General Information about Malegra DXT
Malegra DXT comes in a tablet kind with strengths ranging from 30 mg to one hundred twenty mg. The really helpful dose is one pill per day, taken orally with water about 30 minutes earlier than sexual activity. It is essential to comply with the prescribed dosage and not to exceed it to minimize the risk of side effects.
Combining these two components in Malegra DXT creates a robust dual-action formula that targets each ED and PE. It works by enhancing blood flow to the penis, leading to a firmer and longer-lasting erection, whereas also delaying ejaculation and giving males extra control over their sexual response. This makes Malegra DXT a convenient and environment friendly resolution for those dealing with both situations.
Fortunately, there are treatments obtainable for these situations, and one of them is Malegra DXT. This medicine is a combination of two powerful components – Sildenafil and Duloxetine – that work collectively to improve sexual performance and enhance satisfaction in males.
Sildenafil is a widely known and efficient remedy for erectile dysfunction. It belongs to a category of medication known as phosphodiesterase type 5 (PDE-5) inhibitors, which work by growing blood circulate to the penis, leading to a agency and lasting erection. Sildenafil is the energetic ingredient within the well-liked medication Viagra, and it has been proven to help males with ED achieve and preserve an erection.
On the opposite hand, Duloxetine is a selective serotonin and norepinephrine reuptake inhibitor (SSNRI) that's primarily used to treat depression and anxiety. Unlike Sildenafil, it does not immediately affect erectile operate. However, it has been found to delay ejaculation by affecting certain chemicals in the brain that management sexual response. This might help men who expertise rapid ejaculation to have higher control over their climax and last longer throughout sexual exercise.
In conclusion, Malegra DXT is a protected and effective treatment for men coping with each erectile dysfunction and untimely ejaculation. Its dual-action formula makes it a convenient and efficient answer for these trying to enhance their sexual efficiency and satisfaction. However, as with every medicine, it is crucial to consult a well being care provider before beginning a remedy plan, and to comply with the prescribed dosage to minimize the chance of unwanted effects. With Malegra DXT, men can experience a more fulfilling and pleasant sexual expertise.
It can be important to note that Malegra DXT should not be taken with sure medicines, including nitrates, alpha-blockers, and blood pressure-lowering medication. These can work together with the components in Malegra DXT and trigger potentially harmful side effects. Therefore, it's advisable to inform a health care provider about any other medicines that you are taking to avoid any complications.
Like any medication, Malegra DXT may have some unwanted effects, including nausea, dizziness, headache, flushing, and indigestion. These unwanted effects are usually delicate and short-term, and they need to subside as the medicine wears off. However, in the occasion that they persist or become severe, it's best to seek the assistance of a physician.
This dual-action formula presents a handy and effective answer for those suffering from each of those circumstances.
Erectile dysfunction (ED) and untimely ejaculation (PE) are two of the most typical sexual well being issues affecting men. ED refers again to the incapability to achieve or preserve an erection, while PE refers to the lack of ability to control ejaculation and reach satisfaction during sexual intercourse. Both conditions can lead to frustration, anxiety, and pressure in relationships.
However erectile dysfunction recovery time order 130 mg malegra dxt free shipping, long-term oral treatment is poorly tolerated and often is stopped owing to adverse effects. Propafenone Propafenone is a Na+ channel blocker with a relatively slow time constant for recovery from block (Funck-Brentano et al. Its major electrophysiological effect is to slow conduction in fast-response tissues. The drug is prescribed as a racemate; while the enantiomers do not differ in their Na+ channelblocking properties, S-(+)-propafenone is a adrenergic receptor antagonist in vitro and in some patients. Chronic therapy with oral propafenone is used to maintain sinus rhythm in patients with supraventricular tachycardias, including atrial fibrillation; like other Na+ channel blockers, it also can be used in ventricular arrhythmias, but with only modest efficacy. Pharmacological Effects Procainamide is a blocker of open Na+ channels with an intermediate recovery from block. It also prolongs cardiac action potentials in most tissues, probably by blocking outward K+ current(s). Procainamide decreases automaticity, increases refractory periods, and slows conduction. The major metabolite, N-acetyl procainamide, lacks the Na+ channelblocking activity of the parent drug but is equipotent in prolonging action potentials. Although hypotension may occur at high plasma concentrations, this effect usually is attributable to ganglionic blockade rather than to any negative inotropic effect, which is minimal. Adverse Effects Adverse Effects Hypotension and marked slowing of conduction are major adverse effects of high concentrations (>10 g/mL) of procainamide, especially during intravenous use. Dose-related nausea is frequent during oral therapy and may be attributable in part to high plasma concentrations of N-acetyl procainamide. Torsades de pointes can occur, particularly when plasma concentrations of N-acetyl procainamide rise to greater than 30 g/mL. During long-term therapy, most patients will develop biochemical evidence of the drug-induced lupus syndrome, such as circulating antinuclear antibodies. Therapy need not be interrupted merely because of the presence of antinuclear antibodies. However, 25%50% of patients eventually develop symptoms of the lupus syndrome; common early symptoms are rash and small-joint arthralgias. Other symptoms of lupus, including pericarditis with tamponade, can occur, although renal involvement is unusual. The lupus-like symptoms resolve on cessation of therapy Adverse effects during propafenone therapy include acceleration of ventricular response in patients with atrial flutter, increased frequency or severity of episodes of reentrant ventricular tachycardia, exacerbation of heart failure, and the adverse effects of adrenergic blockade, such as sinus bradycardia and bronchospasm (see previous discussion and Chapter 12). In most subjects ("extensive metabolizers"), propafenone undergoes extensive first-pass hepatic metabolism to 5-hydroxy propafenone, a metabolite equipotent to propafenone as a Na+ channel blocker but much less potent as a adrenergic receptor antagonist. The incidence of adverse effects during propafenone therapy is significantly higher in poor metabolizers. In extensive metabolizer subjects receiving such drugs or in poor metabolizer subjects, plasma propafenone concentrations of more than 1 g/mL are associated with clinical effects of adrenergic receptor blockade, such as reduction of exercise heart rate. It is recommended that dosage in patients with moderate-to-severe liver disease should be reduced to approximately 20%30% of the usual dose, with careful monitoring. It is not known if propafenone doses must be decreased in patients with renal disease. The most common is thrombocytopenia, which can be severe but which resolves rapidly with discontinuation of the drug. Quinidine also can produce cinchonism, a syndrome that includes headache and tinnitus. In contrast to other adverse responses to quinidine therapy, cinchonism usually is related to elevated plasma quinidine concentrations and can be managed by dose reduction. In contrast to effects of sotalol, N-acetyl procainamide, and many other drugs, quinidine-associated torsades de pointes generally occurs at therapeutic or even subtherapeutic plasma concentrations. At high plasma concentrations of quinidine, marked Na+ channel block can occur, with resulting ventricular tachycardia. This adverse effect occurs when very high doses of quinidine are used to try to convert atrial fibrillation to normal rhythm; this aggressive approach to quinidine dosing has been abandoned, and quinidine-induced ventricular tachycardia is unusual. However, in most patients with congestive heart failure, quinidine is well tolerated, perhaps because of its vasodilating actions. Studies in the early 20th century identified quinidine, a diastereomer of the antimalarial quinine, as the most potent of the antiarrhythmic substances extracted from the cinchona plant, and by the 1920s, quinidine was used as an antiarrhythmic agent. As a consequence of its K+ channelblocking actions, quinidine prolongs action potentials in most cardiac cells, most prominently at slow heart rates. Quinidine prolongs refractoriness in most tissues, probably as a result of both prolongation of action potential duration and Na+ channel blockade. In intact animals and humans, quinidine also produces adrenergic receptor blockade and vagal inhibition. Thus, the intravenous use of quinidine is associated with marked hypotension and sinus tachycardia. Quinidine is well absorbed and is 80% bound to plasma proteins, including albumin and, like lidocaine, the acute-phase reactant 1-acid glycoprotein. As with lidocaine, greater-than-usual doses (and total plasma quinidine concentrations) may be required to maintain therapeutic concentrations of free quinidine in high-stress states such as acute myocardial infarction. Quinidine undergoes extensive hepatic oxidative metabolism, and approximately 20% is excreted unchanged by the kidneys. One metabolite, 3-hydroxyquinidine, is nearly as potent as quinidine in blocking cardiac Na+ channels and prolonging cardiac action potentials.
The indications for parenteral iron therapy include documented iron deficiency and intolerance or irresponsiveness to oral iron drugs for erectile dysfunction ppt buy malegra dxt 130 mg online. The rate of hemoglobin response is determined by the balance between the severity of the anemia (the level of erythropoietin stimulus) and the delivery of iron to the marrow from iron absorption and iron stores. When a large intravenous dose of iron dextran is given to a severely anemic patient, the hematologic response can exceed that seen with oral iron for 13 weeks. Parenteral iron therapy should be used only when clearly indicated because acute hypersensitivity, including anaphylactic and anaphylactoid reactions, can occur. Other reactions to intravenous iron include headache, malaise, fever, generalized lymphadenopathy, arthralgias, urticaria, and, in some patients with rheumatoid arthritis, exacerbation of the disease. These include iron dextran, sodium ferric gluconate, ferumoxytol, iron sucrose, and ferric carboxymaltose. Ferumoxytol is a semisynthetic carbohydrate-coated superparamagnetic iron oxide nanoparticle approved for treatment of iron deficiency anemia in patients with chronic kidney disease; the ferumoxytol has to be administered safely as a 1. Indications for ferric gluconate and iron sucrose are limited to patients with chronic kidney disease and documented iron deficiency, although broader applications are being advocated (Larson and Coyne, 2014). Iron dextran can be administered by intravenous (preferred) or intramuscular injection. Given intravenously in a dose less than 500 mg, the iron dextran complex is cleared with a plasma t1/2 of 6 h. When 1 g or more is administered intravenously as total-dose therapy, reticuloendothelial cell clearance is constant at 1020 mg/h. Intramuscular injection of iron dextran should be initiated only after a test dose of 0. However, local reactions and the concern about malignant change at the site of injection make intramuscular administration inappropriate except when the intravenous route is inaccessible. The patient should be observed for signs of immediate anaphylaxis and for an hour after injection for any signs of vascular instability or hypersensitivity, including respiratory distress, hypotension, tachycardia, or back or chest pain. Delayed hypersensitivity reactions also are observed, especially in patients with rheumatoid arthritis or a history of allergies. Fever, malaise, lymphadenopathy, arthralgias, and urticaria can develop days or weeks following injection and last for prolonged periods of time. Use iron dextran with extreme caution in patients with rheumatoid arthritis or other connective tissue diseases and during the acute phase of an inflammatory illness. It seems prudent, however, to withhold the drug whenever the plasma ferritin rises above 800 g/L. Sodium ferric gluconate is an intravenous iron preparation with a molecular size of about 295 kDa and an osmolality of 990 mOsm/kg-1. Unlike iron dextran, which requires processing by macrophages that may require several weeks, about 80% of sodium ferric gluconate is delivered to transferrin within 24 h. Sodium ferric gluconate also has a lower risk of inducing serious anaphylactic reactions than iron dextran (Sengolge et al. Following intravenous injection, the complex is taken up by the reticuloendothelial system, where it dissociates into iron and sucrose. Iron sucrose is generally administered in daily amounts of 100200 mg within a 14-day period to a total cumulative dose of 1000 mg. Like sodium ferric gluconate, iron sucrose appears to be better tolerated and to cause fewer adverse events than iron dextran (Hayat, 2008). Chronic use has the potential to cause renal tubulointerstitial damage (Agarwal, 2006). Iron dextran injection is a colloidal solution of ferric oxyhydroxide complexed with polymerized dextran (molecular weight 180,000 Da) that contains 50 mg/mL of elemental iron. The use of sisting of a ferric hydroxide core and a carbohydrate shell (Keating, 2015). With this preparation, a replenishment dose of up to 1000 mg of iron can be administered in 15 min. Intravenous administration results in transient elevations in serum iron, serum ferritin, and transferrin saturation, with subsequent correction in hemoglobin levels and replenishment of depleted iron stores. Ferric carboxymaltose is rapidly cleared from the circulation, becoming distributed (~80%) in the marrow, as well as the liver and spleen. Common reported drug-related adverse effects include headache, dizziness, nausea, abdominal pain, constipation, diarrhea, rash, and injection site reactions. However, the incidence of drug-related adverse events appears similar to those of patients treated with oral ferrous sulfate. Copper, Pyridoxine, and Riboflavin Copper Copper has redox properties similar to those of iron, which simultaneously are essential and potentially toxic to the cell. Instead, copper is stored by metallothioneins and distributed by specialized chaperones to sites that make use of its redox properties. In mammals, the liver is the organ most responsible for the storage, distribution, and excretion of copper. Copper deficiency is extremely rare; the amount present in food is more than adequate to provide the needed body complement of slightly more than 100 mg. Even in clinical states associated with hypocupremia (sprue, celiac disease, and nephrotic syndrome), effects of copper deficiency usually are not demonstrable. Anemia due to copper deficiency has been described in individuals who have undergone intestinal bypass surgery, in those who are receiving parenteral nutrition, in malnourished infants, and in patients ingesting excessive amounts of zinc (Willis et al.
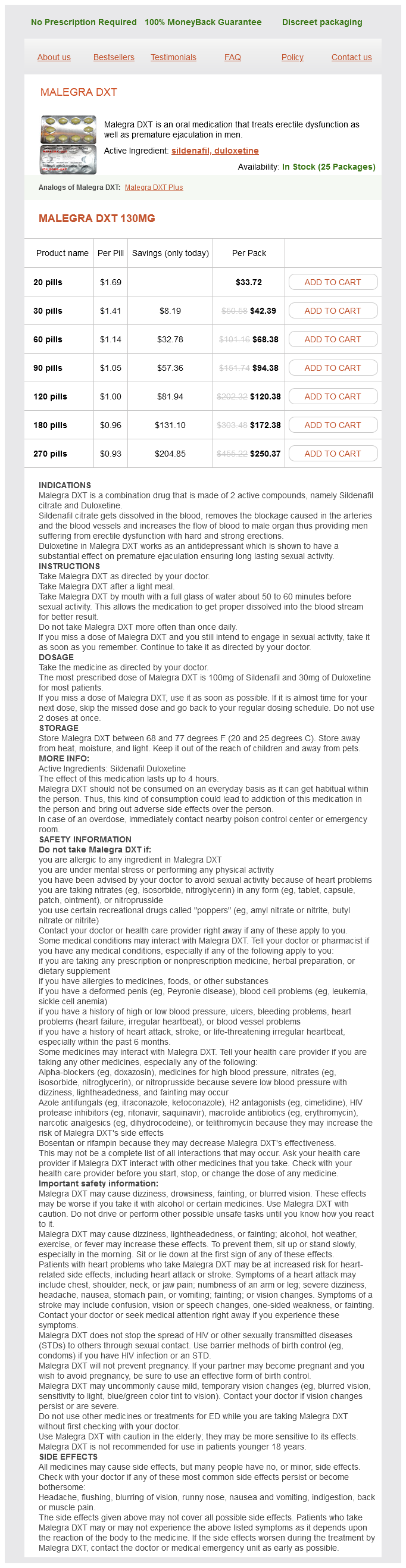
Malegra DXT Dosage and Price
Malegra DXT 130mg
- 20 pills - $33.72
- 30 pills - $42.39
- 60 pills - $68.38
- 90 pills - $94.38
- 120 pills - $120.38
- 180 pills - $172.38
- 270 pills - $250.37
Many of these agents act by decreasing intestinal motility and should be avoided in acute diarrheal illnesses caused by invasive organisms erectile dysfunction treatment homeveda buy malegra dxt australia. In such cases, these agents may mask the clinical picture, delay clearance of organisms, and increase the risk of systemic invasion by the infectious organisms. In the low pH of the stomach, the bismuth subsalicylate reacts with hydrochloric acid to form bismuth oxychloride and salicylic acid. Bismuth is thought to have antisecretory, anti-inflammatory, and antimicrobial effects. The clay in bismuth subsalicylate and generic formulations may have some additional benefits in diarrhea, but this is not clear. A recommended dose of the bismuth subsalicylate (30 mL of regular-strength liquid or 2 tablets) contains approximately equal amounts of bismuth and salicylate (262 mg each). For control of indigestion, nausea, or diarrhea, the dose is repeated every 3060 min, as needed, up to eight times a day. Although 99% of the bismuth passes unaltered and unabsorbed into the feces, the salicylate is absorbed in the stomach and small intestine. Alterations in the balance or composition of the microflora are responsible for antibiotic-associated diarrhea and possibly other disease conditions (see Chapter 51). Probiotic preparations containing a variety of bacterial strains have shown some degree of benefit in acute diarrheal conditions, antibiotic-associated diarrhea, and infectious diarrhea (Menees et al. Empiric Antibiotic Therapy the use of empiric antibiotic therapy for acute diarrhea (therapy given in the absence of diagnostic evaluation) must be carefully balanced with the risks. In patients with suspected or proven enterohemorrhagic Escherichia coli, antibiotics should be avoided because of the risk of hemolytic uremic syndrome. Similarly, in patients with suspected Clostridium difficile, other antibiotics should be discontinued if possible. Azithromycin (500 mg per day for 13 days, or a maximum of 1000-mg single dose) and rifaximin (200 mg three times per day for up to 3 days) are alternative therapeutic agents. In addition, loperamide has antisecretory activity against cholera toxin and some forms of E. It acts quickly after an oral dose, with peak plasma levels achieved within 35 h. The usual adult dose is 4 mg initially followed by 2 mg after each subsequent loose stool, up to 16 mg per day. If clinical improvement in acute diarrhea does not occur within 48 h, loperamide should be discontinued. Recommended maximum daily doses for children are 3 mg for ages 25 years, 4 mg for ages 68 years, and 6 mg for ages 812 years. It is used as adjunct treatment in many forms of chronic diarrheal disease (initially as for acute diarrhea, but with typical divided daily doses of 48 mg per day), with few adverse effects. Loperamide lacks significant abuse potential and is more effective in treating diarrhea than diphenoxylate. In patients with active inflammatory bowel disease involving the colon (see Chapter 51), loperamide should be used with great caution, if at all, to avoid development of toxic megacolon. It is given orally as a 100 mg initial dose, which is repeated every 8 h as needed until diarrhea stops, for up to 7 days maximum. In children, it is given with oral rehydration solution according to body weight (1. It produces less constipation than loperamide and has minimal other adverse effects (headache, itching). Diphenoxylate and its active metabolite difenoxin (diphenoxylic acid) are related structurally to meperidine. As antidiarrheal agents, diphenoxylate and difenoxin are somewhat more potent than morphine (Menees et al. Both drugs are listed as schedule V controlled substances by the Drug Enforcement Agency, and both are coformulated with atropine to discourage habituation. Both compounds are extensively absorbed after oral administration, with peak levels achieved within 12 h. Diphenoxylate is rapidly deesterified to difenoxin, which is eliminated with a t1/2 of about 12 h. The usual dosage for adults is 2 tablets initially (diphenoxylate or difenoxin), then 1 tablet every 34 h, not to exceed 20 mg/d (diphenoxylate) or 8 mg/d (difenoxin). If chronic diarrhea does not improve within 10 days at the maximum daily dose, then these agents are not likely to be effective. Once symptoms are controlled, dosing should be reduced; if no effect is seen in 48 h, the drug is unlikely to be effective. They are available in preparations containing small doses of atropine (considered subtherapeutic) to discourage abuse and deliberate overdosage: 25 g of atropine sulfate per tablet with either 2. With excessive use or overdose, constipation and (in inflammatory conditions of the colon) toxic megacolon may develop. Opioids used for diarrhea include codeine (in doses of 30 mg given three or four times daily) and opium-containing compounds. Paregoric (camphorated opium tincture) contains the equivalent of 2 mg of morphine per 5 mL (0. The two tinctures sometimes are confused in prescribing and dispensing, resulting in dangerous overdoses.