General Information about Levonorgestrel Bp
It is important to notice that Alesse will not be suitable for everybody. Women who've a historical past of blood clots, heart disease, liver illness, or breast most cancers ought to seek the guidance of their physician earlier than beginning Alesse. Additionally, the pill may not be as efficient for ladies who're overweight or on certain medicines which will affect its absorption. It is always beneficial to seek the advice of with a healthcare skilled to find out if Alesse is the proper birth control method for one's individual wants.
In conclusion, Levonorgestrel BP (Alesse) is a extremely effective and handy birth control methodology that's extensively used by ladies to forestall pregnancy. Its excessive effectiveness, ease of use, and minimal unwanted side effects have made it a well-liked selection amongst women worldwide. However, like several medicine, it's important to make use of Alesse as directed and consult with a healthcare skilled to discover out if it is the right choice for individual wants. With using Alesse, women can have more management over their reproductive health and make knowledgeable choices about their future.
Levonorgestrel BP, also identified as Alesse, is a extremely effective birth control methodology that's taken orally to forestall ovulation and pregnancy. It is a synthetic type of the feminine hormone progesterone, and its main operate is to inhibit the release of an egg from the ovaries. Alesse is a popular contraceptive amongst women as a result of its ease of use, effectiveness, and minimal unwanted effects.
Alesse has been approved by the FDA and is extensively out there in plenty of nations all over the world. It is considered a mix birth control capsule, as it incorporates both progestin (levonorgestrel) and estrogen (ethinyl estradiol). The hormones in Alesse work collectively to thicken the cervical mucus, making it troublesome for sperm to succeed in an egg, and likewise thinning the liner of the uterus to stop implantation.
Alesse can be recognized for its ease of use. Unlike other birth control strategies similar to condoms or diaphragms, which require careful placement and attainable interruption during sexual exercise, Alesse only requires one pill to be taken at the similar time every day. This makes it a handy and discreet possibility for ladies who might not need to interrupt intimacy for contraceptive functions.
Additionally, Alesse is understood to have minimal unwanted effects in comparability with other contraception methods. Some women may experience gentle unwanted effects such as nausea, headache, or breast tenderness, but these usually subside inside the first few months of taking the tablet. Alesse also has reported positive effects on menstrual durations, such as reducing cramps and regulating the cycle.
One of the principle benefits of utilizing Alesse is its excessive stage of effectiveness. When taken correctly, it's estimated to have a 99% success fee in stopping being pregnant. This means that out of every a hundred girls using Alesse, only one might turn into pregnant. However, it is very important note that Alesse does not protect against sexually transmitted infections (STIs), and in some rare cases, when it is not taken accurately, it may not prevent pregnancy.
Some patients only have early dumping birth control for 36 year old cheap 0.18mg levonorgestrel with amex, some only have late dumping, and some have both. The initial therapy for dumping syndrome is quite effective and consists of dietary modification (AC). This includes eating frequent small meals, avoiding large amounts of carbohydrates and instead eating food high in protein and fat, and avoiding large amounts of fluids with meals. Serotonin antagonists (B) have been used for dumping syndrome but have not been routinely effective. Creation of a reversed jejunal segment (E) can be considered in the management of postvagotomy diarrhea. Efficacy of octreotide acetate in treatment of severe postgastrectomy dumping syndrome. Control of dumping symptoms by somatostatin analogue in patients after gastric surgery. In the majority of patients with a perforated duodenal ulcer, simple closure of the ulcer with an omental (Graham) patch is all that is necessary (A). In addition, a Graham patch alone should be used if the patient is unstable, if there is extensive exudative peritonitis, or if the perforation is long standing (>24 hours). However, in the setting of a patient with a known ulcer diathesis who has either already been treated for H. Pyloroplasty is typically performed along with a vagotomy because the widened outlet from the stomach to the duodenum helps circumvent any unwanted effects of the decreased gastric peristalsis and overall change in gastric emptying patterns that occur following vagotomy. Truncal vagotomy and antrectomy (C, D) is generally not recommended in the setting of perforation because of the high associated morbidity and mortality rates. Postvagotomy syndromes include diarrhea, gastric atony, and incomplete vagotomy (leading to recurrent ulceration). The diarrhea associated with vagotomy occurs more frequently and is not associated with the other cardiovascular manifestations seen with dumping syndrome (C). The initial treatment is similar to that for dumping syndrome, with dietary modifications such as frequent small meals with decreased fluid intake and an increase in fiber. Loperamide and codeine have also been shown to delay intestinal transit time and improve symptoms. In the very rare patient who does not respond to medical management, reversal of a segment of jejunum is effective in slowing transit time and improving diarrhea (D). Octreotide is not effective for postvagotomy diarrhea and may make the situation worse by decreasing pancreatic secretions and thus increasing steatorrhea (A). Effect of codeine and loperamide on upper intestinal transit and absorption in normal subjects and patients with postvagotomy diarrhoea. Alimentary Tract-Stomach 79 level, whereas hyperthyroidism increases gastrin levels (B). For those that cannot be localized, surgical exploration is still indicated because excision of the primary tumor leads to a decreased rate of liver metastasis. When exploring, it is important to be aware that 80% of gastrinomas are found within the gastrinoma (Passaro) triangle, an area defined by the junction of the cystic duct and common bile duct, the second and third portions of the duodenum, and the neck and body of the pancreas. As many as 60% of gastrinomas are within the wall of the duodenum, primarily in the first and second portions and can be very small. Thus, the next maneuver would be to perform a blind proximal duodenotomy to manually palpate the duodenal wall for tumors. Blind distal pancreatectomy and splenectomy (these share blood supply) (B) or distal duodenotomy (E) would have very low yields. A pancreaticoduodenectomy (Whipple procedure) (C) would not be indicated in this setting. It is potentially indicated for multiple duodenal or proximal pancreatic head tumors that could not be enucleated. Staging of gastric cancer involves depth of invasion (T1 invades lamina propria; T2, muscularis propria or subserosa; T3, serosa; T4, adjacent structures), nodes, and distant metastasis (E). It is approximately 80% accurate in determining whether the tumor is transmural (invading serosa, T3) but only 50% accurate in assessing whether pathologically enlarged lymph nodes are present (B). N1 disease includes 1 to 6 regional nodes; N2, 7 to 15 regional nodes; and N3, more than 15 regional nodes. Endoscopic ultrasonography in preoperative staging of gastric cancer: determination of tumor invasion depth, nodal involvement and surgical respectability. R1 indicates removal of all macroscopic disease but microscopic margins are positive for disease. A D1 resection (A) refers to removal of group 1 lymph nodes; D2 (B) refers to resection of lymph nodes in groups 1 and 2. Risk factors for gastric cancer include dietary factors such as a large consumption of smoked meats, pickled foods, high nitrates, and high salt, whereas a diet high in fruits and vegetables may be protective (D, E). PeutzJeghers syndrome is associated with a markedly increased risk of cancer in the esophagus, stomach, small bowel, colon, pancreas, breast, lung, uterus, and ovary, with a cumulative 93% risk of cancer. Gastric cancer has been categorized by Lauren into intestinal and diffuse types based on histology. The intestinal type is thought to be more related to environmental factors, is associated with chronic gastritis, and is well differentiated. The diffuse type is usually poorly differentiated and associated with signet rings and occurs in younger patients and in association with familial disorders and also with type A blood. Regional and social differences in cancer incidence of the digestive tract in the German Democratic Republic. When considering gastrinoma, it is important to be aware of the differential diagnosis of an elevated gastrin level. Causes of hypergastrinemia with increased acid production include gastrinoma, G-cell hyperplasia (not D-cell) (E), retained antrum after distal gastrectomy, renal failure, and gastric outlet obstruction. Hypergastrinemia with normal or low acid production includes pernicious anemia, postvagotomy states, use of acid-suppressive medication, and chronic gastritis.
Once remission had been achieved after an acute flare-up birth control pills jazz buy generic levonorgestrel, it is important to maintain remission. Although corticosteroids would theoretically be useful, the side effects preclude longterm administration. Infliximab is used to maintain remission, as are azathioprine and 6-mercaptopurine. Approximately three-fourths of patients with Crohn disease will eventually require surgery. Indications for surgery include failure of medical management, intestinal obstruction, fistula, abscess, bleeding, and perforation. Because patients with Crohn disease will often require repeat operations, it is important to avoid unnecessary resection of small bowel because this puts the patient at risk of short bowel syndrome. Surgical resection should be limited to the segment of bowel that is causing the complication. Other areas of active disease should be left alone provided they are not causing obvious complications. The finding of "creeping fat" or mesenteric fat wrapping is a gross feature of Crohn disease that is considered pathognomonic. It indicates the encroachment of mesenteric fat onto the serosal surface of the bowel. The presence of fat wrapping correlates well with the presence of underlying acute and chronic inflammation. A recent study suggests that adiponectin, an adipocyte-specific protein with antiinflammatory properties found in mesenteric adipose tissue, may play an important role in the inflammation seen in Crohn disease. Terminal ileitis refers to any acute inflammation of the distal ileum adjacent to the ileocecal valve and is therefore not pathognomonic. Terminal ileitis is associated with numerous infectious causes including Yersinia enterocolitica and pseudotuberculosis, Mycobacterium, cytomegalovirus (in acquired immunodeficiency syndrome), Salmonella, Campylobacter, and Shigella, among others. Overall, a minority of patients (10% in one study) who present with terminal ileitis progress to Crohn disease on long-term follow-up (C). The majority of extraintestinal manifestations in inflammatory bowel disease improve with bowel resection but ankylosing spondylitis and primary sclerosing cholangitis do not (B). Clinical manifestations of pyoderma gangrenosum associated with inflammatory bowel disease. They may cause symptoms of malabsorption due to bacterial overgrowth within the diverticula. Less commonly, bleeding can arise within the diverticulum, or diverticulitis can develop leading to perforation, which usually occurs into the retroperitoneum. Perforation requires laparotomy, and closure of the duodenal defect can be challenging and may require placing a loop of jejunum over the defect as a serosal patch. Association of periampullary duodenal diverticula with bile duct stones and with technical success of endoscopic retrograde cholangiopancreatography. There are four main cell types in the small intestine: absorptive enterocytes (E), which make up 95% of intestinal cells; goblet cells (A); Paneth cells (D); and enteroendocrine cells (C). Paneth cells secrete several substances including lysozyme, tumor necrosis factor, and cryptidins, which assist in host mucosal defense. There are more than 10 distinct types of enteroendocrine cells that secrete various gut hormones. The interstitial Cajal cell is a specialized cell of mesodermal origin that seems to regulate peristalsis. Acquired diverticula consist of mucosa and submucosa but lack a complete muscularis and thus are considered false diverticula. They are most commonly located in the second portion of the duodenum near the ampulla of Vater and are referred to as periampullary diverticula. They arise on the mesenteric border in areas of weakness in the bowel wall where blood vessels penetrate (A). Periampullary diverticula are associated with cholangitis, pancreatitis, and sphincter of Oddi dysfunction. These latter complications are thought to be due to the location of the periampullary diverticulum, which may lead to obstruction and stasis of the common duct. The majority of patients presenting with biliary complications who are discovered to have a duodenal diverticulum can be safely treated endoscopically (C). Care must be taken during diverticulectomy to identify and preserve the sphincter, which may require cannulation of the common bile duct. They are distinguished from a Meckel diverticulum, which is a true diverticulum present at birth. Duodenal diverticula are most often discovered between ages 56 to 76 years during upper endoscopy, endoscopic retrograde cholangiopancreatography, or abdominal imaging in as many as 6% of patients (B). They are asymptomatic in the majority of patients, and thus surgery is not recommended if they are discovered incidentally either on imaging or intraoperatively. The bleeding can present as either melena or bright red blood per rectum and is due to heterotopic gastric mucosa within the Meckel diverticulum, leading to acid production and an ulcer forming in the ileum adjacent to the diverticulum. A Meckel diverticulum is a true diverticulum that is due to a failure of closure of the vitelline (omphalomesenteric) duct. An adhesive band may remain between the Meckel diverticulum and the umbilicus, leading to adhesive small bowel obstruction or volvulus (E). Bowel obstruction can also occur due to intussusception with the Meckel diverticulum as the lead point (A) or due to incarceration of the diverticulum into a hernia sac (Littre hernia). Due to the smaller potential space of a Meckel diverticulum in a child, bacterial infection leading to diverticulitis is rarely encountered (D). In Western countries, chylous ascites is most often due to malignancy and cirrhosis, whereas in Eastern and developing countries, infectious etiologies predominate, such as tuberculosis and filariasis. Other causes include post-laparotomy inflammatory disorders, trauma, radiation therapy, congenital lymphatic abnormalities, and pancreatitis.
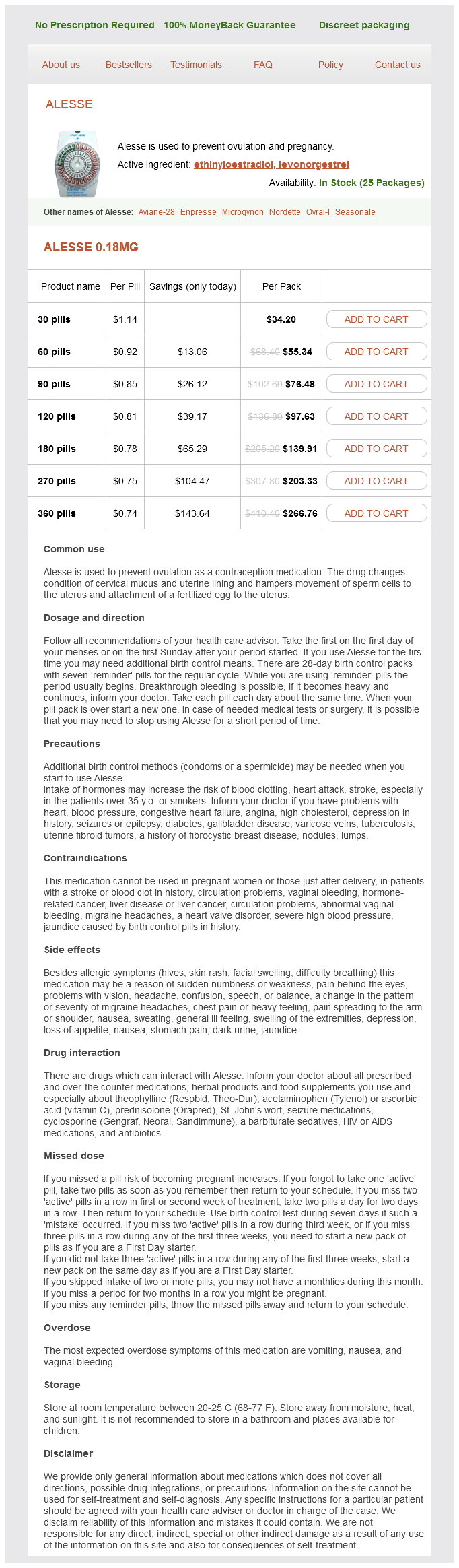
Levonorgestrel Bp Dosage and Price
Alesse 0.18mg
- 30 pills - $34.20
- 60 pills - $55.34
- 90 pills - $76.48
- 120 pills - $97.63
- 180 pills - $139.91
- 270 pills - $203.33
- 360 pills - $266.76
These include the Japan Integrated Staging score took birth control pill 6 hours late buy cheap levonorgestrel line, Cancer of the Liver Italian Program score, and Barcelona Clinic Liver Cancer Staging score. T2 is any solitary tumor with vascular invasion or multiple tumors with all lesions being smaller than 5 cm. Tumor grade is not included and does not appear to be an independent predictor of outcome (A). The diagnostic test of choice is a duplex ultrasound scan of the portal vein (BE). Some patients may have congenital webs in the portal vein (leading to stasis), and a smaller fraction have inherited hypercoagulable states. This also applies to asymptomatic patients because complete recanalization or partial resolution improves survival. Initial treatment of the bleeding varices is similar to that for adults and includes the use of sclerotherapy or banding as well as octreotide. Nevertheless, a portosystemic shunt should be considered in patients who are refractory to medical management. The finding of isolated gastric varices, without esophageal varices, is highly suggestive of splenic vein thrombosis. This condition leads to venous outflow obstruction of the spleen, resulting in massively dilated short gastric veins. The most common cause of splenic vein thrombosis is chronic pancreatitis, which leads to perivenous inflammation. Splenic vein thrombosis with gastric variceal formation is referred to as left-sided or sinistral portal hypertension. Controversy exists as to whether prophylactic splenectomy is necessary when asymptomatic gastric varices are discovered in association with splenic vein thrombosis. A recent study suggests that gastric variceal bleeding from pancreatitis-induced splenic vein thrombosis occurs in only 4% of patients. Thus, prophylactic splenectomy is not recommended in asymptomatic patients, nor is it recommended concomitant with another planned abdominal operation. Bypass procedures carry a higher risk of morbidity and would not address the underlying problem (AC). Long-term beta-blocker therapy is used as a prophylactic agent in patients with esophageal varices secondary to cirrhosis (D). The cyst becomes a trophozoite in the colon and invades the colonic mucosa, resulting in a diarrheal illness. It leads to a liquefaction necrosis of the liver, leading to the description of an "anchovy paste" appearance of the fluid, which is a combination of blood and liquefied hepatic tissue. The infection is much more common in endemic areas such as Central and South America, India, and Africa or in those individuals who have had recent travel to those locations. Amebic liver abscesses are much more common in patients with a history of heavy alcohol consumption, suggesting that alcohol increases susceptibility. The best test to establish the diagnosis is serologic testing using enzyme immunoassays. Percutaneous ultrasonography-guided aspiration is indicated only in patients who fail to improve clinically after 48 to 72 hours (C). Amebic liver abscesses may lead to mildly elevated transaminase and bilirubin levels, but these findings are nonspecific (E). The main issues to be aware of are that they can sometimes be difficult to distinguish from malignancy and that in children, in particular, giant hemangiomas can lead to arteriovenous shunting with congestive heart failure and thrombocytopenia secondary to consumptive coagulopathy (Kasabach-Merritt syndrome). Hepatic adenomas present in young women and in association with oral contraceptive use (B). Mesenchymal hamartoma of the liver typically affects young males and is considered a benign lesion that may present with intra-abdominal enlargement and respiratory distress particularly in the neonate (D). Inflammatory pseudotumor is a benign liver lesion that requires needle biopsy for correct diagnosis (E). Polycystic liver disease is an autosomal dominant disorder that is seen in patients with polycystic kidney disease, or it can be seen with liver cysts alone (B). The majority of patients are asymptomatic from their liver, but on rare occasion, large cysts can produce severe abdominal pain requiring intervention (C). Various strategies have been used with varying degrees of success in symptomatic patients with liver cysts. Laparoscopic fenestration has emerged as the preferred treatment option and has a low risk of bleeding. When all other options have been exhausted, liver transplantation has been successful. However, patients are instructed to avoid factors that have been associated with increased cyst growth. Hormone replacement therapy with estrogens in particular has been linked to cyst growth and should therefore be avoided (D). Liver function tests are typically normal but can be elevated if there is gross displacement of liver parenchyma by massive liver cysts (E). Pathophysiology, epidemiology, classification and treatment options for polycystic liver diseases. Liver resection and cyst fenestration in the treatment of severe polycystic liver disease. Postmenopausal estrogen therapy selectively stimulates hepatic enlargement in women with autosomal dominant polycystic kidney disease. Given the rapid response to oral metronidazole, aspiration or catheter-directed drainage is unnecessary in the majority of cases (BE). Aspiration is only indicated if the diagnosis of amebic liver abscess is uncertain or if the patient does not respond appropriately to antibiotics within a few days. Treatment of amoebic liver abscess with metronidazole alone or in combination with ultrasound-guided needle aspiration: a comparative, prospective and randomized study.