infections.
As with any medication, it is crucial to take Mectizan as prescribed and to complete the complete course of remedy. Skipping doses or stopping the therapy prematurely can result in the reoccurrence of the an infection, and in some instances, the development of drug-resistant parasites.
Mectizan is an FDA-approved drug and has been used safely in hundreds of thousands of people worldwide. However, it must be prevented in folks with certain medical conditions, together with liver or kidney disease, and people taking sure drugs like warfarin or rifampicin.
One of essentially the most important achievements of Mectizan is its position within the elimination of river blindness (onchocerciasis) in various countries in Africa and Latin America. This illness, caused by the parasitic worm Onchocerca volvulus, can lead to visible impairment and blindness. Mectizan has been widely utilized in mass drug administration applications to regulate the spread of this disease. It is given as a single dose every six to 12 months, and important progress has been seen within the reduction of circumstances of river blindness in endemic areas.
Although Mectizan is mostly well-tolerated, it might trigger some unwanted aspect effects in some individuals, together with nausea, vomiting, diarrhea, and complications. These unwanted effects are usually delicate and resolve on their own. However, it is essential to seek the advice of a physician if they persist or are extreme.
Mectizan, also recognized as Stromectol, is an anthelmintic drug used for the treatment of infections brought on by certain parasites. Mectizan has been proven to be extremely efficient in treating parasitic infections like river blindness, lymphatic filariasis, and scabies. Since its discovery within the Seventies, Mectizan has been utilized in various nations throughout the globe to combat the specter of parasitic illnesses.
In addition to those major achievements, Mectizan has also been used to treat different parasitic infections such as scabies, a skin condition attributable to the microscopic mite Sarcoptes scabiei. It is a highly contagious disease, often prevalent in overcrowded and unsanitary dwelling situations. Mectizan is an efficient therapy for scabies, because it kills the mite and its eggs, offering relief from the intense itching and pores and skin irritation.
Moreover, Mectizan has additionally been instrumental in controlling the spread of lymphatic filariasis, a parasitic illness transmitted by mosquito bites. This disease causes severe and infrequently irreversible swelling of limbs and genitalia, known as elephantiasis. In combination with one other drug, albendazole, Mectizan has been used in mass drug administration programs to cease the transmission of the disease. The success of this method has resulted in the World Health Organization (WHO) setting a goal to eliminate lymphatic filariasis by 2020.
In conclusion, Mectizan, also recognized as Stromectol, is a vital and extremely effective drug for the therapy of parasitic infections. Its success in controlling the spread of ailments like river blindness and lymphatic filariasis has been commendable. With continued efforts and the use of this drug in mass drug administration applications, it's potential to eradicate these parasitic ailments and improve the lives of millions of people all over the world. However, it is crucial that Mectizan is used responsibly and as prescribed to make sure its effectiveness and keep away from the event of drug-resistant parasites.
If present treatment for dogs flaky skin discount mectizan 3 mg online, the lens is displaced and Effects of Increased Intraocular Pressure Prolonged ocular hypertension has several effects on the eye: In adults, increased intraocular pressure leads to a characteristic cupped excavation of the optic nerve head (glaucomatous cupping), accompanied by a nasal displacement of the retinal blood vessels. The cornea or sclera bulges at weak points, such as sites of scars in the outer coat of the eye. It may arise from melanocytes in any part of the eye, the choroid being the most common site. Orange lipofuscin pigment is sometimes evident over the surface of some choroidal melanomas. Microscopically, uveal melanomas may be composed mainly of variable numbers of spindle-shaped cells without nucleoli (spindle A cells), spindle-shaped cells with prominent nucleoli (spindle B cells), polygonal cells with distinct cell borders and prominent nucleoli (epithelioid cells) or a fourth cell type that is similar to epithelioid cells but smaller with indistinct cell borders. Melanomas of the ciliary body and iris may extend circumferentially around the globe (ring melanoma). Melanomas in the iris are usually diagnosed clinically one to two decades earlier than those in the choroid and ciliary body, perhaps because they are more easily seen and are often first observed by the patient. Aside from hematogenous spread, uveal melanomas disseminate by traversing the sclera to enter the orbital tissues, usually at sites where blood vessels and nerves pass through the sclera. The liver is a common site of metastases, and anecdotally, the diagnosis of metastatic ocular melanoma can be made intuitively by astute clinicians who discover an enlarged liver in a patient with a "glass eye. Section through an eye with phthisis bulbi, exemplifying the markedly disorganized nature of the intraocular contents of such atrophic disordered globes. A typical finding in phthisis bulbi is intraocular bone formation, which may be derived from the hyperplastic pigment epithelium. Intraocular neoplasms arise mostly from immature retinal neurons (retinoblastoma) and uveal melanocytes (melanoma). Although the retinal pigment epithelium often undergoes reactive proliferation, it seldom becomes neoplastic. Unfavorable indicators are tumor hyperploidy, high mitotic activity, high microvascular density, high tumor-infiltrating lymphocyte counts, chromosome 3 monosomy and high serum melanoma inhibitory activity protein. Deaths have been reported within 5 years from spindle A melanomas, but tumors composed purely of epithelioid cells have the worst prognosis. Others extend between the sensory retina and the retinal pigment epithelium, thereby detaching the retina (exophytic retinoblastoma). Rarely, a retinoblastoma spreads diffusely within the retina without forming an obvious mass (diffuse retinoblastoma). The retina often contains several distinct foci of tumor in the same eye, some of which represent a multifocal origin, whereas others are tumor implants from dissemination through the vitreous body. Retinoblastoma is a cream-colored tumor that contains scattered, chalky white, calcified flecks within yellow necrotic zones. In other retinoblastomas, the cells are arranged radially around a central cavity (Flexner-Wintersteiner rosettes), as they differentiate toward photoreceptors. Viable tumor cells align themselves around blood vessels, and necrotic areas with calcification are seen a short distance from the vascularized regions. They also invade blood vessels, especially in the highly vascular choroid, before metastasizing Retinoblastomas Originate from Immature Neurons Retinoblastoma is the most common intraocular malignant neoplasm of childhood, affecting 1 in 20,000 to 1 in 34,000 children. It occurs most frequently within the first 2 years of life and may even be found at birth. Up to 25% of sporadic retinoblastomas and most inherited retinoblastomas are bilateral. Some patients with retinoblastoma have homologous genomic mutations in the Rb gene. Patients with inherited retinoblastomas, presumably as a consequence of the loss of Rb gene function, show increased susceptibility to other Metastatic Tumors to the Eye Are More Common Than Primary Ocular Neoplasms Sometimes an ocular metastasis may be the initial clinical manifestation of a cancer, but most cases are diagnosed only after death. Leukemias and cancers of the breast and lung usually metastasize to the posterior choroid and account for most cases of intraocular metastases. The orbit may be invaded by malignant neoplasms of the eyelid, conjunctiva, paranasal sinuses, nose, nasopharynx and intracranial cavity. Micozzi the Manner of Death Cause of Death versus Mechanism of Death Evidence Analyzed by the Forensic Pathologist Traumatic Injuries Sharp Force and Incised Wounds Blunt Force Trauma Death Occurring before a "Fatal" Accident Determination of Timing and Order of Receiving Wounds Asphyxiation Accident versus Homicide versus Suicide Cutting Motor Vehicles Gunshot Wounds Drug Overdose Hanging Poisonings Electrical Injury and Lightning Strikes Timing of Death Body Temperature Lividity Rigor Decomposition Disarticulation Forensic pathology is the specialty in which pathological examinations and related investigations are conducted for the purposes of classifying the cause and manner of death. A related goal is the establishment of the time since death, which may range from minutes to days to years. There are many observations of the deceased body that are made at the gross level and that cannot be documented by microscopic examination. Examples are the nature of traumatic injuries and the presence, location, size and extent of a pulmonary embolism. Whereas gross pathology is always part of the autopsy examination, the forensic pathologist may or may not pursue further microscopic examination, depending upon the nature of the case and the evidence. This chapter presents a summary of frequent problems in the practice of forensic pathology. Cause of Death versus Mechanism of Death Both resident and practicing physicians frequently complete a death certification incorrectly stating "cardiopulmonary" arrest as the cause of death. However, cardiopulmonary arrest is not a cause of death but a final common pathway whereby the underlying disease process finally leads to cessation of vital signs. Causes of true sudden death, whereby an otherwise healthy ambulatory person suddenly "drops dead in his tracks," are relatively few. A massive myocardial infarction brought about suddenly by coronary occlusion (see Chapter 7) may inactivate the conduction system and evoke an arrhythmia. Most of the cases that fall under medical examiner jurisdiction actually support areas beyond or outside public safety. A rule of thumb is that the rate of suicide is double the rate of homicide (except in excessively violent, crime-ridden jurisdictions). In most locations, about 1/2 of accidents relate to motor vehicle accidents and traffic fatalities, whereas the other 1/2 are industrial accidents and those in the home or in recreational settings. In terms of natural causes of death occurring outside the presence of a treating physician, these investigations are often important in identifying acute or chronic threats to public health, such as infectious disease outbreaks, contaminated water supplies, accidental poisonings or other toxic exposures.
In infants and children newest antibiotics for acne buy mectizan paypal, before cranial sutures have fused, the head enlarges sometimes to grotesque proportions as the ventricles dilate. As hydrocephalus is common in infants and treatable by shunting, measurement of the head circumference is a fundamental part of the pediatric physical examination. After sutures fuse, hydrocephalus cannot enlarge the head, but rather increases intracranial pressure. Remarkably, such individuals may retain substantial cognitive abilities, although spasticity may cloak the expression of this intelligence. Slow ventricular enlargement may appear clinically as progressive dementia, gait impairment and urinary incontinence as the long white matter fibers connecting portions of cortex to one another and lower motility centers are stretched apart by relentless expansion of the ventricles. This condition is usually accompanied by normal baseline intracranial pressure and so is called normal-pressure hydrocephalus, which may respond to shunting. This occurs most often in diffuse cortical atrophy, but focal destruction such as occurs at the site of an old infarct may lead to focal compensatory ventricular enlargement. However, evolutionary selection has not yet adequately responded to the need to survive motor vehicle crashes, personal assaults or dives into shallow pools. This energy transfer may directly disrupt tissues in penetrating injuries, or the energy may be translated into movement and compression of neural structures within the skull or spinal canal in a closed injury. Extreme injury of the brain and cord is possible with minimal disruption of overlying tissues. Conversely, superficial tissues can sustain dramatic injury while the nervous system underneath remains unaltered. Epidural Hematomas Are Often Fatal Epidural hematomas usually result from blows to the head with skull fracture. The intracranial dura is securely bound to the inner aspect of the calvaria and so is analogous to the intracranial periosteum. The middle meningeal arteries reside in grooves in the inner table of the bone between the dura and the calvaria, and their branches splay across the temporalparietal area. The temporal bone, being one of the thinnest bones of the skull, is particularly vulnerable to fracture. Populations at highest risk for such injuries include children, men in late adolescence and early adulthood and the elderly. This leads to a lensshaped accumulation of fresh blood that stops at the coronal suture lines. A discoid mass of fresh hemorrhage overlies the dura covering frontalparietal cortex but does not transgress the coronal sutures. Epidural hematomas are invariably progressive and, when not recognized and evacuated, may be fatal in 2448 hours. The blood and granulation tissue are surrounded by a sheet of fibrous connective tissue-the "membranes" of a chronic subdural hematoma. Fibroblasts first create a membrane on the calvarial side of the hematoma, the outer membrane. Then they invade the subjacent hematoma to form a fibrous membrane subjacent to the blood clot. It may (1) be reabsorbed and leave only a small amount of telltale hemosiderin; (2) remain static, and perhaps calcify; or (3) enlarge as a result of recurrent microhemorrhages in the granulation tissue. Expansion of the hematoma, and onset of symptoms, commonly results from rebleeding, usually within 6 months. Granulation tissue is fragile and so vulnerable to minor trauma, even that caused by shaking the head. Thus, subdural hematomas can rebleed and create a new hematoma subjacent to the outer membrane. Episodes of sporadic rebleeding expand these lesions periodically and at unpredictable intervals. In addition to granulation tissue and blood, other cellular constituents include plasma cells, lymphocytes and extramedullary hematopoiesis. These may contribute to the cellular dynamics of the subdural hematoma by releasing cytokines and causing cerebral edema in the underlying brain. Stretching of meninges leads to headaches; pressure on the motor cortex produces contralateral weakness; and focal cortical irritation can initiate seizures. Subdural hematomas are bilateral in 15%20% of cases, and these may impair cognitive function and lead to a mistaken diagnosis of dementia. Subdural Hematomas Develop More Slowly Than Epidural Hematomas Subdural hematomas are a significant cause of death after head injuries from falls, assaults, vehicular accidents and sporting accidents. The hematomas expand more slowly than epidural hematomas, so their clinical tempo is slower, but once critical increased intracranial pressure is attained, clinical deterioration and death can occur with horrific rapidity. Parenchymal Injuries Produce Variable Symptomatology Traumatic brain and spinal cord injuries range in severity from temporary loss of function with little or no discernible structural damage in concussion, to intermediate damage with hemorrhage and necrosis of the tissue in contusions, to profound disruption of structure and function in lacerations. Blood drains from cerebral hemispheres through veins that cross the subarachnoid space and arachnoid to breach the dura and enter the dural sinus. There is no true subdural space per se, but the inner layer of meningothelial cells of the dura has fewer tight junctions than those in the outer layers of the dura. Since bleeding in this situation is under low venous pressure, it is slow and may stop spontaneously from a local tamponade effect. The bleeding is within the dura itself and readily extends beyond the coronal sutures, causing a hematoma that can extend along the entire anterior to posterior dimensions of the calvarium. Granulation tissue forms in reaction to the blood, and the delicate capillaries of this tissue may themselves leak. This leads to gradual accumulation of an ever enlarging subacute, and ultimately chronic, subdural hematoma.
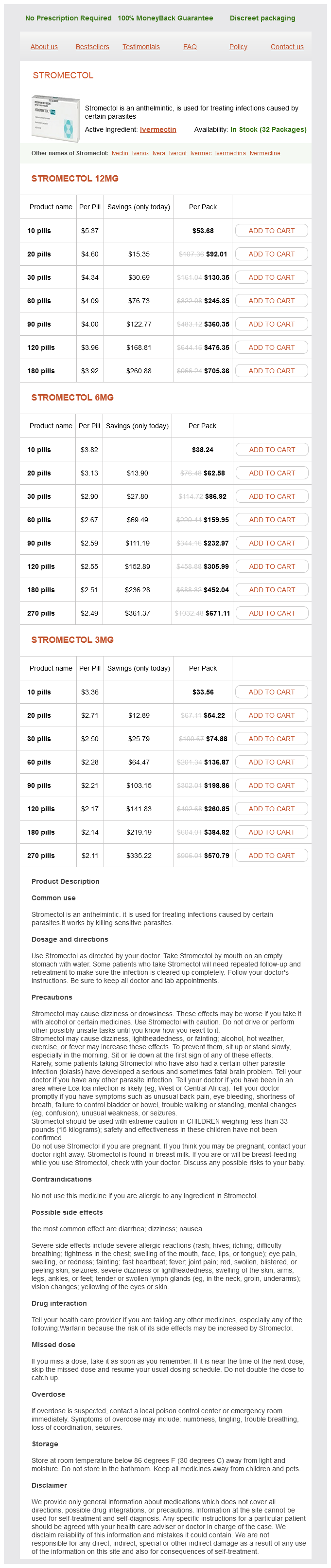
Mectizan Dosage and Price
Stromectol 12mg
- 10 pills - $53.68
- 20 pills - $92.01
- 30 pills - $130.35
- 60 pills - $245.35
- 90 pills - $360.35
- 120 pills - $475.35
- 180 pills - $705.36
Stromectol 6mg
- 10 pills - $38.24
- 20 pills - $62.58
- 30 pills - $86.92
- 60 pills - $159.95
- 90 pills - $232.97
- 120 pills - $305.99
- 180 pills - $452.04
- 270 pills - $671.11
Stromectol 3mg
- 10 pills - $33.56
- 20 pills - $54.22
- 30 pills - $74.88
- 60 pills - $136.87
- 90 pills - $198.86
- 120 pills - $260.85
- 180 pills - $384.82
- 270 pills - $570.79
Tumor may also be arranged in broad sweeping fascicles antibiotics no dairy discount mectizan 6 mg overnight delivery, resembling the "herringbone" pattern of fibrosarcoma. Some cells have a multinucleate appearance, although usually not as well formed as osteoclast-type giant cells. A secondary inflammatory infiltrate may accompany the tumor, either in association with areas of edema and necrosis or dispersed throughout the tumor. Very cellular samples often contain small fragments of loosely cohesive cell groups as well as single cells in the background. It may be more challenging to exclude the presence of some other type of high-grade neoplasm, particularly melanoma or sarcomatoid carcinoma. Judicious use of immunohistochemistry can be helpful in this case, with the caveat that faint or focal staining should not be accepted as proof of specific lineage differentiation. In addition, there is a "periostitis ossificans" that occurs on or in the periosteum of the bone, usually one of the long bones. Patients present with a rapidly growing and painful soft tissue mass in the digits; there may be redness and swelling as well. In those lacking history, the mechanism of formation is thought to be some type of subclinical, repetitive pattern of soft tissue injury. This occurs variably several weeks after the onset of symptoms, when dense calcifications begin to appear around the periphery of the injured soft tissue. Eventually the calcification coalesces to form an egg-shell type of rim around the lesion. Given time, the lesion will become completely ossified and may eventually be partially or completely resorbed. There may also be islands of immature-appearing cartilage that undergo ossification. The stroma may contain extravasated red blood cells, inflammatory cells, and osteoclastlike giant cells. Mitoses are usually numerous, but atypical mitotic figures should not be identified. The only difference is that the tumor of the digits tends to lack a clear-cut "zonation" pattern. Very immature lesions may closely resemble nodular fasciitis with an edematous stroma and entrapped skeletal muscle fibers. Fine needle biopsy or aspiration is much more likely to yield diagnostic material if either the calcified rim can be successfully penetrated (usually under image guidance) or the shell is thin and incomplete. Successful aspirates are most likely to be composed of the contents of the interior of the lesion and to resemble the cytologic features of nodular fasciitis. The background may have a granular or "dirty" texture with debris and inflammatory cells. Of note, degenerating muscle fibers can display extreme cytologic atypia and should not be overinterpreted as malignant or "sarcomatous" elements. In this example, degenerating skeletal muscle is present in a background of plump epithelioid and spindled cells. Lab results include hypophosphatemia, hyperphosphaturia, normocalcemia, and increased serum alkaline phosphatase. Because these lesions are sometimes very small, it is often necessary to "hunt" for them using radionucleotide scans. They do not tend to have any specific imaging features that are helpful in diagnosis. The latter have both aggressive histologic features as well as an aggressive clinical course with multiple recurrences. In addition, they can have variable amounts of intralesional matrix material, often in the form of irregular, "grungy," or flocculent calcifications. The soft tissue variant also frequently contains numerous osteoclast-type giant cells. There are several different mechanisms of disease formation, all involving an imbalance or defect in the calcium and/or phosphorus homeostasis metabolism. Tumor calcinosis can also occur secondary to other disease states, most commonly end-stage renal disease. Lesions developing as a secondary phenomenon are often termed "tumoral calcinosis-like" lesions. Tumoral calcinosis preferentially affects the large joints including the hips, shoulder, and elbows. It typically does not involve the joint space per se, but may involve the bursa and tendons. Symptoms are most often related to a mass effect, and there may be pain and limitation of joint movement. There is often secondary inflammation, and sinus tracts to the skin surface may form. Treatment of tumoral calcinosis is surgical if the lesion is idiopathic or primary. Secondary tumoral calcinosis responds best T to correction of the underlying associated disease process. This may include dietary restrictions or use of medical therapy to lower phosphate levels, dialysis, and renal transplantation.