General Information about Glucotrol XL
One of the key advantages of Glucotrol XL is its capacity to decrease blood sugar ranges without causing excessive drops or 'peaks.' This implies that it can assist to avoid the 'rollercoaster impact' of blood sugar ranges that can occur with other diabetes drugs. The extended-release formulation additionally reduces the danger of hypoglycemia (low blood sugar) in comparison with different forms of glipizide.
Glucotrol XL is generally well-tolerated, but like any treatment, it could cause unwanted side effects in some individuals. Common side effects embody nausea, diarrhea, stomach upset, and dizziness. These unwanted effects are normally delicate and may be managed by adjusting the dose or taking the medication with food. Serious unwanted effects corresponding to allergic reactions, liver problems, and low blood sugar are rare however might occur in some people.
It belongs to a bunch of medicines referred to as sulfonylureas, which work by stimulating the pancreas to provide more insulin. Glucotrol XL (glipizide prolonged release) is an oral medication that's taken once a day to help control blood sugar levels in individuals with sort 2 diabetes. It can be utilized alone or in combination with other medicines to successfully handle the illness.
Type 2 diabetes affects millions of individuals worldwide and is characterized by excessive blood sugar ranges because of the body's incapability to use insulin properly. Insulin is a hormone that helps regulate the amount of glucose within the blood. Glucotrol XL helps the physique use insulin extra effectively, thereby reducing blood sugar ranges and lowering the danger of long-term problems of diabetes corresponding to kidney illness, nerve injury, and blindness.
Glucotrol XL is usually prescribed as part of a complete treatment plan that includes lifestyle adjustments corresponding to a nutritious diet and regular train. It is important to follow the beneficial food plan, exercise, and medicine regimen to successfully handle diabetes and prevent problems.
It is essential to tell your physician in case you have a history of liver or kidney illness, as nicely as another health circumstances or medications you are taking. They may have to adjust the dose or intently monitor your blood sugar ranges to make sure the medication is secure and effective for you.
In conclusion, Glucotrol XL (glipizide extended release) is an efficient and handy medicine for managing type 2 diabetes. It works by stimulating the pancreas to produce more insulin and bettering the physique's response to it. With once-daily dosing and an extended-release formulation, it can assist maintain regular blood sugar levels and forestall the long-term complications of diabetes. However, it is very important use Glucotrol XL as a part of a complete remedy plan that features lifestyle changes for optimal administration of kind 2 diabetes. As at all times, consult with your healthcare provider earlier than starting any new medicine.
Glucotrol XL is on the market within the form of extended-release tablets, that are designed to slowly launch the medication into the body all through the day. This helps to maintain steady blood sugar levels, particularly between meals and in a single day, when blood sugar ranges can drop too low. The extended-release formulation additionally allows for once-daily dosing, making it a handy option for people with busy schedules.
The active ingredient in Glucotrol XL is glipizide, which works by stimulating the beta cells in the pancreas to provide and release extra insulin. This helps to reduce back blood sugar ranges and maintain them inside a healthy range. Glipizide also helps to enhance the body's response to insulin, which implies that the physique can use it more efficiently. This is especially helpful for people with insulin resistance, a typical condition in kind 2 diabetes where the physique is unable to make use of insulin successfully.
Inactivated influenza vaccine (1) Uses inactivated (killed) viruses that are currently prevalent jamaica diabetes diet discount 10 mg glucotrol xl fast delivery. Live attenuated intranasal vaccine (1) Uses live-attenuated strains administered intranasally that replicate poorly in the warmer lower respiratory tract. Compared with placebo, live attenuated intranasal vaccine increases nasal congestion (45% vs 27%) and sore throat (28% vs 17%). Oseltamivir and zanamivir are neuraminidase inhibitors active against influenza viruses A and B and are usually highly effective as chemoprophylaxis. Amantadine and rimantadine are not effective against influenza B (and often not against influenza A) and should not be used for chemoprophylaxis or treatment. Indications for chemoprophylaxis (1) Persons at high risk (or those who come in contact with such persons) who were vaccinated after exposure to influenza (continue treatment until 7 days after last exposure or 2 weeks after vaccination). Additionally, such patients should receive chemoprophylaxis if there was a poor match between the vaccine and circulating virus strain. When given within 48 hours of symptom onset, they reduce the symptom severity and the duration of symptoms approximately 12 days. A benefit may be present when started within 96 hours of symptoms in hospitalized patients. Taking the drug with food decreases nausea and vomiting, which occurs in 10% of patients. Drug resistance (1) A strain of influenza A (H1N1) was discovered to be resistant to oseltamivir in the 20082009 season (99% of isolates). All hospitalized patients, patients with severe influenza (pneumonia), and patients at high risk for complications including pregnant patients (see above Complications) b. Therapy should be started within 48 hours when possible but may still provide a benefit in severely sick patients when started within 5 days of symptom onset. Consider for patients without risk factors for complications who present within 48 hours of symptom onset and wish to shorten the duration of illness. A variety of clinical situations increase the likelihood that patients are colonized with multidrug resistant bacteria. Risk factors include recent or current hospitalization, mechanical ventilation, nursing home and assisted-living residence, hemodialysis, infusion therapy or immunosuppression. The diagnosis of pneumonia is typically made clinically by the presence of a new lung infiltrate and 2 of the following: fever > 38°C, leukocytosis or leukopenia, and purulent secretions. The American Thoracic Society Guidelines recommend obtaining a lower respiratory tract culture in these patients. Antimicrobial spectrum should be broadened to cover afore mentioned bacteria taking into account local resistance patterns and available culture data B. Recent recipients of antibiotics should include antibiotics from a different class C. Pertussis Textbook Presentation the typical adult with pertussis presents with "viral type" upper respiratory infection symptoms of nonproductive cough, rhinorrhea, sore throat, and sneezing. However, instead of resolving over 37 days the cough persists and is paroxysmal, often severe and occasionally even terminates in posttussive emesis. Typical symptoms include rhinitis, lacrimation, sore throat, coughing, and sneezing. Paroxysmal phase begins in the second week with fits of 510 or more forceful coughs (paroxysms) in an otherwise well appearing patient. Unusual complications from coughing in adults include hernia, pneumothorax, rib fracture, and weight loss. Among patients with cough of > 67 days the prevalence of pertussis is 3 20% but the likelihood increases in adult patients with acute cough > 3weeks 1232%. Productive cough makes pertussis unlikely (occurs in 3% of patients with pertussis) Pertussis is unlikely in patients with productive coughs. Childhood vaccination diminishes over 510 years and is rarely effective for more than 12 years. Without postexposure prophylaxis (see below) the secondary attack rate is > 80% among susceptible persons. Infected patients should avoid contact with young children and infants and working in healthcare facilities for at least 5 days after starting antibiotics. Postexposure prophylaxis recommended for people in close contacts with pertussis regardless of the immunization status. Updated Guidelines for Using Interferon Gamma Release Assays to Detect Mycobacterium tuberculosis Infection United States, 2010. Tuberculosis: still overlooked as a cause of community-acquired pneumoniahow not to miss it. Testing strategies in the initial management of patients with community-acquired pneumonia. Clinical indicators of radiographic findings in patients with suspected community-acquired pneumonia: who needs a chest x-ray Diagnostic accuracy of serum 1,3-D-glucan for Pneumocystis jiroveci pneumonia, invasive candidiasis, and invasive aspergillosis: systematic review and meta-analysis. Rapid Diagnostic Testing for Influenza: Information for Health Care Professionals. Population-based incidence of pertussis among adolescents and adults, Minnesota, 19951996. B is a previously healthy 70-year-old man who underwent right upper lobectomy for localized squamous cell lung cancer 5 days ago. On morning rounds, he comments that he is in a military barracks and that he is ready to go home. A patient whose mental status change is acute may have either fluctuating or nonfluctuating symptoms. Whereas delirium is acute, usually reversible and nearly always has an underlying, non-neurologic etiology, dementia is chronic and seldom reversible. A disturbance in attention (ie, reduced ability to direct, focus, sustain, and shift attention) and awareness (reduced orientation to the environment).
A delicate balance must be maintained between promoting calmness by pharmacologic means and minimizing the risk of hypoventilation metabolic disease specialist erie pa order glucotrol xl with mastercard. Specifically, it is important to note the mental status (lethargy, drowsiness) as well as any focal neurologic deficits the child may have. Inhalation induction may be acceptable in a child without clinical and/or radiographic evidence of severe intracranial hypertension. This effect can be attenuated by preinduction hyperventilation, but this is not an easily accomplished or feasible task in most children. The neurophysiologic effects of dexmedetomidine, an 2-agonist, is not as well understood. Studies show that it generally decreases cerebral blood volume and cerebral blood flow and has minimal effect on the cerebral metabolic rate. Stroke, commonly regarded as a problem limited to the adult population, is among the top 10 causes of death in children. Vascular abnormalities such as arteriovenous malformations, cavernous malformations, and aneurysms are the most important causes of hemorrhagic stroke, which accounts for nearly half of all stroke cases in children. Cerebrovascular arteriopathy, such as moyamoya disease, has recently become recognized as a major cause of ischemic stroke in children. However, they are an important cause of pediatric Minimizing the risk of intracranial bleeding and preventing cerebral ischemia are the most important goals in the perioperative management of children with cerebrovascular anomalies. For children with moyamoya disease, a thorough preoperative assessment, particularly of the neurologic status, is extremely important; any deficits should be noted. It is also important to obtain a baseline trend of blood pressures during both awake and asleep states to determine the lowest pressure that the child may tolerate. The child should not be subjected to prolonged periods of fasting, because dehydration may precipitate cerebral ischemia. Thus, preoperative hydration is prudent to minimize hypotension upon induction of anesthesia. Preoperative anxiolysis is recommended; hyperventilation with anxiety or with crying must be avoided, because hypocarbia will lead to cerebral vasoconstriction, which further compromises cerebral perfusion. If an intravenous catheter is not in place, a slow inhalation induction is acceptable as long as the agent is titrated to minimize change in systemic blood pressure. An arterial line should be placed as soon as possible to establish uninterrupted blood pressure monitoring. Hypocarbia is detrimental because it will induce cerebral vasoconstriction; hypercarbia should also be avoided because vasodilation of the normal vasculature may create a steal from the affected vessels. Intraoperative electroencephalography is sometimes performed to detect potential ischemia related to surgical manipulation. Any changes in anesthetic level or drug administration should be communicated to the surgical team to avoid misinterpretation of potential anestheticrelated signal changes as ischemia. The child is still at risk for cerebral ischemia even after the completion of the surgery, because several months are required for new collateral formation to become fully established after indirect bypass procedures. Direct bypass procedures may reestablish flow immediately, but there is an attendant risk of reperfusion injury that may lead to cerebral edema. For this reason, a smooth emergence with adequate analgesia is important to avoid extreme hemodynamic changes. The same principles apply to children with arteriovenous malformations who come for surgery; they are also at risk of ischemia. Sudden hemorrhage can occur during the dissection and resection of arteriovenous malformations; thus, large-bore intravenous access must be established and reserved blood products arranged. If criteria are met, the child should be extubated as soon as possible to allow for neurologic examination. The defect results from abnormal fusion of one or more vertebral posterior arches. This cleft can be covered by normal-appearing skin, which results in a hidden defect (spina bifida occulta) without involvement of the underlying neural structures. More often, both the spinal cord and meninges herniate through the spinal cleft (myelomeningocele) forming a defect that lacks a skin, and sometimes dural, covering. Overall, spina bifida represents the second most common type of congenital defect. Hairs Skin Normally, the neuroectoderm invaginates and closes to form the primary neural tube from which the future brain, spinal cord, spinal column, and overlying skin derive. Over the years, multiple teratogens and vitamin deficiencies have been implicated. The clearest causal relationship that has been established is between folic acid deficiency and myelomeningocele. However, the exact mechanism by which folic acid may be protective against myelomeningocele formation is unclear. Valproic acid and carbamazepine have also been strongly associated with neural tube defects. A likely explanation for the effect of valproic acid is that it is a known folate antagonist. Spina bifida occulta, as its name implies, is sometimes discovered only incidentally, because normal skin hides the defect and the mild spinal cleft does not usually cause neurologic deficits. Meningoceles are normally diagnosed prenatally by fetal ultrasonography or at birth by the presence of a dorsal spinal mass.
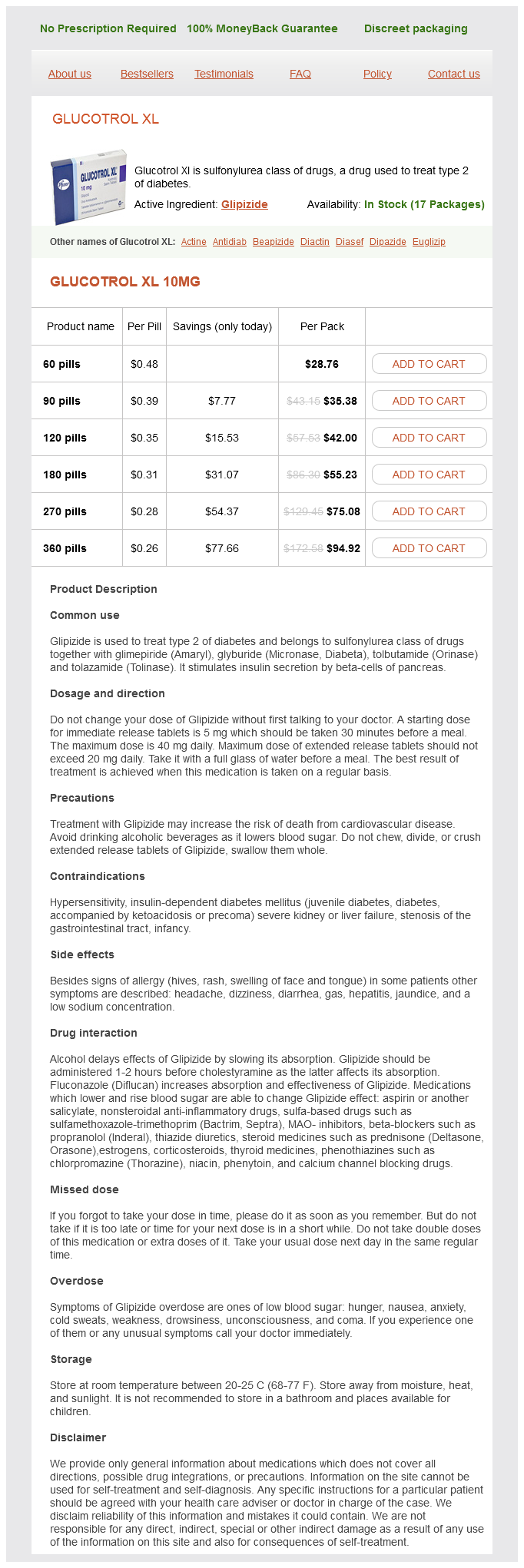
Glucotrol XL Dosage and Price
Glucotrol XL 10mg
- 60 pills - $28.76
- 90 pills - $35.38
- 120 pills - $42.00
- 180 pills - $55.23
- 270 pills - $75.08
- 360 pills - $94.92
However diabetes type 2 wiki cheap generic glucotrol xl uk, in patients with retained aganglionic bowel or acquired aganglionosis, sequelae such as severe strictures, dysfunctional bowel, or intestinal neuronal dysplasia may occur, requiring reoperation. In urgent cases, such as in the situation of concomitant enterocolitis, full-stomach precautions should be taken. Extra care should be taken in positioning, since these operations can be quite lengthy. A lithotomy position is required for anorectal pull-through procedures that involve both abdominal and perineal incisions. Intravenous catheters should be placed in the upper extremities, because the lower extremities may be included in the surgical field. Intraoperative blood loss is usually low, but third-space fluid losses can be significant. Patients may require an initial intravenous bolus of 10 to 20 mL/kg of crystalloid to offset the volume deficit resulting from bowel preparation and fasting. Epidural anesthesia provides excellent intraoperative as well as postoperative analgesia in patients undergoing open abdominal procedures. If regional techniques are not used, intravenous opioids are the mainstay of postoperative analgesia. Postoperative fluid requirements may be greater than maintenance requirements in the first 24 hours. Low lesions such as perineal fistulas, on the other hand, may be repaired during the neonatal period without an initial diverting colostomy. The majority of patients with perineal fistula and rectal atresia can attain full urinary and fecal continence after definitive repairs. More severe sacral malformations are associated with a lower rate of full bowel and bladder control. Anorectal anomalies include a spectrum of defects, most of which involve a fistula between the lower intestinal tract and the genitourinary structures. Spinal and vertebral anomalies also occur in up to 50% of patients with anorectal malformations. Cardiovascular anomalies such as atrial septal defect, patent ductus arteriosus, tetralogy of Fallot, and ventral septal defect are present in approximately one third of patients with imperforate anus. Rapid-sequence induction is often employed, particularly if abdominal distention is significant. All defects can be repaired through a posterior sagittal approach, although some patients may also require an abdominal incision to mobilize a high rectum or vagina. Extra care should be taken in positioning and padding for these lengthy procedures. Neuromuscular blocking agents should be avoided, because electrical muscle stimulation is used throughout the procedure to identify muscle structures and to define the anterior and posterior limits of the new anus. Intravenous catheters should be placed in upper extremities, because surgical positioning of the legs may impede venous flow or limit access to the intravenous catheter insertion sites. Analgesia can be provided with opioids, but these should be given to newborns and young infants in a monitored setting. Pyloric Stenosis Pyloric stenosis is one of the most common gastrointestinal abnormalities appearing in the first 6 months of life. This disorder has a polygenic mode of inheritance and occurs four times more commonly in males, more often in first-born infants, and more frequently in white infants. It is usually an isolated finding, and fewer than 10% of affected infants have other anomalies. Male infants with imperforate anus usually require emergent surgery (diverting colostomy) to relieve the obstruction, whereas in females, the presence of a rectovaginal (rectovestibular) fistula will allow passage of stool. Rectovesicular fistula is frequently seen in males and requires antibiotic prophylaxis to prevent urinary tract infection even after decompressive surgery until definitive repair is performed. Affected newborns have partial or complete intestinal obstruction and require decompression. If the infant has a fistula as well, there may also be obstructive uropathy and associated systemic infection. Pyloric stenosis presents as relentless postprandial, nonbilious projectile vomiting beginning at 2 to 5 weeks of age. Symptoms may develop as early as the first week and as late as the fifth month of life. With continued vomiting of gastric contents, which contain sodium, potassium, chloride, and hydrogen, the infant classically develops a hypochloremic, hypokalemic metabolic alkalosis. The initially alkaline urine thus becomes acidic, and this paradoxic aciduria worsens the existing metabolic alkalosis. The severity of dehydration can be assessed by physical examination of skin turgor, mucous membranes, and anterior fontanelle, and measurement of resting vital signs. The more severe the fluid and electrolyte loss, the lower the serum chloride concentration. The diagnosis can be confirmed by palpation of an olivelike mass just below the xiphoid process, although this may be difficult to do in a struggling infant. Abdominal ultrasonography is both sensitive and specific in detecting a hypertrophied pylorus. Severely dehydrated infants should receive an initial intravenous bolus (20 mL/kg) of isotonic normal saline to reexpand the intravascular volume.