General Information about Glyburide
Like all medications, Micronase does have potential unwanted side effects. The commonest side effects are low blood sugar (hypoglycemia) and upset abdomen. These unwanted side effects can typically be managed by adjusting the dosage or making sure dietary adjustments. It is essential to discuss any unwanted aspect effects with a healthcare supplier to find out the most effective plan of action.
When prescribed Micronase, it is very important monitor blood sugar ranges frequently to ensure they keep inside a healthy range. The dosage might must be adjusted based on these ranges, as properly as other factors such as diet, train, and overall well being. It is necessary to observe the instructions of a healthcare provider and make any necessary dietary and way of life adjustments to effectively manage diabetes.
Type 2 diabetes is a chronic condition in which the physique either doesn't produce sufficient insulin or is unable to correctly use the insulin it produces. Insulin is a hormone that regulates blood sugar ranges, permitting cells to soak up and use glucose for energy. Without enough insulin, glucose builds up within the blood, leading to excessive blood sugar ranges. Over time, this could result in critical well being issues such as coronary heart illness, nerve damage, and kidney disease.
In conclusion, Glyburide, or Micronase, is a commonly prescribed treatment for sort 2 diabetes. By stimulating insulin production, it helps to decrease blood sugar levels and improve overall blood sugar control. However, it may be very important work carefully with a healthcare provider, make needed life-style modifications, and monitor blood sugar ranges to successfully manage diabetes. With proper care and management, individuals with kind 2 diabetes can stay a healthy and fulfilling life.
In some instances, Micronase could additionally be used in combination with different diabetes drugs to higher manage blood sugar levels. This may include insulin therapy or other oral medicines such as metformin. It is important to observe healthcare supplier directions and proceed monitoring blood sugar levels to make sure proper management of diabetes.
Micronase just isn't really helpful to be used in folks with sort 1 diabetes, as it's not efficient in stimulating insulin production in those with a non-functioning pancreas. It is also not beneficial for use in pregnant ladies or those with kidney or liver illness. Additionally, individuals with a sulfa allergy also needs to keep away from using this medication.
Micronase works by stimulating the beta cells within the pancreas to supply more insulin. This helps to decrease blood sugar ranges and improve the physique's capability to use insulin effectively. The medicine is usually taken once a day, with or without food, on the same time each day to hold up consistent ranges within the body.
Glyburide, additionally known by its model name Micronase, is a drugs commonly prescribed for the remedy of kind 2 diabetes. This medicine, classified as a sulfonylurea, helps to lower blood sugar ranges by growing the amount of insulin produced by the pancreas.
As expected diabetes injectable medications victoza 2.5 mg glyburide for sale, from cycle 7, fewer patients experienced grade 3 or 4 toxicity in arm B. Given these results, a subsequent study to evaluate a complete break from therapy was pursued. The survival benefit, adjusted for prognostic factors in a multivariate analysis, remained significant (p =. In a QoL analysis, all significant differences, except for diarrhea score, were in favor of the irinotecan group. Treatment was given until disease progression, unacceptable toxic effects, or patient refusal to continue treatment. Patients treated with irinotecan lived significantly longer than those on fluorouracil (p =. These studies taken together endorsed a role for second-line therapy for colorectal metastatic disease. The robustness of the primary analysis was supported by multivariate and subgroup analyses. Taken together, these data challenge the assumption that, in this noncurative setting, maximum tolerable treatment must necessarily be used first line. The staged approach of initial single-agent treatment upgraded to combination when required is not worse than first-line combination and is an alternative option for discussion with patients. Taken together, these results endorse a strategy of a continuum of care, in which the use of chemotherapy is tailored to the clinical setting and includes switching chemotherapy prior to disease progression, maintenance therapy, drug "holidays," and surgical resection of metastases in selected patients. Studies evaluating combination therapy compared to sequential use of single-agent chemotherapy were undertaken to address this scenario. Through random assignment, 820 patients with advanced colorectal cancer received either first-line treatment with capecitabine, second-line irinotecan, and third-line capecitabine plus oxaliplatin (sequential treatment; n = 410) or first-line treatment with capecitabine plus irinotecan and second-line capecitabine plus oxaliplatin (combination treatment; n = 410). The frequency of grades 3 to 4 toxicity over all lines of treatment did not differ significantly between the two groups, except for grade 3 hand-foot syndrome, which occurred more often with sequential treatment than with combination treatment (13% vs. Thus sequential treatment remains a valid option for patients with advanced colorectal cancer. A second study enrolled 2,135 patients randomly assigned to three treatment strategies. Bevacizumab was associated with an increase in hypertension, bleeding, and vomiting. Analysis of treatment withdrawals showed that, despite protocol allowance of treatment continuation until disease progression, only 29% and 47% of bevacizumab and placebo recipients, respectively, were treated until progression. The toxicity profile of bevacizumab was consistent with that documented in previous trials. Treatment continuation until disease progression may be necessary to optimize the contribution of bevacizumab to therapy. Although most of the preclinical data with cetuximab alone has demonstrated primarily cytostatic activity, data combining cetuximab with marginally effective or ineffective cytotoxic chemotherapy have demonstrated marked synergy with dramatic improvement in antitumor activity for the combination. In cases of disease progression, the addition of irinotecan to cetuximab monotherapy was permitted. The rate of response in the combination therapy group was significantly higher than that in the monotherapy group (22. The median time to progression was significantly greater in the combination therapy group (4. Toxic effects were more frequent in the combination therapy group, but their severity and incidence were similar to those that would be expected with irinotecan alone. Cetuximab has clinically significant activity when given alone or in combination with irinotecan in patients with irinotecan-refractory colorectal cancer. Cetuximab did not exacerbate toxicity, except for acneiform rash, diarrhea, hypomagnesemia, and associated electrolyte imbalances. This trial has not confirmed a benefit of addition of cetuximab to oxaliplatin-based chemotherapy in first-line treatment of patients with advanced colorectal cancer. The use of cetuximab in combination with oxaliplatin and capecitabine in first-line chemotherapy in patients with widespread metastases cannot be recommended. Tumor assessments by blinded central review were scheduled from week 8 until disease progression. Skin toxicities, hypomagnesemia, and diarrhea were the most common toxicities observed. Increased toxicity without evidence of improved efficacy was observed in the panitumumab arm of the irinotecan cohort. Treated patients in the cetuximab group had more grade 3 or 4 adverse events, which were attributed to cetuximab-related adverse cutaneous effects. Ten patients (23%) underwent resection with curative intent of previously unresectable metastases. The treatment resulted in a high resectability rate, which could potentially result in an improved cure rate. A total of 823 and 230 patients were randomly assigned to the oxaliplatin and irinotecan cohorts, respectively. Panitumumab was discontinued after a planned interim analysis of 812 oxaliplatin patients showed worse efficacy in the panitumumab arm. By incorporating the advances in medical management with surgical and interventional procedures, it is expected that more patients will enjoy a better survival.
The effects of two types of sleep deprivation on visual working memory capacity and filtering efficiency diabete 5g purchase glyburide 2.5 mg without prescription. Postnatal maturation of breathing stability and loop gain: the role of carotid chemoreceptor development. Treating acute insomnia: A randomized controlled trial of a "singleshot" of cognitive behavioral therapy for insomnia. Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Sleep complaints among elderly persons: An epidemiologic study of three communities. Epidemiologic study of sleep disturbances and psychiatric disorders: An opportunity for prevention Relations between sleep, fatigue, and healthrelated quality of life in individuals with insomnia. Disruption of circadian rhythms accelerates development of diabetes through pancreatic betacell loss and dysfunction. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). Some preliminary findings on physical complaints from a prospective study of 1,064,004 men and women. Cognitive Behavioral Social Rhythm Group Therapy for Veterans with posttraumatic stress disorder, depression, and sleep disturbance: Results from an open trial. Selective slow wave sleep but not rapid eye movement sleep suppression impairs morning glucose tolerance in healthy men. Weekly brief phone support in selfhelp cognitive behavioral therapy for insomnia disorder: Relevance to adherence and efficacy. A selfassessment questionaire to determine morningnesseveningness in human circadian rhythms. Comparative metaanalysis of behavioral interventions for insomnia and their efficacy in middleaged adults and in older adults 55+ years of age. The immediate effects of nasal continuous positive airway pressure treatment on sleep pattern in patients with obstructive sleep apnea syndrome. Sleep apnea related risk of motor vehicle accidents is reduced by continuous positive airway pressure: Swedish traffic accident registry data. Sleep parameters from actigraphy and sleep diary: Is the agreement important for sleep study Interindividual variation in sleep duration and its association with sleep debt in young adults. Risk factors associated with complaints of insomnia in a general adult population: Influence of previous complaints of insomnia. Estimating the economic benefits of eliminating job strain as a risk factor for depression. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Longterm cardiovascular outcomes in men with obstructive sleep apnoeahypopnoea with or without treatment with continuous positive airway pressure: An observational study. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Effect of continuous positive airway pressure treatment on blood pressure: A systematic review and metaanalysis of randomized controlled trials. The Insomnia Severity Index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Nonpharmacological interventions for insomnia: A metaanalysis of treatment efficacy. Epidemiology of insomnia: Prevalence, selfhelp treatments, consultations, and determinants of helpseeking behaviors. Measuring treatment outcomes in comorbid insomnia and fibromyalgia: Concordance of subjective and objective assessments. National Institutes of Health State of the Science Conference statement on manifestations and management of chronic insomnia in adults, June 1315, 2005. Effect of sleep apnea and continuous positive airway pressure on cardiac structure and recurrence of atrial fibrillation. Association of sleepdisordered breathing, sleep apnea, and hypertension in a large community based study. Group cognitive behavioural therapy for insomnia: Effects on sleep and depressive symptomatology in a sample with comorbidity. Prospective study of sleepdisordered breathing and hypertension: the sleep heart health study. Interactions between sleep normative data and sociocultural characteristics in the elderly. Metaanalysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Continuous positive airway pressure therapy for treating sleepiness in a diverse population with obstructive sleep apnea results of a metaanalysis. Exercise and sleepdisordered breathing: An association independent of body habitus. Prospective study of the association between sleepdisordered breathing and hypertension. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: A randomized controlled trial.
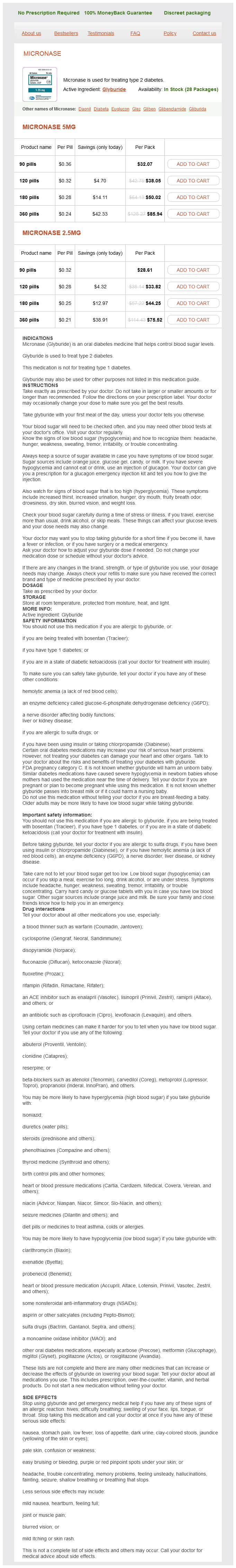
Glyburide Dosage and Price
Micronase 5mg
- 90 pills - $32.07
- 120 pills - $38.05
- 180 pills - $50.02
- 360 pills - $85.94
Micronase 2.5mg
- 90 pills - $28.61
- 120 pills - $33.82
- 180 pills - $44.25
- 360 pills - $75.52
Typically diabetes diet in hindi pdf cheap glyburide line, short-acting oral opioids have an onset of analgesia in 30 minutes, with peak effect at 60 to 90 minutes, and provide 3 to 4 hours of analgesia. Therefore, they are often used in initiation of therapy in opioid naïve patients, because their short half life may make them less risky if the patient has a dose-limiting side effect such as somnolence. Long-acting formulations of opioids are typically manufactured to provide a steady level of pain relief for 8 to 72 hours. It is recommended that patients with continuous moderate to severe pain be managed with a combination of long-acting and short-acting opioids. Pain experts have expressed concern regarding the accuracy and consistency of published opioid dose conversion tables24a and their effect on patient safety24b considering the considerable intra-individual variability in opioid pharmacoly. For most patients, morphine is considered the first opioid of choice because of its low cost and familiarity of use. Another key component to cancer pain management is frequent reassessment of pain after dose initiation or dose changes. When titrating opioids, it is best to increase doses by percentages and not by dose values. Experts recommend that opioids be increased 25% to 50% for ongoing mild to moderate pain and 50% to 100% for moderate to severe pain. The most commonly used and best studied class of adjuvant medications is anticonvulsant therapy, such as gabapentin or pregabalin, or an antidepressant medication, such as amitriptyline, nortriptyline, or duloxetine. Besides drug therapy, all patients with cancer-related pain should be evaluated for the potential use of nondrug therapies. These include education, counseling, physical modalities, and physical/occupational therapy. Patient education in itself can be a powerful analgesic intervention because it can give patients a greater sense of control and empowerment by understanding their treatment options. Simple counseling techniques can include normalization of symptoms and relaxation techniques. Interventional pain management specialists may be needed to assess for interventions such as nerve blocks or steroid injections that can improve pain control. Analgesic interventional radiology procedures are an important and emerging modality for cancer-related pain and are discussed elsewhere in this text. Therefore, if nausea persists or is particularly severe, a trial of an alternative opioid may be reasonable. Pharmacologic treatment of opioid-induced nausea is empiric with antidopaminergic antiemetics. Dopamine antagonists are a good first choice for the symptomatic treatment of nonspecific nausea in advanced cancer patients due to low cost, availability, and favorable side effect profile. Over half of all patients treated with opioids experience constipation,34 and it does not attenuate with duration of therapy. Opioids lead to constipation by inhibiting peristalsis, decreasing gastrointestinal secretions, and increasing sphincter tone. Rarely, decreasing the opioid dose is necessary if pain is well controlled and constipation is severe. Because the mechanisms of nausea can be so varied, it is important to consider a wide differential diagnosis and pursue a diagnostic workup that is focused to the most likely cause. Two of the most common etiologies for nausea in cancer patients are chemotherapy and opioid induced. For chemotherapy-induced nausea, there are well-established prophylactic drug regimens. For the treatment of delayed chemotherapy-induced nausea, dopamine blockers, glucocorticoids, and aprepitant, a neurokinin-1 inhibitor, all have demonstrated efficacy. It is exacerbated by constipation; therefore, evaluation and appropriate management of constipation is advised. For most patients, nausea is self-limiting within a few days and does not require a dose adjustment. There is some evidence that transdermal fentanyl is less constipating than oral opioids. There are four general categories of pharmacologic treatments: stimulants, bulk-forming agents, osmotic, and surfactant laxatives. Stimulants, such as senna or bisacodyl, are often used in the prevention and treatment of opioid-induced constipation. Many experts recommend scheduling these medications whenever a patient is placed on a long-acting opioid to prevent constipation from becoming severe. Bulk-forming agents, such as fiber and psyllium, have a limited role in opioid-induced constipation. Although they increase stool mass and water content, they do not promote motility so are not effective as monotherapy. There is no defined role for oral surfactant agents, such as docusate, in patients with advanced illness. Saline-based laxatives usually contain magnesium salts and can be used safely long term in lower doses. They are often used as an added agent to a stimulant laxative in opioid-induced constipation. They should be used cautiously in patients with renal failure due to concern for hypermagnesemia. They can be poorly tolerated because of their sweet taste but are generally felt to be effective as an as-needed agent.