General Information about Januvia
Januvia, or sitagliptin, is a drugs that belongs to a category of medication called DPP-4 inhibitors. These medicine work by inhibiting the enzyme DPP-4, which breaks down a hormone known as incretin. When this hormone is not broken down, it stimulates the pancreas to produce more insulin and in addition helps to reduce the production of glucose within the liver. This helps to manage blood sugar levels and prevent them from getting too high.
One of the principle advantages of Januvia is that it is an oral treatment, which means it might be taken in tablet type rather than injected like another diabetes drugs. This makes it much more handy and user-friendly for patients who will not be comfy with injecting themselves. Additionally, Januvia doesn't cause weight achieve, which is a typical side impact of many different diabetes medications.
Januvia isn't appropriate for everybody, and it is essential to talk about any medical conditions or medications with a healthcare supplier earlier than beginning treatment. Pregnant or breastfeeding ladies must also consult with their doctor earlier than taking Januvia.
Januvia is typically taken once every day, with or without meals. The dosage may range depending on the person's wants, but you will need to observe the prescribed dosage and instructions from a healthcare supplier. It is also essential to frequently monitor blood sugar levels while taking Januvia to guarantee that it's effectively controlling blood sugar levels.
It is an oral medicine that helps to regulate blood sugar ranges by stimulating the production of insulin and reducing the manufacturing of glucose in the liver.
Type 2 diabetes is a chronic condition where the body either doesn't produce enough insulin or does not effectively use the insulin that's produced. Insulin is a hormone that helps to manage blood sugar ranges, and with out sufficient of it, glucose ranges can turn out to be too excessive. This can result in critical health issues such as heart disease, kidney injury, and nerve injury.
Like any medication, Januvia may cause unwanted side effects in some people. Common unwanted aspect effects include headache, runny or stuffy nose, sore throat, and higher respiratory tract infections. In rare cases, serious side effects such as pancreatitis, allergic reactions, and liver issues may happen. It is necessary to seek medical attention if any severe or persistent unwanted effects are skilled.
In conclusion, Januvia is a extensively used and effective medicine for the treatment of sort 2 diabetes. It helps to control blood sugar ranges and prevent critical issues related to the situation. However, you will want to follow instructions and monitor blood sugar levels regularly while taking this medicine. By working closely with a healthcare supplier, people with sort 2 diabetes can effectively handle their condition and reside a healthier life.
Pathophysiology of Acute Hematogenous Osteomyelitis Acute hematogenous osteomyelitis involves mostly the metaphyses of long bones (Cierny-Mader classification stage I) metabolic disease group purchase januvia 100 mg with mastercard. Because the infection is not confined to the metaphyses, approximately half of cases of neonatal osteomyelitis also have involvement of the adjacent joint with development of septic arthritis. The predilection of infection to the metaphyseal region is explained by its peculiar anatomy. This nonanastomosing capillary system feeds into large venous sinusoids, where the blood flow becomes slow and turbulent. Any minor trauma can lead to the development of a small hematoma, vascular obstruction, and subsequent bone necrosis. The acute infection initially produces an inflammatory infiltration, increased bone pressure, decreased pH, and decreased oxygen tension. These factors compromise the medullary circulation and enhance the spread of infection. In infants, the infection may proceed laterally through the bone cortex or through the epiphysis and joint surfaces through capillaries that cross the growth plate. Most cases of acute hematogenous osteomyelitis in children can be treated with antimicrobial therapy alone. After microbiologic specimens have been obtained, empirical antimicrobial therapy is started to cover clinically suspected organisms. When an organism is identified, the antimicrobial therapy can be changed accordingly (see Table 104. Switching from parenteral therapy to oral antimicrobial therapy can be done when the patient is afebrile and able to tolerate oral antimicrobials. Oral antimicrobial therapy should be given to compliant patients with close follow-up. A retrospective analysis of postdischarge antibiotics used in children and adolescents with acute osteomyelitis found comparable efficacy of oral versus intravenous antibiotics. The typical duration of antimicrobial therapy in children is 3 weeks (see Table 104. In adults with acute hematogenous osteomyelitis, surgical therapy often is required, followed by appropriate antimicrobial therapy based on culture and sensitivity data. Studies have implicated several genetic factors in the pathophysiology of this disease. Osteitis typically is multifocal and affects several bones, including the chest wall bones (63%), pelvis (40%), and spine (33%). The disease is self-limited, with spontaneous intermittent periods of exacerbation and remission. The differential diagnosis includes infectious osteomyelitis, bone malignancy, and other inflammatory arthritides. Patients require bone biopsy and cultures for diagnosis to exclude infectious osteomyelitis. The same caution with regard to concomitant colonic malignancy exists with osteomyelitis as with endocarditis, with 46 of 64 (71. Common causative organisms in osteomyelitis of the neonate are organisms that frequently cause neonatal sepsis, such as group B Streptococcus spp. In children, the diagnosis often is made in a patient with compatible radiologic and clinical findings with positive blood cultures. Bone radiographs may show lytic erosions similar to those of infectious osteomyelitis affecting the metaphysis. Histopathology typically is nonspecific, with a combination of acute and chronic inflammatory cells. Cultures of biopsy material are typically negative for bacteria, fungi, or mycobacteria. These conditions put these patients at risk for contiguous osteomyelitis of the extremities (see "Osteomyelitis in Patients With Diabetes Mellitus or Vascular Insufficiency"). Early reports postulated incorrectly that this disease was not infectious because of the nonresponse to antimicrobials and the "nonvirulent organisms" recovered during cultures. The disease is encountered after a variety of urologic and gynecologic surgical procedures, including Marshall-Marchetti-Krantz urethropexy, prolonged catheterization, inguinal hernia repair, vaginal delivery, and prostatectomy or radiotherapy for prostate cancer. It is believed that this form is due to an aseptic inflammation that could be triggered by surgery, by bone infarction, or in athletes. Most patients present with suprapubic pain and difficulty and pain with ambulation. In one study, the time between surgery and the diagnosis ranged from 2 to 18 months. Radiographs performed 6 months later can reveal pubic bone sclerosis, widening of the joint spaces, and rarefaction. The aseptic form of osteitis pubis could be managed with nonsteroidal antiinflammatory drugs and corticosteroids. In one study, surgical débridement of infected bone was required in more than 70% of cases. The disease may manifest with acute local pain and swelling with positive blood cultures. Fever, localized swelling or a mass, and soft tissue abscesses were present in 60%, 30%, and 30% of cases, respectively. Chronic cases should be treated with surgical débridement, followed by antimicrobial therapy. Sites of bony infarction result from recurrent episodes of vasoocclusion in an expanded marrow space. In a large cohort study of 299 patients with homozygous sickle cell anemia in France, the prevalence of osteomyelitis was 12%. The differentiation between bone infarction and osteomyelitis could be challenging because their clinical and radiologic presentations are similar.
It appears that individuals who are immune to rubella diabetes test while pregnant fasting discount januvia 100 mg buy, either by having had the natural infection or by having received rubella vaccine, may be reinfected when reexposed. However, reinfection is usually asymptomatic and detectable only by serologic means. Viremia and congenital rubella in maternal reinfection appear to be very rare events. The presence of large numbers of immune people in a community appears to be able to prevent rubella epidemics from occurring; this effect is termed herd immunity. Although it has been documented that herd immunity does not entirely eliminate the spread of rubella, it probably plays a major role in control of this infection, which is now rare in the United States. As in measles (see Chapter 160), a primary and a secondary viremia are believed to accompany rubella. Rubella virus has been detected in leukocytes of patients 1 week before the onset of symptoms. Although circulating immune complexes are detectable during rubella, they do not appear to contribute to the development of rash. However, the factors responsible for this protection are not precisely understood. Antibody titers to rubella virus develop, but the significance of the decline of antibody titers with time remains unclear. The long-term persistence of humoral and cellular immunity to rubella in a group of cloistered nuns who had no opportunity for reexposure to rubella virus has been documented. Postnatally acquired rubella is usually an innocuous infection, and, as 2009 of human synovial cells cultured in vitro was reported, and this was advanced as an explanation for the pathogenesis of chronic forms of rubella arthritis. This complication may be due to both thrombocytopenia and vascular damage, and it is probably immunologically mediated. It occurs more frequently in adults than in children, and it is associated with a mortality rate of 20% to 50%. The incidence of congenital rubella in a given population is quite variable, depending on the number of susceptible individuals, the circulation of virus in the community, and, in recent times, the use of rubella vaccine. During the first 2 months of gestation, the fetus has a 65% to 85% chance of being affected, with an outcome of multiple congenital defects or spontaneous abortion. Fetal infection during the fourth month carries a 10% risk for a single congenital defect. Occasionally fetal damage (deafness alone) is seen if rubella occurs up to the 20th week of gestation. Some children whose mothers had rubella during pregnancy and who were considered normal at birth were found to have manifestations of congenital rubella when they reached school age. In contrast, the fetus is at high risk for development of severe rubella, with serious sequelae if infected transplacentally in early pregnancy because of maternal rubella. The major clinical manifestations of postnatal rubella are adenopathy, which may last several weeks, and rash. The lymph nodes involved include the posterior auricular, posterior cervical, and suboccipital chains. An enanthem consisting of petechial lesions on the soft palate (Forschheimer spots) has been described for rubella, but this enanthem is not diagnostic for rubella (in contrast to Koplik spots in measles). Postnatal Rubella Complications of Postnatal Rubella Complications of postnatal rubella, in contrast to complications of measles, are uncommon. Arthritis or arthralgia has been reported in one-third of women with rubella; this complication is less common in children and in men. The frequency of detection and the quantity of circulating immune complexes are higher in rubella vaccinees who report joint complaints than in those with no joint involvement. This material is used by permission of Wiley-Liss, a subsidiary of John Wiley & Sons. There was no increased incidence of malignant disease in these 50-year-old survivors. It has been suggested that persistent infection with rubella virus leads to a mitotic arrest of cells, which causes inhibition of cellular growth and, consequently, retarded organ growth. The disease has been confused with other infections such as scarlet fever, mild measles, infectious mononucleosis, toxoplasmosis, roseola, erythema infectiosum, and certain enteroviral infections. Virus isolation from throat swabs, urine, synovial fluid, or other body secretions is an acceptable method for diagnosis, particularly in the early days after rash onset. Virus isolation for diagnosis of rubella and especially for congenital rubella has been largely supplanted by molecular methods such as reverse-transcriptase polymerase chain reaction. The laboratory diagnosis of postnatal rubella is most conveniently made serologically. A demonstration of specific IgG on one serum sample is evidence of immunity to rubella. Acute rubella infection may be diagnosed either by a demonstration of specific IgM in one serum sample or by a fourfold or greater increase in rubella antibody titer in acute and convalescent specimens assayed in the same test. However, some commercial assays for rubella immunity may yield false-negative results (see "Vaccination Against Rubella"). For a serologic diagnosis of congenital rubella in the neonatal period, antibody to rubella virus should be measured in both infant and maternal sera. It may be necessary to perform several antibody determinations on serum from the infant to detect whether the titer of rubella antibody is falling, which indicates passively acquired maternal antibody, or rising, which suggests rubella infection. There is no specific therapy, but for patients with fever and arthritis or arthralgia, the treatment of symptoms is indicated. With the advent of rubella vaccine, it is now recommended to immunize susceptible women of childbearing age against rubella before they become pregnant.
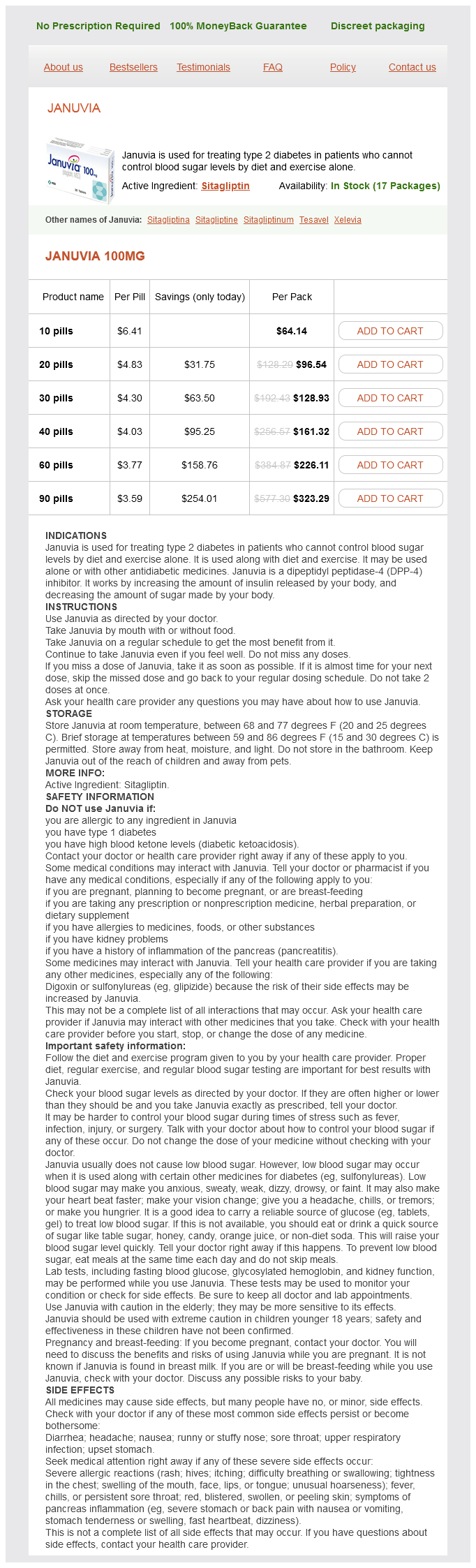
Januvia Dosage and Price
Januvia 100mg
- 10 pills - $64.14
- 20 pills - $96.54
- 30 pills - $128.93
- 40 pills - $161.32
- 60 pills - $226.11
- 90 pills - $323.29
Soaks with aluminum acetate diabetes symptoms legs bruising januvia 100 mg buy low price, or Burow solution, in the management of herpes zoster can be both soothing and cleansing. Acyclovir is approved in the United States for the treatment of both chickenpox and herpes zoster in the normal host (Table 136. Oral acyclovir therapy in healthy children, adolescents, and adults shortens the duration of lesion formation by about 1 day, reduces the total number of new lesions by approximately 25%, and diminishes constitutional symptoms in one-third of patients. In children 2 to 18 years old, the oral dosage is 20 mg/kg four times daily for 5 days (maximum 800 mg daily). Oral therapy of herpes zoster in the normal host accelerates cutaneous healing and reduces acute neuritis. Acyclovir has been evaluated in controlled studies for all herpesvirus infections. In the first part of the 21st century, the differential diagnosis of varicella and herpes zoster is less confusing than it was 20 to 30 years ago. Smallpox or disseminated vaccinia was confused with varicella because of the similar appearance of the cutaneous lesions, and it could again pose a problem in the era of bioterrorism. With the worldwide eradication of smallpox, these disease entities only serve to confound the diagnosis if used by a bioterrorist or as a complication of vaccination. The characteristic skin rash of chickenpox with lesions in all stages of development provides the basis for the clinical diagnosis of infection. The presence of pruritus, pain, and low-grade fever also helps establish the diagnosis of chickenpox. The localization and distribution of a vesicular rash make the diagnosis of herpes zoster highly likely; however, other viral exanthemas can occasionally be confused with this disease. Impetigo is usually caused by group A -hemolytic streptococci, often follows an abrasion of the skin or inoculation of bacteria at the site of the skin break, and can be associated with the formation of small vesicles in the surrounding area. Systemic signs of disease may be present if progressive cellulitis or secondary bacteremia develops. Unroofing lesions and performing a Gram stain of the scraping of the base of the lesion should reveal gram-positive cocci in chains, suggestive of streptococci, or gram-positive cocci in clusters, suggestive of staphylococci, another cause of vesicular skin lesions, or both organisms. Treatment for these latter infections is distinctly different from treatment for chickenpox and requires administration of an appropriate antibiotic. An unequivocal diagnosis can be made only by isolation of the virus in tissue culture. Disseminated enteroviral infections, particularly those caused by group A coxsackieviruses, have been reported to cause widespread distal vesicular lesions. The prodrugs of acyclovir and penciclovir-valacyclovir and famciclovir, respectively-have been licensed for therapy of herpes zoster. Both drugs appear superior to acyclovir for acceleration of cutaneous healing and are at least equally, if not more, efficacious for resolution of pain. Valacyclovir is administered to adults at a dosage of 1 g three times daily for 7 to 10 days. These medications primarily affect the acute and subacute phases of disease, as noted earlier. Dosage recommendations are 60 mg/kg every 8 hours adjusted for renal function for at least 10 days or until lesions are healed. A placebo-controlled trial, using a 2 × 2 factorial design, demonstrated significant improvement in quality of life. Complications were not encountered; however, patients at risk for complications of high-dose steroid therapy were excluded. Management of varicella pneumonitis and other complications requires excellent supportive nursing care in addition to evaluation on an individual basis of the potential need for antiviral therapy. The judicious use of analgesics ranging from nonnarcotic to narcotic derivatives is required, and drugs such as amitriptyline hydrochloride, fluphenazine hydrochloride, lidocaine patches, gabapentin, and pregabalin may be used. Patients who require hospitalization because of varicella are a source of nosocomial infection. Because approximately 10% of adults are seronegative, the risks in the hospital environment can be high. Individuals most likely to become infected are nurses and other medical personnel providing care to infected patients. Airflow can be a means of transmission of infection from one area to another in the hospital environment. For preterm hospitalized infants, guidelines for use have been recommended by the American Academy of Pediatrics Red Book Committee. A vaccine was licensed for the prevention of chickenpox in immunocompetent individuals in 1995. In immunocompromised children, serologic evidence of host response after vaccination has been achieved in 89% to 100% of vaccinated individuals. However, vaccine-induced rash is not uncommon and occurs in variable percentages of patients from approximately 6% to 47%. The factor most predictive of the appearance of rash is the degree of immunosuppression. Specifically, for children with acute lymphoblastic leukemia, the likelihood of rash can be 40% to 50%. The subsequent occurrence of natural varicella after community exposure was decreased in larger control studies and averaged 8% to 16%. Vaccination did not appear to increase the likelihood of subsequent herpes zoster during the period of follow-up. Vaccine-induced rash was far less common in these individuals and occurred at a frequency of 0.