General Information about Innopran XL
Some different circumstances that InnoPran XL is used for embody angina, irregular coronary heart rhythms, and migraines. In certain cases, it could also be prescribed for the remedy of hysteria and tremors. This versatile medication is on the market in each immediate-release and extended-release formulations, making it appropriate for various people with various wants.
InnoPran XL is primarily used for treating hypertension. It is commonly prescribed as a first-line treatment for people who have been identified with hypertension. It can be used alone or in combination with other medicines, such as diuretics, to attain optimum blood strain control.
InnoPran XL should not be taken by individuals with a historical past of asthma, sure types of coronary heart circumstances, or liver or kidney illness. It can also be not beneficial for pregnant and breastfeeding women. Therefore, it's essential to inform your physician of any pre-existing medical conditions or medications you could be taking before beginning remedy with InnoPran XL.
In comparison to different beta-blockers, InnoPran XL is known to have fewer side effects. However, as with any treatment, some people may expertise frequent unwanted aspect effects such as dizziness, fatigue, and nausea. These unwanted effects are often gentle and temporary, and they often improve after the physique gets used to the medication. It is essential to consult a health care provider if these side effects persist or turn out to be bothersome.
In conclusion, InnoPran XL is a broadly used and effective medication for managing hypertension. It has been proven to be secure and well-tolerated by most people. However, it's crucial to consult with a healthcare supplier earlier than starting remedy with this treatment. With correct medical steering and common monitoring, InnoPran XL can help individuals with hypertension to regulate their blood stress and stop severe well being complications.
One of the main advantages of InnoPran XL is that it is a long-acting medication. This signifies that it only must be taken once a day, making it handy for people with busy schedules or those who have bother remembering to take multiple doses throughout the day. The extended-release formulation also helps to take care of a continuing stage of the medication in the body, leading to better blood stress management.
Regular check-ups and monitoring of blood stress are important when taking InnoPran XL or any other treatment for high blood pressure. This helps to make certain that the treatment is working successfully and to make any essential dosage changes. It can be vital to proceed taking the medication as prescribed by your physician, even when you begin to really feel higher. Stopping medication abruptly can cause your blood pressure to rise, resulting in probably harmful well being problems.
InnoPran XL, also called propranolol, belongs to a class of medications known as beta-blockers. It works by blocking the consequences of adrenaline, a hormone that causes the center to beat faster and tougher, thereby decreasing the workload on the guts. This, in turn, helps to lower blood strain and improve blood circulate all through the body.
High blood stress, also called hypertension, is a typical well being condition that affects millions of individuals worldwide. If left untreated, it could result in critical well being problems similar to heart illness, stroke, and even kidney failure. Fortunately, there are medicines available that can effectively management and manage high blood pressure. One of these medications is InnoPran XL.
The patient should also be asked if he or she was ever referred for alcohol or other substance use counseling prehypertension in spanish order innopran xl line, family violence counseling, or a psychiatric evaluation. If the patient had a family while in the service, it is important to explore the frequency and effects of family separation on the service member, the spouse, and the children. With service members or veterans who report having been in combat, a description of the location and the events should be obtained. It is often helpful to obtain copies of service records to verify combat exposures. Witnessing atrocities, seeing the death of children, seeing friends killed and wounded, and feeling responsible for the death of a friend are especially disturbing elements of some combat and war environments for both military and civilian persons. As in all traumas, the recovery environment (that is, whether family, friends, and the nation are welcoming or ashamed) plays a large role in how the experience is recalled and managed. Some immigrants have previously lived in war zones or have served as members of military, paramilitary, or insurgent units before immigration. Some may also have been victims of torture, maltreatment, or rape as part of a war environment. Immigrants who may have served for regimes that espoused strong antiAmerican politics may fear repercussions from an unsympathetic country. These contextual issues require clear and supportive discussion in the evaluation and assessment in order to obtain necessary clinical information. Some individuals may express distress through a variety of symptoms that may abate after the conclusion of legal proceedings or payment of damages. This pattern may represent the effects of retraumatization resulting from exposure to a perpetrator or recollection of traumatic events during depositions, trial preparation, or testimony, followed by the (at times, only transient) sense of "closure" that these proceedings provide. Some persons may demonstrate waxing and waning symptoms regardless of the status of legal proceedings. By raising the possibility that secondary gain, symptom exaggeration, or malingering may be part of the clinical picture, these factors can complicate assessment and treatment planning, as well as research (35). Confidentiality can also be compromised if the treating psychiatrist is in a dual role and is also required to communicate with members of the legal system. Some of the complexity of these cases can be managed by having the treatment and forensic evaluations performed by different psychiatrists, if possible (36, 37). Determining the temporal course of symptoms relative to the timing of legal initiatives is helpful in this process (38). Patients with serious mental illness are exposed to high rates of physical assault and sexual abuse as well as other traumas (45 49). Mental health clinicians may fail to obtain this information unless they specifically inquire (50). Individuals with psychotic disorders (48) and with borderline personality disorder (50, 5254) are particularly likely to have experienced victimization in childhood and in adulthood. For a number of reasons, the medical and neurological effects of traumatic events may not be immediately apparent. Acute psychological responses to trauma such as dissociation may also diminish the initial experience of physical pain. In the presence of overwhelming anxiety and distress, individuals may not be able to describe their mental and physical state to medical professionals in an articulate fashion. Individuals exposed to traumatic events, particularly events that include interpersonal assault and violence, can find the motives of well-intentioned evaluators suspect. Without the establishment of trust, patients may be unwilling or unable to provide a complete medical or psychiatric history. Physical complaints, which may result from injury, may also represent comorbid somatization disorder or other somatoform disorders (12, 63). Similarly, patients with preexisting personality disorders or maladaptive character traits, as well as those with unresolved psychodynamic developmental concerns or histories of childhood traumatic events, may be at higher risk for an accentuated response to further traumatic events. In the presence of prominent depressive symptoms, social withdrawal and avoidance may be increased, and suicide risk may be heightened. Evaluating the safety of the patient and others As with all psychiatric patients, for patients exposed to trauma it is crucial to assess the risk for suicide and nonlethal self-injurious behavior as well as the risk for harm to others. Although many factors have been associated with an increased risk of suicide attempts and suicide in groups of individuals, it is not possible to predict suicide in a given individual at a given point in time. In assessing suicide risk, it is essential to determine whether the patient has had thoughts of death, self-harm, or suicide and the degree to which the patient intends to act on any suicidal ideation, the extent of planning or preparation for suicide, and the relative lethality of any suicide methods that the patient has considered. The availability of the means for suicide, including firearms, should also be explored, and a judgment should be made concerning the lethality of those means. Risk for suicide and for suicide attempts is also increased by the presence of previous suicide attempts, including aborted attempts. Thus, if a patient has a history of previous suicide attempts, the nature of those attempts should be determined. Treatment of Patients With Acute Stress Disorder and Posttraumatic Stress Disorder 21 Copyright 2010, American Psychiatric Association. Such behavior may progress to more serious forms of nonlethal self-harm but also confers an increased risk of suicidal behaviors. Patients should also be asked about suicide in their family and recent exposure to suicide or suicide attempts by others. An association has also been observed between the number of previous traumatic events and the likelihood that an individual will attempt suicide (67, 68). Nonetheless, it is important to assess thoughts, plans, or intentions of harming others as part of the psychiatric evaluation.
Psychodynamic approaches and other psychotherapies may facilitate this integration (124127) blood pressure keto discount 80 mg innopran xl with visa. Choice of initial treatment modality Patients assessed within hours or days after an acute trauma may present with overwhelming posttraumatic physiological and emotional symptoms that would appear to prevent or severely limit psychotherapeutic interchanges. However, pharmacological intervention to relieve overwhelming physical or psychological pain, impairing insomnia, or extremes of agitation, rage, or dissociation may restore baseline function or may be a useful temporizing measure as the clinician monitors for the development of additional symptoms and considers additional psychotherapeutic intervention and/or medication treatment. D, "Specific Treatment Strategies"), few direct comparisons of specific interventions or studies of combinations of support/education, pharmacological intervention, Treatment of Patients With Acute Stress Disorder and Posttraumatic Stress Disorder 27 Copyright 2010, American Psychiatric Association. Furthermore, in contrast to the findings for debriefing, there is no evidence to suggest that early supportive care is harmful (131134). It may be useful in addressing developmental, interpersonal, or intrapersonal issues that may be of particular importance to social, occupational, and interpersonal functioning. The presence of a comorbid psychiatric disorder may also guide initial intervention. In addition, individuals who are depressed may be at greater risk for further exposures to trauma. For example, when domestic partner violence is ongoing, low self-esteem or decreased energy accompanying depression may produce increased violence in the abusive partner or inadequate self-protective efforts in the patient. However, a systematic review of the factors that may be contributing to treatment nonresponse is possible. Since the initial treatment plan will have detailed each selected treatment, the rationale for its use, and the goals for treatment outcome, a review of this initial plan of care should help determine the extent to which therapeutic goals have been met. If interventions have been introduced sequentially, it will be easier to discern their individual effects. In reviewing the original plan, the clinician should explore with the patient which (if any) symptoms have improved, worsened, or remained the same. For example, has the patient failed to do homework assignments or discontinued medications or skipped doses because of side effects or financial difficulties The potential of other psychological disorders or underlying personality traits to interfere with the treatment should be reconsidered and addressed as needed. The therapist should inquire about any new psychosocial or other environmental factors that may be hindering therapy, such as a conflict at work or with family members. If it appears that the therapist-patient relationship is not at issue and that the patient is adhering to the treatment, the therapist should explore other options. One strategy for nonresponse is to augment the initial treatment with another-for example, adding pharmacotherapy to psychotherapy, psychotherapy to a pharmacological intervention, or couples therapy to an individual psychotherapy. Generally, the therapist should first exhaust the treatments for which there is the best evidence of efficacy before trying more novel treatments. In some cases, the original treatment may need to be discontinued and a different modality selected, as in the case of a patient who is too overwhelmed by anxiety to tolerate exposure therapy. Many promising results still require replication, and some interventions that are commonly used, based on extensive clinical experience and consensus, have yet to be examined in more methodologically rigorous studies. In the studies that are available, treatment and follow-up durations are typically short, sample sizes are frequently small, and the possibility of a placebo response is often inadequately addressed (138). It is also likely that responses to specific treatments may differ depending on the type of trauma experienced. Throughout the first 3 months after a traumatic event, recovery is the general rule (139), and this natural recovery period may extend up to 6 months (34, 140). Here, the clinician is guided by the expectation of recovery, the relief of suffering, and the use of interventions to speed recovery and to prevent additional exposure to the traumatic event, chronicity of symptoms, and relapse. Treatment of Patients With Acute Stress Disorder and Posttraumatic Stress Disorder 29 Copyright 2010, American Psychiatric Association. Although systematic study of these factors is rare, clinical experience suggests that these factors may also necessitate modification of the individual treatment plan. Specific treatment strategies should be selected to target the symptoms or symptom clusters. Personality style and family interactions may affect symptom expression, persistence, or exacerbation. Therefore, in clinical practice and in pharmacotherapy research, medications have been used in doses similar to those recommended or approved for other psychiatric illnesses. While the clinical evidence to date for each of these interventions is limited, the efficacy of combinations of education/support, psychotherapy, and psychopharmacology has been even less well characterized. Where efficacy has been established to a greater degree with regard to particular symptoms or clinical features or at particular time intervals after the trauma exposure, these findings are highlighted. While symptom reduction was generally observed within 24 weeks of treatment, symptoms of anger and irritability were reduced within the first week (149). In studies of fluoxetine, improvement in arousal, numbing, and avoidance (but not reexperiencing) and overall response were greater in women than in men. Other studies have demonstrated efficacy for these agents in intrusive, avoidance/numbing, and arousal symptoms. Smaller open-label studies of fluvoxamine have shown efficacy in sleep-related symptoms (including nightmares) in combat veterans (147, 150). In all of the trials, subjects were primarily male combat veterans, which limits the generalizability of findings. Concerns about addictive potential in individuals with comorbid substance use disorders may prompt additional caution regarding the use of benzodiazepines. Worsening of symptoms with benzodiazepine discontinuation has also been reported (158). Nonetheless, patients with these illnesses may also experience psychotic symptoms as part of a comorbid disorder. Before initiating antipsychotic treatment, careful diagnostic evaluation is required to appropriately address the potential contributions of delirium, dementia, primary thought disorders, brief psychotic reactions, delusional disorder, substance abuse, closed head injury, or other comorbid general medical conditions.
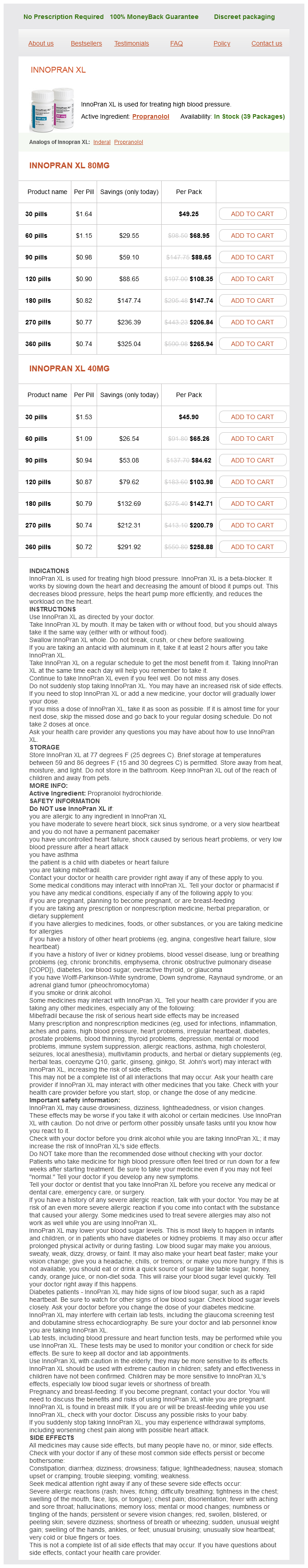
Innopran XL Dosage and Price
Innopran XL 80mg
- 30 pills - $49.25
- 60 pills - $68.95
- 90 pills - $88.65
- 120 pills - $108.35
- 180 pills - $147.74
- 270 pills - $206.84
- 360 pills - $265.94
Innopran XL 40mg
- 30 pills - $45.90
- 60 pills - $65.26
- 90 pills - $84.62
- 120 pills - $103.98
- 180 pills - $142.71
- 270 pills - $200.79
- 360 pills - $258.88
It is suggested that a list of terms that would always be considered ``serious`` could be developed to provide some guidance and to reduce uncertainty in what should be reportable to regulators arrhythmia caffeine purchase innopran xl 80 mg without a prescription. Such a list is not meant to be a substitute for case-by-case review and decisionmaking; however, it can provide a mechanism for assigning medical seriousness in the absence of detailed and confirming information. As a result, the sample list presented should not be regarded as thorough or definitive, but rather a starting point. Different users may wish to develop their own custom-designed list to serve their special needs related to the medical aspects of their products and the diseases they treat. The terms given do not necessarily refer to a serious condition per se, but may be indicative of a serious syndrome. Unexpected adverse drug experience (for a marketed drug): Any adverse drug experience that is not listed in the current labeling for the drug product. This includes events that may be symptomatically and pathophysiologically related to an event listed in the labeling, but differ from the event because of greater severity or specificity. An adverse reaction, the nature or severity of which is not consistent with the applicable product information or labeling. It is the reference information by which listed and unlisted are determined for the purpose of periodic reporting for marketed products, but not by which expected and unexpected are determined for expedited reporting. Daily dose of suspected medicinal product and regimen Route of administration Indication(s) for which suspect medicinal product was prescribed Starting date (and if relevant, time of day of treatment;. If serious, criterion or criteria for regarding the case as serious Starting date of onset of reaction (or time to onset) If not available, time interval between drug administration and start of event/reaction o If not available, treatment duration. Stopping date and time or duration of treatment For concomitant medications: o Daily dose and regimen o Stopping date and time or duration of treatment B. Whether or not the hospital discharge summary is available if patient were hospitalized. Anything relevant to facilitate assessment of the case such as medical history, relevant drug history including allergy, drug or alcohol abuse, family history. Paragraph numbering is also used for demonstration purposes to highlight the order proposed for the template. Case reference number 16041938 is a spontaneous case report sent by a hospital pharmacist which refers to a male aged 84 years. The following drugs are known to have been taken by the patient prior to the event (start date in parentheses): cimetidine (1996), steroids (1990) and tetracycline (September 9, 1999). Some 12 hours later, and 10 minutes following the latest dose, the patient developed rash, dyspnea and queasiness. Over the period of the next two days, the patient also developed chest pain and later unconsciousness. The patient was treated for the event with a beta-blocker; qweasytrol was discontinued on 8 January 2000. The patient died on 12 January 2000 from myocardial infarction; no autopsy was done. Death occurred approximately 12 days after the treatment with qweasytrol began and 4 days after it was discontinued. The company believes the following facts are also relevant in this case: as a highly selective epsilon - G2 receptor antagonist, there is no known plausible mechanism by which the drug would cause a myocardial infarction. However, if there were a rechallenge, a typical paragraph might read: Qweasytrol was subsequently reintroduced and the event did/did not recur. When qweasytrol was again discontinued, the event abated/did not abate/had an unknown outcome. Examples of Acceptable Company Clinical Evaluation Comments for Possible use in Paragraph 8 of a Standard Narrative 1. The available pre-clinical data did not suggest a possibility that the subject drug would induce -. As only limited information has been obtained so far, it is difficult to assess a cause and effect relationship. The temporal relationship (6 weeks) between the onset of the event and administration of drug x, which has a one-hour half-life, makes any causal relationship unlikely. It is of interest to note that the patient was subsequently rechallenged at the same dose without recurrence of the adverse effect. The following important information is lacking -, thus the causal relationship to drug x is not assessable. The event resolved while drug x was continued at the same dose which makes any relationship to the drug unlikely. The co-medications y and z should also be considered causative; the reported event is labeled for both drugs. This adverse event is not reflected in the prescribing information, but will be monitored closely in the future. The medication was not administered according to the dosage recommendation for the drug. The investigator on follow-up has changed his assessment from ``probably' to ``probably not' for the following reasons -. This case has also been forwarded to (name of the other manufacturer) as - (drug name) is the primary suspect drug. Examples of Unacceptable Company Clinical Evaluation Comments for Paragraph 8 of a Standard Narrative 1. The investigator changed his assessment from ``probably' to ``probably not' on follow-up. Furthermore, for products with subsequent additional regulatory approvals (new indications, new dosage forms, etc.