General Information about Glyset
Like any medication, Glyset does include some potential unwanted side effects, similar to bloating, diarrhea, and gasoline. These side effects are normally gentle and could be managed by adjusting the dosage or taking the treatment with meals. It is important to debate any potential unwanted aspect effects with a healthcare supplier and report any concerning signs.
Another good thing about Glyset is that it can be taken without regard to meals. This implies that it does not should be taken earlier than or with meals like some other diabetes medications. This added flexibility can be very helpful for individuals with busy schedules or those that wrestle with remembering to take their medicine on time.
In addition to its effectiveness in controlling blood sugar levels, Glyset also has an excellent security profile. It has been in the marketplace for over 20 years and has been studied in quite a few medical trials. It has additionally been shown to be secure for use in combination with different diabetes drugs, making it a flexible treatment possibility.
This is the place Glyset comes in. It belongs to a category of drugs known as alpha-glucosidase inhibitors, which work by slowing down the digestion and absorption of carbohydrates within the physique. Carbohydrates are the principle source of sugar in our food plan, so by slowing down their absorption, Glyset helps to stop a sudden spike in blood sugar ranges after a meal. This, in flip, helps to maintain blood sugar levels within a wholesome vary.
One of the principle benefits of Glyset is that it does not cause hypoglycemia (low blood sugar) on its own. This is a standard concern for many individuals with diabetes, particularly those who take insulin or different medicines that may result in low blood sugar. With Glyset, this danger is greatly lowered, making it a safer option for many individuals.
Type 2 diabetes is a continual condition that affects millions of people worldwide. It is characterised by high blood sugar ranges as a result of physique's inability to produce enough insulin or correctly use the insulin it produces. Over time, this will result in critical health complications, corresponding to coronary heart disease, nerve harm, and even blindness. Managing diabetes requires a combination of way of life adjustments, together with a healthy diet and regular exercise, and infrequently medicine to control blood sugar levels.
Glyset is a medicine that has been making waves within the field of diabetes management. It is an FDA-approved drug used as an adjunct to food plan and train to improve glycemic management in adults with kind 2 diabetes mellitus. In easier terms, it helps to control blood sugar ranges in individuals dwelling with diabetes, allowing them to higher handle their condition and enhance their total well being.
In conclusion, Glyset is a valuable medication within the remedy of kind 2 diabetes. It offers an efficient way to handle blood sugar levels, with out causing hypoglycemia. Its flexible dosing and good safety profile make it a handy and protected alternative for a lot of individuals with diabetes. If you or a liked one has kind 2 diabetes, discuss to your healthcare provider to see if Glyset might be a helpful addition to your remedy plan. Remember, a combination of a nutritious diet, common exercise, and correct medicine may help you keep better control of your diabetes and lead a happier, more healthy life.
Clinical studies have shown that Glyset can effectively decrease A1C levels in people with kind 2 diabetes. A1C is a measure of common blood sugar levels over the past 2-3 months and is used to assess long-term glycemic control. By reducing A1C levels, Glyset may help to forestall or delay the onset of diabetic issues, bettering the overall well being and high quality of life for those residing with the situation.
Laparoscopy: It is an invaluable diagnostic tool in the investigation of chronic pelvic pain glyset 50 mg without a prescription. It has been found that about 50% of cases with normal clinical pelvic findings have got detectable abnormality on laparoscopy. Conversely, one-third of women with detectable clinical pathology are ultimately proven to have normal pelvis on laparoscopy. The negative finding also have got value-assures the clinician that no abnormality exists. However both the syndromes (trapped and remnant) have the identical symptoms though is differentiated by amount of ovarian tissue presented. It may appear in 13% of all cases of hysterectomy with preservation of one or both the ovaries. The pain is due to tension within the developing follicle of the ovary with periovarian adhesions. Multidisciplinary approach involving a psychologist is ideal specially when no pathology could be detected. In detectable pathology: Conservative or radical surgery is to be done to remove the offending pathology. Hysterectomy is ideal for women with pelvic endometriosis or adenomyosis, when she has completed child bearing. Medical management of pain Assurance and sympathetic handling too often cure or ameliorate the pain. Neurolytic agents: Tricyclic antidepressants- Amitriptyline, Imipramine, Serotonin uptake inhibitors: Sertraline, Fluoxetine, Paroxetine, Ion channel blockers: Gabapentin, Carbamazepine. Minimal invasive surgery includes laser therapy in pelvic endometriosis or laparoscopic adhesiolysis. Polypharmacy: Some times combining drugs acting on different sites may improve pain. Oophorectomy becomes technically difficult during hysterectomy in cases with extensive endometriosis or pelvic inflammatory disease. Pain is due to the remnant of ovarian cortical tissue, left behind (retroperitoneally) unintendedly following a difficult oophorectomy. The presenting complaints are chronic pelvic pain (cyclic), deep dyspareunia and persistence of symptoms of endometriosis. Laparoscopic visualization of the remnant ovarian tissue is difficult because of adhesions. Careful dissection is needed as it is adjacent to the ureter in the retroperitoneal space. The significance of postmenopausal bleeding, whatever slight it may be, should not be underestimated. The same importance is also given to those cases where normal menstruation continues even beyond the age of 55 years. Palpation: To separate the labia for better inspection of the urethral meatus to find out any caruncle, polyp or mucosal prolapse. Speculum examination: To note the condition of the cervix and the vault of the vagina. Adequate sample is obtained with this procedure and the tissue is subjected for histological examination. Bimanual Examination Uterus may be normal, atrophic or enlarged due to pyometra or sarcoma. On the other hand, thick polypoid endometrium (910 mm), irregular texture, fluid within the uterus require further evaluation (to exclude malignancy). Endometrial biopsy may be done using pipelle cannula or the Sharman curette as an outpatient basis. Endometrial biopsy for diagnosis of endometrial carcinoma under guidance of sonohysterography or hysteroscopy has got the similar diagnostic accuracy. Detection of a benign lesion should not prevent further detailed investigations to rule out malignancy. Intake of estrogen-even if the history of intake is present, full investigations should be carried out to exclude malignancy. General Examination Obesity, diabetes and hypertension are often related to endometrial carcinoma. Breasts should be palpated because gynecological symptoms may be related to breast cancer (see p. Per abdomen: A lump in the lower abdomen may be due to pyometra or uterine sarcoma or adnexal mass. Inspection of the perineum If the uterus is outside the introitus, a decubitus ulcer may be detected (see p. If no cause is detected and there is only minimal bleeding once or twice, careful observation is mandatory, if conservatism is desired. Pelvic malignancy produces backache by involving the nerve roots, metastasis in the vertebrae or involving the lateral pelvic wall. In cases of recurrences or continued bleeding whatever may be the amount, it is better to proceed for laparotomy and to perform hysterectomy with bilateral salpingo-oophorectomy. Unexpectedly, one may find a pathology either in the ovary or fallopian tube or else, an uterine polyp-benign or malignant may be evident in the removed uterus. As such, many a breast related complaint or disease is associated with endocrine dysfunctions.
Treatment involves prolonged manual compression discount glyset 50 mg line, cessation/reversal of anticoagulation as needed, ultrasound-guided compression/thrombin injection, and, in rare cases, surgery. Radial Arteriovenous Fistula sheaths (incidence up to 2% with certain older brands of sheath). Diagnosis is by biopsy that shows sterile granulomas with chronic inflammation and giant cell reaction. Radial Artery Avulsion Arteriovenous fistula between the radial artery and the veins is a rare complication (0. Sterile Granuloma this is a rare complication due to excessive radial artery spasm during sheath removal. In some cases, the sheath should be left in place and an attempt at removal should be performed several hours later. In very rare cases, general anesthesia may be necessary to completely resolve the spasm. The artery is usually smaller than the radial Sterile granuloma at the entry site is due to chronic inflammation at the arterial entry site due to hydrophilic coated 49 artery (although this is variable), has a deeper course in the forearm and wrist making it difficult to palpate, and lies in close proximity to the neurovascular bundle at the wrist. Preprocedural considerations, access technique, and postprocedure care including closure are similar to those described under radial access. Transulnar access has been found to have a higher crossover rate due to access failure when compared with transradial access. However, in a few patient subsets, the ulnar artery pulse may be stronger than the radial and can serve as an access site for failed transradial access. The advantage of brachial access over radial access is the larger size of the artery, which can accommodate larger sheath sizes. However, brachial access carries with it the risk of distal ischemia and embolization. The brachial artery is a continuation of the axillary artery below the lower border of the teres major muscle, runs down the ventral surface of the arm into the cubital fossa on the medial aspects of the biceps brachialis, and divides into the radial and ulnar arteries. The artery is in close proximity with the median nerve, which is medial to the artery at the level of the cubital fossa. In addition, a fascia covers the brachial artery and hence a hematoma can risk compartment syndrome. The basilic vein arises from the dorsum of the hand, traverses through the medial part of the forearm and arm, continues as the axillary vein and the subclavian vein, which joins with the internal jugular vein to form the brachiocephalic vein, which drains into the superior vena cava and then into the right atrium. The basilic vein at the elbow is being increasingly used for right heart catheterization. Procedure Procedure Have the nurse insert an intravenous heplock in the basilic vein in the prep area. Exchange the line for a 5 Fr sheath in the cardiac catheterization laboratory after prepping and draping the area. In some patients, the subclavian vein joins the internal jugular vein into the brachiocephalic vein at an angle that may make the passage of the Swan-Ganz catheter difficult. Complication the arm is abducted on an arm board and the brachial artery site in and around the antecubital fossa is prepped and draped. Preprocedural considerations are similar to those described under the radial access section. The artery is palpated just proximal to the antecubital fossa where the biceps tendon can be felt. The artery is entered with the modified Seldinger technique and exchanged for a suitable size sheath. Anterior wall puncture is preferable to a through and through puncture to reduce the risk of hematoma. After access is obtained, intraarterial administration of a vasodilator cocktail will help minimize spasm. Anticoagulation with heparin (or bivalirudin for patients with heparin-induced thrombocytopenia) also can potentially reduce the risk of ischemic complications. In rare cases, perforation of the vein, especially at the point of insertion into the internal subclavian vein, can result in infraclavicular hematoma. OtherVenousAccess-Femoral/ InternalJugular Procedure ClosureandComplications After the procedure the sheath should be left in for a short period of time and removed immediately after diagnostic catheterization or after the effect of anticoagulants has worn off after interventional procedures (as described under the femoral arterial access section). The reported rates of complication are high and many patients with access complication require surgical correction (for brachial artery thrombosis or pseudoaneurysm). In addition, various vascular closure devices such as the Angio-Seal have been used for brachial artery hemostasis with a high success rate. The vein is distinguished from the artery as it is more compressible than the artery and with the triphasic Doppler signal from the artery. Once the ideal site is obtained, local anesthesia should be administered starting with the skin and working deeper (can be done under ultrasound guidance). An 18-gauge or a 20-gauge needle is then used to enter the vein under direct ultrasound guidance and using the modified Seldinger technique. Closure Manual compression is the most commonly used modality to obtain hemostasis after cannulation of the veins. Care must be taken not to pull back on the device too much as the thin-walled veins can tear. This is ideal for fully anticoagulated patients and those who receive thrombolytic agents.
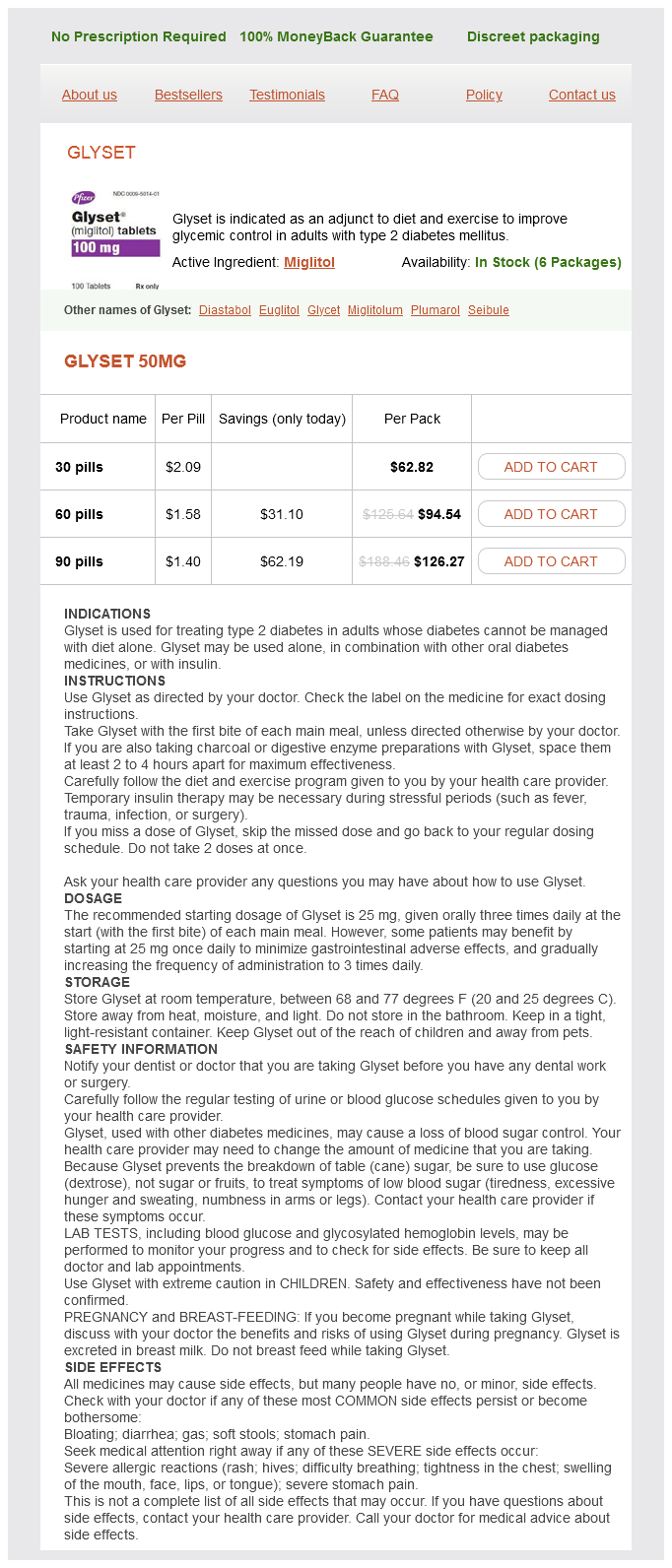
Glyset Dosage and Price
Glyset 50mg
- 30 pills - $62.82
- 60 pills - $94.54
- 90 pills - $126.27
In healthy adults more than 50 × 109 neutrophils are produced by the bone marrow and released into the circulation every day order glyset cheap online. This high rate of production is required to balance the rapid rate of neutrophil destruction and to compensate for the relatively short half-life of the neutrophil-around 8 hours. The normal range of neutrophil count varies with age and ethnic group and is highly influenced by various conditions such as stress, infections, and medication. An increase in the number of neutrophils in peripheral blood (neutrophilia) is often seen during infections of various kinds, as well as during stress or inflammation. This case shows the dramatic effects of a severe lack of neutrophils, and illustrates the essential role of neutrophils in controlling infections due to extracellular bacteria. The case of Michael Henchard: near death in infancy as a result of invasive bacterial infection. He remained in the nursery for 3 days, with no complications, and was then discharged and sent home. After 2 weeks, during which he fed and grew well, his mother noticed a slight redness around the stump of his umbilical cord. She did not think much of it at first, but after 24 hours the redness had spread and the umbilical area had become hard and swollen. His mother took him to the pediatrician, who diagnosed Michael with omphalitis (an infection of the umbilical stump) and immediately referred him for treatment at the infection ord stump Umbilical c. His abdomen was distended and the abdominal wall was very warm to the touch, hard and erythematous (reddened). The emergency room team immediately placed a venous catheter and treated Michael with fluids and broad-spectrum antibiotics. Abundant Gram-positive cocci, identified as Staphylococcus aureus, were cultured from the umbilical stump swab as well as from the blood. He was treated with the antibiotic vancomycin, and with fluids and other medication to support his cardiovascular system. His condition gradually improved and the symptoms of infection in the umbilical area subsided. His physicians therefore wondered whether his neutropenia was secondary to the infection (that is, due to bone marrow suppression) or whether he suffered from congenital neutropenia. Michael received chemotherapy, followed by allogeneic hematopoietic stem-cell transplantation from a matched unrelated donor. This is a genetically and phenotypically heterogeneous group of hereditary disorders, with an estimated frequency of around two cases per million live births. Viral infections, but also some bacterial infections, in particular Salmonella and bacterial infection of the blood (sepsis), can cause a suppression of myelopoiesis that can last for several weeks. Impaired generation of neutrophils can also be part of a broader spectrum of genetically determined disorders of bone marrow function, known as bone marrow failure syndromes. These include Fanconi anemia, dyskeratosis congenita, DiamondBlackfan anemia, ShwachmanDiamond syndrome, cartilage hair hypoplasia, and others. These disorders typically also show other hematological abnormalities, and may present with distinctive extra-hematological features (for example short stature in Fanconi anemia, and diarrhea with pancreatic insufficiency in ShwachmanDiamond syndrome). Finally, neutropenia can also reflect myelodysplasia, a condition of ineffective production of myeloid cells in the bone marrow. Myelodysplasia may progress to leukemia, with replacement of the bone marrow hematopoietic matrix by clonal proliferation of leukemic cells. Monosomy 7 is a chromosomal abnormality that is frequently observed in patients with myelodysplasia and is associated with a higher risk of leukemic transformation. Accelerated destruction of neutrophils can reflect an immune mechanism, as observed in the phenomenon of autoimmune neutropenia, which is often seen in systemic autoimmune diseases such as systemic lupus erythematosus (see Case 36). Transplacental passage of anti-neutrophil antibodies from an autoimmune mother may cause alloimmune neutropenia in the infant for up to several months after birth. Neutropenia may also be secondary to hypersplenism, a condition of spleen enlargement, associated with retention and destruction of neutrophils in the spleen. For some of these mutations, the neutropenia is associated with other manifestations. Case 25: Severe Congenital Neutropenia Conditions of chronic neutropenia must be distinguished from other situations in which the neutropenia is intermittent and follows a cyclic pattern. This page intentionally left blank to match pagination of print book Case 26 ChroniC Granulomatous Disease 151 A specific failure of phagocytes to produce H2O2 and superoxide. Uptake of microorganisms by phagocytes is enhanced by the opsonization of the particle-that is, coating it with complement, or, in the case of the adaptive immune response, with antibody and complement. One of the most important of these involves the production of hydrogen peroxide (H2O2) and superoxide radicals (O2), by a complex process that results in changes to the phagosomal pH and membrane potential, as well as the production of active bactericidal factors. These changes are critical in creating the bactericidal environment within the phagosome that facilitates the activation and function of the enzymes that are released into the phagosome. Microbes (red) are ingested by a phagocyte and Chronic Granulomatous Disease in a phagocytic vacuole, or phagosome. The enzymes are released into the phagosome, where they kill and degrade the microbe. Several other subunits, including p47phox, p67phox, p40phox, and Rac2, reside in the cytoplasm in unstimulated phagocytes. The genes encoding p47phox, p67phox, p21phox, and p40phox map to autosomal chromosomes, whereas gp91phox is encoded on the short arm of the X chromosome. In these women, because of random X chromosome inactivation, two populations of neutrophils exist. For simplicity, only four major components are shown here: gp91phox and p22phox, which together form the complex known as cytochrome b558 in the granule membranes, and p67phox and p47phox, which normally reside in the cytoplasm. The neutrophils in the right panel are from a heterozygous carrier of chronic granulomatous disease.