General Information about Loratadine
One of the principle makes use of of loratadine is for the aid of nasal and non-nasal symptoms of seasonal allergic rhinitis, also called hay fever. This condition happens when the physique's immune system overreacts to allergens, such as pollen or pet dander. Symptoms can embody sneezing, congestion, runny nostril, itching in the nose and throat, and watery eyes. Claritin works by blocking the effects of histamine, lowering these bothersome signs and offering reduction for the particular person affected by allergies.
Loratadine is out there in a quantity of types, including tablets, liquid, and chewable tablets. It is often taken once a day, and the dosage for adults and kids over the age of 6 is 10 mg. For children between the ages of two and 5, the dosage is 5 mg as soon as a day. It is essential to observe the beneficial dosage and not to exceed the every day restrict, as this might lead to opposed effects.
Claritin just isn't recommended for youngsters under 2 years of age, and pregnant or breastfeeding girls should seek the guidance of their doctor earlier than taking it. In some instances, loratadine may not be suitable for people with specific medical circumstances, corresponding to liver disease or kidney problems. It is essential to at all times learn the label and comply with the instructions to be used.
In conclusion, loratadine, or Claritin, is a commonly used antihistamine that offers reduction for people suffering from seasonal allergic reactions and chronic idiopathic urticaria. Its effectiveness and relatively low threat of unwanted effects make it a popular alternative for those in search of relief from allergic reactions and hives. However, it is important to use it as directed and to consult a healthcare skilled in case you have any issues or questions.
While loratadine is generally secure and well-tolerated, it might cause some unwanted effects in some people. These can embrace dry mouth, headache, drowsiness, and stomach upset. It is necessary to note that loratadine might interact with certain medications, so it's essential to seek the guidance of a physician or pharmacist before taking it in case you are already taking different drugs.
Loratadine, commonly identified by its brand name Claritin, is a well-liked over-the-counter treatment that's used to alleviate symptoms of seasonal allergies and chronic urticaria. It belongs to a class of medication known as antihistamines, which work by blocking the motion of histamine, a chemical that is responsible for causing allergy signs corresponding to sneezing, itching, and watery eyes.
Another use of Claritin is for the treatment of chronic idiopathic urticaria, a skin situation characterized by itchy, raised welts on the skin that can seem all of a sudden and final for a quantity of hours or days. Chronic urticaria, also called hives, is commonly attributable to an allergic reaction to certain foods, medicines, or environmental components. Loratadine helps to scale back the symptoms of persistent idiopathic urticaria by blocking the discharge of histamine in the physique.
For this reason allergy treatment hay fever buy generic loratadine 10 mg on-line, many recommend the use of peripherally selective agents as first-line treatment for any patient who is at high risk for the development of adverse events. However, they may cause residual daytime sedation, decreased alertness, and performance impairment. A meta-analysis of performance-impairment trials did not show a clear and consistent distinction between diphenhydramine and the peripherally selective agents. Dry mouth, difficulty in voiding urine, constipation, and potential cardiovascular effects may be troublesome. Patients with a predisposition to urinary retention (eg, older men and those on concurrent anticholinergic therapy) should use antihistamines with caution. Caution also should be used for patients with increased intraocular pressure, hyperthyroidism, and cardiovascular disease. Other adverse effects of oral antihistamines include loss of appetite (and paradoxically, weight gain with increased appetite), nausea, vomiting, and epigastric distress. Antihistamines are only fully effective when taken approximately 1 to 2 hours before anticipated exposure to the offending allergen. This must be discussed with patients who face exposure daily during a pollen season and with those who have indoor perennial allergens where daily scheduled use is necessary. If tolerance develops to the therapeutic effect, a change to an agent in a different chemical class is usually effective. Patients should check with their healthcare professional and read labels before taking nonprescription medications. Table 95-6 lists the recommended dosages of the commonly used agents with their prescription status. Because many of the older agents are available generically, they are much less expensive. Patient cost for many of the older nonprescription agents is less than $5 for a 30-day supply, compared with more than $20 for some of the nonprescription selective agents and more than $70 for the selective prescription-only products. The selective agents have moved ahead of the nonselective choices in a recent survey of pharmacist recommended over-the-counter antihistamines. For seasonal and persistent allergic rhinitis, the intranasal antihistamine azelastine is available. Despite this labeling, recent guidelines favor the use of the intranasal route for seasonal but not persistent allergic rhinitis. Patient satisfaction has been varied because while the product produces rapid symptom relief, patients complain of drying effects, headache, and diminished effectiveness over time. Allergic conjunctivitis, often associated with allergic rhinitis, can be treated with ophthalmic antihistamines such as levocabastine or bepotastine. Because systemic antihistamines usually are also effective for allergic conjunctivitis, one of these ophthalmic agents is a logical addition to nasal steroids when ocular symptoms occur, and it is an acceptable approach for patients whose only symptoms involve the eyes or to add for those whose symptoms persist on oral treatment. Decongestants Topical and systemic decongestants are sympathomimetic agents that act on adrenergic receptors in the nasal mucosa, producing vasoconstriction. When nasal congestion occurs with allergic rhinitis, decongestants work well in combination with antihistamines. Topical Decongestants Topical decongestants are applied directly to swollen nasal mucosa via drops or sprays. However, prolonged use of these agents (for more than 3 to 5 days) can result in a condition known as rhinitis medicamentosa, or rebound vasodilation, with even more severe congestion. Patients who develop this condition use increasingly more spray more often with less response. Although the methods used to treat this "addiction" have not been studied formally, several are used commonly. Abrupt cessation works, but it is difficult because of rebound congestion that may leave the patient congested for several days or weeks. Weaning the patient off topical decongestants can be accomplished by decreasing the dosing frequency or the concentration over several weeks. Other adverse effects of topical decongestants include burning, stinging, sneezing, and dryness of the nasal mucosa. Patients should be counseled on the use of topical decongestants to prevent rhinitis medicamentosa. Patients should be instructed to use as small a dose as possible as infrequently as possible and only when absolutely necessary (eg, at bedtime to aid in falling asleep). Systemic Decongestants Oral decongestants are not as effective on an immediate basis as the topical agents, but their effects sometimes last longer and they cause less local irritation. The use of phenylephrine is increasing because of regulations related to pseudoephedrine described below. Legal requirements for the sale of pseudoephedrine were put into place to combat the misuse of the drug as a component in making methamphetamine. Pseudoephedrine must now be sold behind the counter, and the monthly amount a patient can purchase is limited. Until this requirement, pseudoephedrine was the most frequently used systemic decongestant, and it was considered the safest. Doses of 180 mg have been shown to produce no measurable change in blood pressure or heart rate. Stroke, related to use of oral decongestants such as pseudoephedrine, can occur in patients with hypertension and/or vasospasm. Severe hypertensive reactions can occur when pseudoephedrine is given concomitantly with monoamine oxidase inhibitors. Combination Products Numerous products combine an antihistamine with a decongestant. While the combination may be rational because of the different mechanisms of action, remember that antihistamines must be taken on a regular schedule, but decongestants should only be used when needed.
If these are unsuccessful allergy shots portland oregon 10 mg loratadine order visa, patients often are sent to a pain clinic or neurologist for further evaluation. The numb variant of peripheral neuropathy is not treated with medications, but may lead to pressure areas on the foot and subsequent ulceration. Clinical manifestations of diabetic autonomic neuropathy may include resting tachycardia, exercise intolerance, orthostatic hypotension, constipation, gastroparesis, erectile dysfunction, anhidrosis, heat intolerance, gustatory sweating, dry skin, impaired neurovascular function, and hypoglycemic unawareness. Improved glycemic control, discontinuation of medications that slow gastric motility, and the use of metoclopramide for only a few weeks at a time or low dose erythromycin may be helpful. A differential versus celiac disease, exocrine insufficiency, and gut bacterial overgrowth should be considered. Diabetic diarrhea frequently responds to a 10- to 14-day course of an antibiotic such as doxycycline or metronidazole. If a patient develops orthostatic hypotension, antihypertensive agents should be stopped and dietary sodium intake should be liberalized. Some patients may require pharmacologic treatment for orthostatic hypotension with mineralocorticoids or adrenergic agonist agents. In severe cases, supine hypertension may be extreme, mandating that the patient sleep in a sitting or semirecumbent position. Erectile dysfunction is common in diabetes, and initial treatment should include a trial of one of the phosphodiesterase type 5 inhibitors prior to referral. People with diabetes often require the highest doses of these medications to have an adequate response. Autonomic neuropathy may also result in gustatory sweating after eating, which may be treated with antiperspirants or anticholinergic drugs. Hypoglycemic unawareness requires the patient to avoid hypoglycemia, as the body will slowly increase the glycemic level at which it will signal the autonomic signals. Focal neuropathies are uncommon, but occur more often in older patient with poorly controlled diabetes. Diabetic amyotrophy, which is characterized by a proximal thigh muscle pain and weakness, is one of the most debilitating. The clinical presentation can be quite dramatic, but the course is usually self-limited, and partial or full recover occurs in a few weeks to months. Carpal tunnel syndrome, caused by radial nerve entrapment in wrist, is also more common in people with diabetes, and tarsal tunnel syndrome may cause foot paresthesias. There are three methods for assessing microalbuminuria: (1) measurement of the urine albumin:creatinine ratio can be determined in a random spot collection, preferably the first morning void. Microalbuminuria on a spot urine specimen is defined as a ratio of 30 to 300 mg/g (3. On timed collections, microalbuminuria is defined as 30 to 300 mg/24 h or an albumin excretion rate of 20 to 200 mcg/min. Due to day-to-day variability, microalbuminuria should be confirmed on at least two of three samples over 3 to 6 months unless the results are unequivocally positive. Additionally, when assessing urine protein or albumin, conditions that may cause transient elevations in urinary albumin excretion should be excluded. These conditions include intense exercise, recent urinary tract infections, hypertension, short-term hyperglycemia, heart failure, and acute febrile illness. Glucose and blood pressure control are important for preventing and retarding the progression of nephropathy. Diuretics frequently are necessary due to the volume-expanded state of the patient and are recommended second-line therapy. Smoking cessation, correction of lipid abnormalities, good glycemic control, and antiplatelet therapy are important strategies in treating peripheral arterial disease. Revascularization is successful in selected patients; however, small vessel disease that cannot be bypassed is common in diabetes. Local debridement and appropriate footwear are vitally important in the early treatment of foot lesions. In more advanced lesions, multiple treatments including grafts, topical wound healing, and hyperbaric treatments may be necessary. Foot examinations each visit and a yearly Semmes-Weinstein 10 gram-force monofilament test to assess for loss of protective sensation can be used to identify high-risk patients that need further podiatric evaluation. The trial was stopped early when the primary efficacy endpoint of major cardiovascular events was reduced by 37% (P = 0. The Heart Protection Study randomized 5,963 patients age more than 40 years with diabetes and total cholesterol more than 135 mg/dL (3. Low-density lipoprotein cholesterol has been the primary target of therapy for years. In people with type 1 or type 2 diabetes who are ages 40-75 years, the decision whether to use moderate or high intensity statin should be based on risk. High intensity statins include atorvastatin 40 to 80 mg day or rosuvastatin 20 to 40 mg day. Caution is advised when beginning statins in women of child bearing age because statins may cause birth defects. Material from this publication has been used with the permission of American Diabetes Association. Improved glycemic control, weight loss, and exercise will also have a positive impact on serum triglycerides. Efforts to reduce triglycerides with improved glycemic control, elimination of other secondary causes (including medications), and the use of fibrates, omega-3 fatty acid, or niacin can be used.
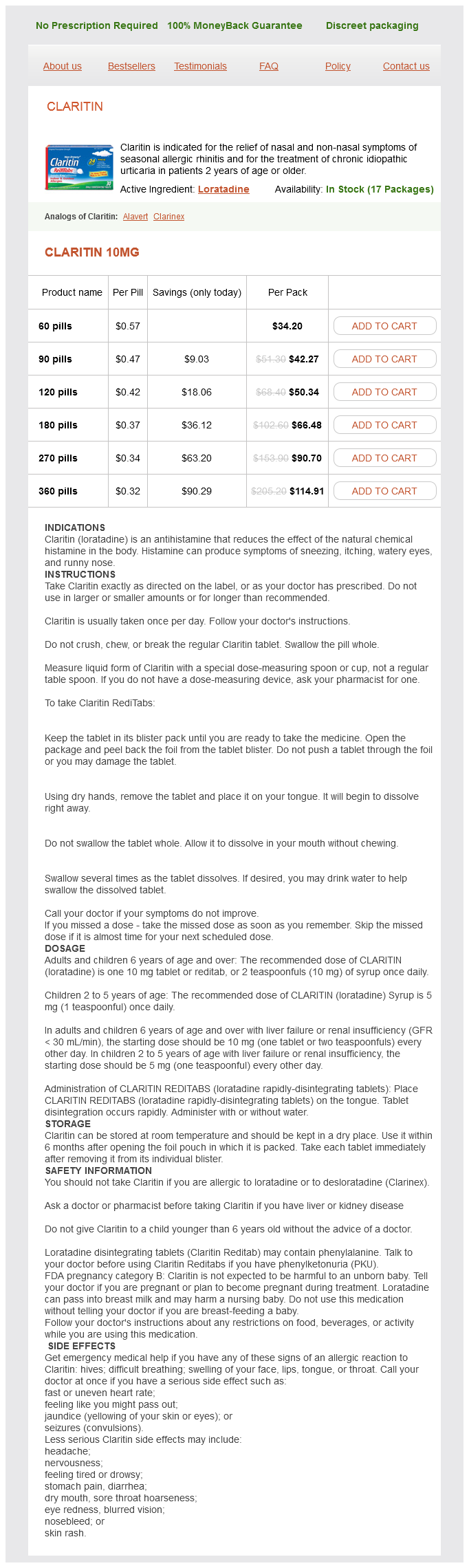
Loratadine Dosage and Price
Claritin 10mg
- 60 pills - $34.20
- 90 pills - $42.27
- 120 pills - $50.34
- 180 pills - $66.48
- 270 pills - $90.70
- 360 pills - $114.91
Health professionals with formal training and experience in diabetes education can become certified allergy testing quebec 10 mg loratadine purchase. Accredited diabetes education program can receive payment through Medicare and private health insurance plans. Since 1995, a number of new oral and injectable antidiabetic therapies have become available. Selecting the most appropriate pharmacological treatment approach has become increasing complex and a number of factors must be considered. Oral antidiabetic agents are often grouped according to their glucose-lowering mechanism of action. Sulfonylureas and meglitinides are often categorized as insulin secretagogues because they enhance endogenous insulin release. When selecting a treatment regimen medication, several factors in addition to contraindications and potential side effects should be considered. Non-glycemic effects on weight, lipids, cardiovascular outcomes and risk factors, and even the perceived -cell preservation/effects may sway the treatment selection. Historically, after the discovery of insulin by Banting and Best in 1921, frequent injections of regular insulin, the only insulin then available, were given to control the symptoms of hyperglycemia. These "long-acting" insulins enabled many patients to use only one or two injections each day. Treatment was based on symptoms of hyperglycemia and hypoglycemia, which are easily misinterpreted by patients, and by measuring glucose in the urine. Moreover, while the renal threshold for glucose is relatively predictable in young healthy subjects, it is highly variable in older patients, heart failure, and patients with renal disease. Urine glucose levels will vary with time above the renal threshold, and a significant temporal lag in appearance should be expected versus blood glucose values. The HbA1c provided a measure of glycemic control over the previous 3 months that correlated with the risk of long-term complications. Insulin sensitivity and insulin secretion are not constant throughout the day, however, which renders the concept of stable basal insulin requirements inaccurate. The timing of insulin onset, peak, and duration of effect must match meal patterns and exercise schedules to achieve near-normal blood glucose values throughout the day. One or two injections daily of any one insulin formulation will in no way mimic normal physiology, and therefore is unacceptable. The morning intermediate-acting insulin dose provides basal insulin during the day and provides "prandial" coverage for the midday meal. The evening intermediate-acting insulin dose provides basal insulin throughout the evening and overnight. If patients are very compulsive about timing of meals and carbohydrate intake, such a strategy may be acceptable. However, the majority of patients are not sufficiently predictable in their schedule or food intake to achieve "tight" glucose control with this approach. Moreover, achieving good glycemic control overnight without causing nocturnal hypoglycemia can be a challenge using a twice daily split-mixed insulin regimen. This can be a useful approach in those who decline or are unable to implement more intense insulin regimens. Several long-acting insulins can be used to provide the basal insulin component, including insulin detemir, glargine, or degludec. Bolus or prandial insulin can be provided by either regular insulin or one of the rapid-acting insulin analogs: lispro, aspart, or glulisine. The rapid onset and short duration of action of the rapid-acting insulin analogs more closely replicate normal physiology than does regular insulin. The patient reported convenience of injecting at a meal has made rapid acting insulins very popular, though trials comparing regular insulin to rapid acting insulins have found only modest improvements in glycemic control and the risk of hypoglycemia. Many patients start with a fixed dose of insulin prior to meals and then learn how to adjust the insulin dose using an "adjusted insulin scale" or a "correction factor" based on the premeal glucose readings. Patients on more advanced regimens learn to adjust the bolus insulin dose based on anticipated carbohydrate intake and physical activity. The "correction factor" is the approximate plasma glucose lowering effect of 1 unit of short-acting insulin in mg/dL. For rapid-acting insulin analogs, 1,700 or 1,800 is used when calculating the correction factor. For example, if a patient is currently taking 40 units of basal insulin and 12 units of rapid-acting insulin prior to three meals, the total daily insulin dose is 76 units. Thus each unit of rapid acting insulin analog will lower the plasma glucose approximately 22 mg/dL (1. In order to make insulin dose calculations easier for the patient to determine, this would be rounded to either 20 mg/dL or 25 mg/dL per 1 unit of insulin (1. Follow-up review of ongoing blood glucose data permits more precise individualization of the correction factor. Carbohydrate counting is an effective tool for determining the amount of rapid acting insulin that should be injected for each meal. Instead of using a fixed dose of rapid acting insulin before meals, patients can self-adjust their dose based on either estimated grams of carbohydrates or carbohydrate "choices" that will be consumed. Patient who estimate the grams of carbohydrates in their meals commonly use the "insulin to carb ratio" to determine their bolus dose. One method of calculating the insulin to carb ratio is to use 500 divided by the total daily dose of insulin.