General Information about Malegra FXT
Sildenafil citrate, generally generally known as the blue tablet, is a properly known and extremely effective medicine for treating ED. It works by enjoyable the muscles and increasing blood circulate to the penis, permitting for a stronger and longer-lasting erection. With the help of Sildenafil, males can obtain and preserve an erection, thus bettering their sexual performance.
Malegra FXT is easily available online and could be purchased and not utilizing a prescription. However, it's all the time greatest to seek the assistance of a well being care provider earlier than starting any new medication. It can additionally be important to comply with the really helpful dosage and take the treatment as directed. Overdosing on Malegra FXT can lead to severe complications and should be prevented at all costs.
In conclusion, Malegra FXT is a extremely efficient medication that gives a solution to both ED and PE. Its unique mixture of elements makes it a convenient and reliable possibility for males who battle with these sexual well being points. With its proven efficacy and safety, Malegra FXT has turn out to be a popular choice for men seeking a solution to their sexual struggles. It has helped numerous men regain their confidence and improve their sex lives, making it a highly really helpful medicine for these affected by ED and PE.
Fluoxetine, on the other hand, is an antidepressant medication that is known for its position within the treatment of PE. It works by increasing levels of serotonin in the mind, which helps to delay ejaculation and improve ejaculatory control. This makes Malegra FXT a unique medication that not only improves erectile function but in addition addresses the problem of premature ejaculation.
Erectile dysfunction (ED) and untimely ejaculation (PE) are widespread sexual health points that have an result on many men around the world. These situations not solely have physical repercussions but also take a toll on a person's self-esteem and confidence. Thankfully, there are medications available to assist combat these points and one such medicine is Malegra FXT.
As with any treatment, Malegra FXT does come with some potential side effects like complications, dizziness, and nausea. However, these unwanted side effects are generally delicate and may solely happen in a small percentage of customers. It is at all times recommended to seek the advice of a physician before taking any medicine, and the same applies to Malegra FXT. A physician can consider your medical history and decide if this medicine is secure for you.
The effectiveness of Malegra FXT has made it a well-liked choice for males suffering from both ED and PE. It has been clinically confirmed to be more practical than taking separate drugs for ED and PE, making it a handy and cost-effective alternative. It additionally eliminates the necessity to take a quantity of drugs, decreasing the chance of potential unwanted effects.
One of the primary advantages of Malegra FXT is that it starts to work in as little as half-hour, giving males the flexibleness to engage in sexual activity whenever they want. This is particularly helpful for many who have a busy way of life or suffer from performance anxiousness. Malegra FXT has a longer period of action compared to different ED drugs, permitting men to get pleasure from their sexual experiences with none time constraints.
Malegra FXT is a mix medication that has been particularly designed to tackle both ED and PE. It is a generic model of the popular medication, Viagra. The lively elements in Malegra FXT are Sildenafil citrate and Fluoxetine, which work collectively to offer efficient treatment for both problems.
A third subset of the endocrine system is represented by numerous cell types that express intracellular enzymes erectile dysfunction treatment prostate cancer malegra fxt 140 mg buy on-line, ectoenzymes, or secreted enzymes that modify inactive precursors or less active hormones into highly active hormones (see Table 38. Another example is activation of vitamin D by two subsequent hydroxylation reactions in the liver and kidneys to produce the highly bioactive hormone 1,25-dihydroxyvitamin D (vitamin D). Configuration of Feedback Loops Within the Endocrine System the predominant mode of a closed feedback loop among endocrine glands is negative feedback. In a negative feedback loop, a hormone acts on one or more target organs to induce a change (either a decrease or increase) in circulating levels of a specific component, and the change in this component then inhibits secretion of the hormone. A closed positive feedback loop, in which a hormone increases levels of a specific component and this component stimulates secretion of the hormone, confers instability. Under the control of positive feedback loops, something has got to give; for example, positive feedback loops control processes that lead to rupture of a follicle through the ovarian wall or expulsion of a fetus from the uterus. There are two basic configurations of negative feedback loops within the endocrine system: a physiological responsedriven feedback loop (referred to simply as a response-driven feedback loop) and an endocrine axisdriven feedback loop. The response-driven feedback loop is observed in endocrine glands that control blood glucose levels (pancreatic islet cells), blood Ca++ and Pi levels (parathyroid glands, kidneys), blood osmolarity and volume (hypothalamus/posterior pituitary gland), and blood Na+, K+, and H+ levels (zona glomerulosa of the adrenal cortex and atrial cells). In the response-driven configuration, secretion of a hormone is stimulated or inhibited by a change in the level of a specific extracellular parameter. Alterations in hormone levels lead to changes in the physiological characteristics of target organs. The change in the parameter (decreased blood glucose level) then inhibits further secretion of the hormone. Much of the endocrine system is organized into endocrine axes; each axis consists of the hypothalamus, the pituitary gland, and the peripheral endocrine glands. Thus the endocrine axisdriven feedback loop involves a three-tiered configuration. The first tier is represented by hypothalamic neuroendocrine neurons that secrete releasing hormones. Releasing hormones stimulate (or, in a few cases, inhibit) the production and secretion of tropic hormones from the pituitary gland (second tier). Tropic hormones stimulate the production and secretion of hormones from peripheral endocrine glands (third tier). However, in endocrine axisdriven feedback, the primary feedback loop involves feedback inhibition of pituitary tropic hormones and hypothalamic releasing hormones by the peripherally produced hormone. In contrast to response-driven feedback, the physiological responses to the peripherally produced hormone play only a minor role in regulation of feedback within endocrine axisdriven feedback loops. From a clinical perspective, endocrine diseases are described as primary, secondary, or tertiary diseases. Primary disease is a lesion in the peripheral endocrine gland; secondary disease is a lesion in the anterior pituitary gland; and tertiary disease is a lesion in the hypothalamus. An important aspect of the endocrine axes is the ability of descending and ascending neuronal signals to modulate release of the hypothalamic releasing hormones and thereby control the activity of the axis. This tiny gland, close to the hypothalamus, synthesizes the hormone melatonin from the neurotransmitter serotonin, of which tryptophan is the precursor. The amount and activity of this enzyme in the pineal gland vary markedly in a cyclic manner, which accounts for the cycling of melatonin secretion and its plasma levels. Thus melatonin may transmit the information that nighttime has arrived, and body functions are regulated accordingly. Another important input to hypothalamic neurons and the pituitary gland is stress, either as systemic stress. Major medical or surgical stress overrides the circadian clock and causes a pattern of persistent and exaggerated hormone release and metabolism that mobilizes endogenous fuels, such as glucose and free fatty acids, and augments their delivery to critical organs. In addition, cytokines released during inflammatory or immune responses, or both, directly regulate the release of hypothalamic releasing hormones and pituitary hormones. Chemical Nature of Hormones Hormones are classified biochemically as proteins/peptides, catecholamines, steroid hormones, or iodothyronines. The chemical nature of a hormone determines (1) how it is synthesized, stored, and released; (2) how it is transported in blood; (3) its biological half-life and mode of clearance; and (4) its cellular mechanism of action. Proteins/Peptides Protein and peptide hormones can be grouped into structurally related molecules that are encoded by gene families. Protein/peptide hormones obtain their specificity from their primary amino acid sequence and from posttranslational modifications, especially glycosylation. Because protein/peptide hormones are destined for secretion outside the cell, their synthesis and processing are differently from those of proteins destined to remain within the cell or to be continuously added to the membrane. These hormones are synthesized on the polyribosome as larger preprohormones or prehormones. The nascent peptides have at their N-terminus a group of 15 to 30 amino acids called the signal peptide. The nighttime rise in plasma melatonin may mediate certain other circadian patterns. Removal of the signal peptide by a signal peptidase generates a hormone or prohormone, which is then transported from the cisternae of the endoplasmic reticulum to the Golgi apparatus, where it is packaged into a membrane-bound secretory vesicle that is subsequently released into the cytoplasm. Prohormones harbor the peptide sequence of the active hormone within their primary sequence. However, prohormones are inactive or less active and require the action of endopeptidases to trim away the neighboring inactive sequences. Protein/peptide hormones are stored in the gland as membrane-bound secretory vesicles and are released by exocytosis through the regulated secretory pathway. Rather, they are secreted in response to a stimulus through a mechanism of stimulus-secretion coupling.
For example impotence after prostatectomy buy cheap malegra fxt 140 mg online, in the capillary sinusoids of the liver, endothelial cells are often separated by large gaps (discontinuous capillary). As a result, water and all components of the plasma (and some cellular elements) can pass easily across the wall. Other capillaries are lined by endothelial cells that contain fenestrations that are up to 80 to 100 nm in diameter. These fenestrations allow all components of the plasma (only cellular elements of blood cannot pass through the fenestrations) to move across the capillary wall. In addition, a small amount of water traverses the capillary wall via pinocytosis by endothelial cells. The driving forces for fluid (water) movement across the capillary wall are hydrostatic pressure and oncotic pressure. Capillary fluid movement is discussed in detail in Chapter 17; in brief, hydrostatic pressure within the capillary (as a result of the pumping of the heart and the effect of gravity on the column of blood in the vessels feeding a capillary) is a force that causes fluid to move out of the capillary. Hydrostatic pressure in the surrounding interstitial tissue opposes the effect of the capillary hydrostatic pressure. The oncotic pressure of the plasma in the capillary tends to draw fluid from the interstitium into the capillary. Thus the amount of fluid moving across the wall of the capillary is determined as follows: Equation 2. Depending on the magnitude of these forces, fluid may move out of the capillary or into the capillary. The compositions of the various body fluid compartments differ; however, as described later, the osmolalities of the fluid within these compartments are essentially identical. Because of this rapid redistribution of water, measuring the osmolality of plasma or serum,c which is easy to do, reveals the osmolality of the other body fluid compartments. For example, if a blood sample is obtained from an individual, and the [Na+] of the serum is 145 mEq/L, its osmolality can be estimated as follows: Equation 2. Consequently, in trying to understand the physiology of fluid shifts between body fluid compartments, it can be assumed that while water moves freely between the compartments, there is little net movement of solutes. With regard to osmolality and the concentrations of other molecules and ions, the osmolality and concentrations in plasma and serum are virtually identical. When electrolyte solutions are infused by this route, equilibration between plasma and interstitial fluid is rapid. Accordingly,serumosmolalitycanbeestimated asfollows: Serum osmolality = 2(serum [Na +]) + [glucose] [urea] + 18 2. Therefore, there is no net movement of the infused isotonic NaCl solution into cells. The major difference between the interstitial fluid and plasma is that the latter contains significantly more protein. This section is a review of the mechanisms by which cells maintain their intracellular ionic environment and their membrane potential and by which they control their volume. Ionic Composition of Cells the intracellular ionic composition of cells varies from tissue to tissue. For example, the intracellular composition of neurons is different from that of muscle cells, both of which differ from that of blood cells. For example, as described in Chapter 1, a number of solute carriers couple the transport of Na+ to that of other ions or molecules. The Na+-glucose and Na+amino acid symporters use the energy in the Na+ electrochemical gradient, directed to bring Na+ distribution of cations and anions between these two compartments by the Gibbs-Donnan effect (see the section "Isotonic Cell Volume Regulation" for details), this effect is small, and the ionic compositions of the interstitial fluid and plasma can be considered to be identical. For example, the activity of some enzymes is pH dependent; therefore, intracellular pH must be regulated. In addition, the intracellular composition of other electrolytes is similarly held within a narrow range. This is necessary for the establishment of the membrane potential, a cell property especially important for the normal function of excitable cells. Finally, the volume of cells must be maintained because shrinking or swelling of cells can lead to cell damage or death. Similarly, the inwardly directed Na+ gradient drives the secondary active extrusion of H+ from the cell and thus contributes to the maintenance of intracellular pH. As might be expected, the contribution of various electrogenic transporters to the Vm is highly variable from cell to cell. Similarly, the contribution of other electrogenic transporters, such as the 3Na+-Ca++ antiporter and the Na+-glucose symporter is minimal. As described in Chapter 5, rapid changes in ion channel activity underlies the action potential in neurons and other excitable cells, such as those of skeletal and cardiac muscle (see Chapters 12 and 13). As described in Chapter 1, this current can be measured, even at the level of a single channel. By convention, the current generated by the movement of cations into the cell, or the movement of anions out of the cell, is defined as negative current. Conversely, the movement of cations out of the cell, or the movement of anions into the cell, is defined as positive current. Also by convention, the magnitude of the Vm is expressed in relation to the outside of the cell; thus for a cell with a Vm of -80 mV, the interior of the cell is electrically negative in relation to the outside of the cell. The current carried by ions moving through a channel depends on the driving force for that ion and on the conductance of the channel. As described in Chapter 1, the driving force is determined by the energy in the concentration gradient for the ion across the membrane (Ei), as calculated by the Nernst equation (Eq. For a cell, the conductance of the membrane to a particular ion (Gi) is determined by the number of ion channels in the membrane and by the amount of time each channel is in the open state.
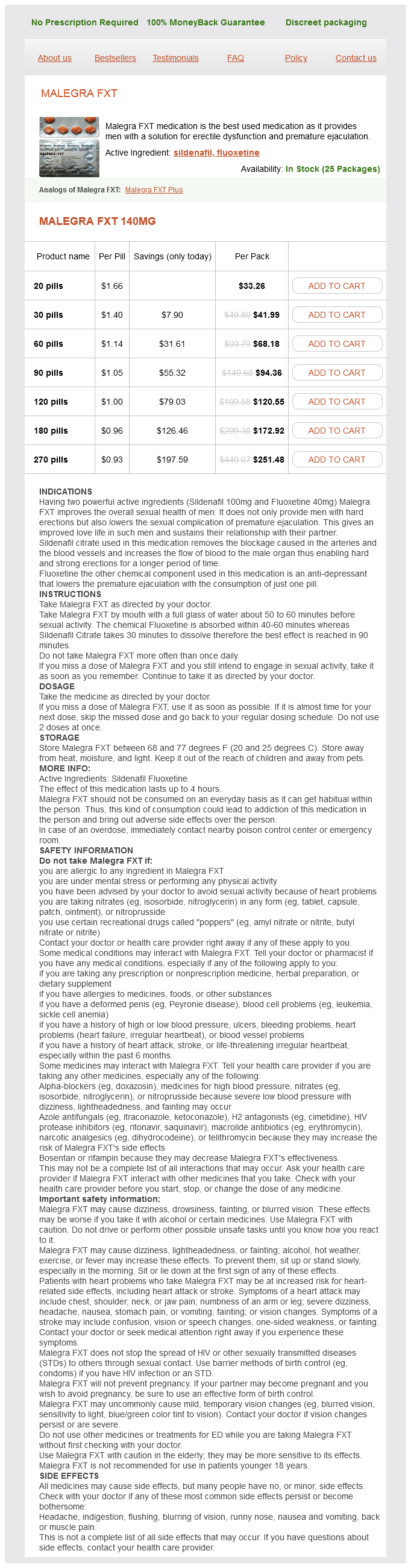
Malegra FXT Dosage and Price
Malegra FXT 140mg
- 20 pills - $33.26
- 30 pills - $41.99
- 60 pills - $68.18
- 90 pills - $94.36
- 120 pills - $120.55
- 180 pills - $172.92
- 270 pills - $251.48
Only cartilage impotence at 80 generic malegra fxt 140 mg fast delivery, bone, epithelia, and tissues of the central nervous system lack lymphatic vessels. This task is accomplished by means of tissue pressure, and it is facilitated by intermittent skeletal muscle activity, lymphatic vessel contractions, and an extensive system of one-way valves. In this regard, lymphatic vessels resemble veins, although the larger lymphatic vessels do have thinner walls than do the corresponding veins, and they contain only a small amount of elastic tissue and smooth muscle. The lymphatic vessels return all of the proteins filtered back to the blood; these proteins account for approximately one fourth to half of the circulating plasma proteins in the blood. The lymphatic vessels are the only means by which the protein that leaves the vascular compartment can be returned to blood. Net backward diffusion of protein into the capillaries cannot occur against the large protein concentration gradient. If the protein were not removed by the lymph vessels, it would accumulate in interstitial fluid and act as an oncotic force that draws fluid from the blood capillaries and produces edema. In addition to returning fluid and protein to the vascular bed, the lymphatic system filters the lymph at the lymph nodes and removes foreign particles such as bacteria. The Coronary Circulation Functional Anatomy of Coronary Vessels the right and left coronary arteries arise at the root of the aorta behind the right and left cusps of the aortic valve, respectively. The left coronary artery, which divides near its origin into the anterior descending and the circumflex branches, supplies mainly the left ventricle and atrium. There is some overlap between the regions supplied by the left and right arteries. In humans, the right coronary artery is dominant (supplying most of the myocardium) in approximately 50% of individuals. The left coronary artery is dominant in another 20%, and the flow delivered by each main artery is approximately equal in the remaining 30%. Coronary arterial blood passes through the capillary beds; most of it returns to the right atrium through the coronary sinus. Of the coronary arteries, epicardial arteries are largest (2 to 5 mm in diameter), large arterioles are medium in size (1. Some of the coronary venous blood reaches the right atrium via the anterior coronary veins. In addition, vascular communications directly link the myocardial vessels with the cardiac chambers; these communications are the arteriosinusoidal, arterioluminal, and thebesian vessels. The arteriosinusoidal channels consist of small arteries or arterioles that lose their arterial structure as they penetrate the chamber walls, where they divide into irregular, endothelium-lined sinuses. These sinuses anastomose with other sinuses and with capillaries, and they communicate with the cardiac chambers. The arterioluminal vessels are small arteries or arterioles that open directly into the atria and ventricles. The thebesian vessels are small veins that connect capillary beds directly with the cardiac chambers and also communicate with the cardiac veins. However, the myocardium does not receive significant nutritional blood flow directly from the cardiac chambers. Factors That Influence Coronary Blood Flow Physical Factors the primary factor responsible for perfusion of the myocardium is aortic pressure. Changes in aortic pressure generally evoke parallel directional changes in coronary blood flow. However, the major factor in the regulation of coronary blood flow is a change in arteriolar resistance engendered by changes in the metabolic activity of the heart. When the metabolic activity of the heart increases, coronary resistance decreases; when cardiac metabolism decreases, coronary resistance increases (see Chapter 18). If a cannulated coronary artery is perfused by blood from a pressurecontrolled reservoir, perfusion pressure can be altered without a change in aortic pressure and cardiac work. The relationship between initial and steady-state blood flow is shown in the experiment depicted in. This is an example of autoregulation of blood flow, which is mediated by a myogenic mechanism in large and small arterioles (Chapter 18). The metabolic activity of cardiac muscle in small arterioles and the endothelium modulate autoregulation. The coronary circulation adjusts serial resistances within the microvasculature thereby adapting blood flow to O2 requirements. Hence, changes in coronary blood flow are caused mainly by changes in the diameter of coronary resistance vessels in response to the metabolic demands of the heart. In addition to providing the pressure to move blood through the coronary vessels, the heart also affects its blood supply by the squeezing effect (extravascular compression) of the contracting myocardium on its own blood vessels. In the left ventricle, coronary perfusion pressure is the difference between aortic diastolic pressure and left ventricular end-diastolic pressure. Left ventricular myocardial pressure (pressure within the wall of the left ventricle) is highest near the endocardium and lowest near the epicardium. This pressure gradient does not normally impair endocardial blood flow because the greater blood flow to the endocardium during diastole compensates for the greater blood flow to the epicardium during systole. Measurements of coronary blood flow indicate that the epicardial and endocardial halves of the left ventricle receive approximately equal blood flow under normal conditions. Because extravascular compression is greatest at the endocardial surface of the ventricle, the equality of epicardial and endocardial blood flow indicates that the tone of the endocardial resistance vessels is less than that of the epicardial vessels. The flow pattern in the right coronary artery is similar to that in the left coronary artery.