General Information about Glucophage SR
So, what precisely is Glucophage SR and how does it work? Glucophage SR is a slow-release, or sustained-release, pill containing 500mg or 750mg of metformin. This signifies that the medication is slowly launched into the body over a interval of 12 hours, providing a gentle stage of the drug in the blood. This is in contrast to the immediate-release type of metformin, which is taken a quantity of occasions a day. The advantage of Glucophage SR is that it's more handy, solely needing to be taken as soon as a day, and it also reduces the likelihood of side effects corresponding to nausea, diarrhea, and abdomen upset.
Apart from its glucose-lowering effects, Glucophage SR has also been shown to have constructive results on weight reduction. As obesity is a leading threat factor for sort 2 diabetes, this is a vital profit for patients. Studies have proven that Glucophage SR can lead to a modest amount of weight loss over the course of its use, making it a super medicine for people who're fighting both diabetes and obesity.
Diabetes is a persistent illness that impacts hundreds of thousands of people worldwide. In fact, it is estimated that there are over four hundred million individuals living with diabetes and this quantity is only going to increase within the coming years. Diabetes mellitus, or just diabetes, is a situation during which the body is unable to manage its blood sugar ranges. There are several types of diabetes, however the most typical one is type 2 diabetes. This type of diabetes develops when the body becomes immune to insulin, the hormone that regulates blood sugar levels. It is often seen in adults and is usually related to obesity. Fortunately, there are drugs out there to help handle type 2 diabetes and improve the quality of life for those residing with the condition. One such medication is Glucophage SR.
Furthermore, Glucophage SR is properly tolerated by most sufferers. The commonest unwanted effects reported are gastrointestinal in nature, together with nausea, diarrhea, and stomach discomfort. These unwanted facet effects are normally gentle and have a tendency to enhance over time because the body adjusts to the medicine. It is also important to notice that Glucophage SR shouldn't be utilized in sufferers with impaired kidney perform, as this will increase the chance of a uncommon however severe side effect called lactic acidosis.
Glucophage SR is a drugs used to treat type 2 diabetes in adults. It is very beneficial for people who are chubby or overweight and haven't had success with different medications, notably the group of sulphonylurea drugs. This medicine is an extended-release type of metformin, some of the commonly prescribed oral drugs for diabetes. Metformin works by lowering sugar manufacturing in the liver and improving the physique's response to insulin, which helps to decrease blood sugar ranges.
One of the most important benefits of Glucophage SR is its capability to regulate blood sugar ranges. Studies have shown that sufferers taking this medicine expertise a major decrease of their HbA1c ranges, an essential marker for long-term blood sugar control. This implies that Glucophage SR is effectively managing the underlying explanation for sort 2 diabetes, insulin resistance. By enhancing insulin sensitivity, the body is best in a position to regulate blood sugar levels, decreasing the risk of problems related to diabetes, corresponding to heart disease, kidney illness, and nerve harm.
In conclusion, Glucophage SR is a valuable medicine in the administration of kind 2 diabetes. Its capacity to manage blood sugar ranges, assist in weight reduction, and be properly tolerated by most patients makes it a well-liked selection among healthcare providers. However, you will need to notice that Glucophage SR is just one element of a complete treatment plan for diabetes. A healthy diet, regular train, and regular check-ups with a healthcare provider are all essential in managing diabetes successfully. And as always, before starting any new medication, it is important to seek the guidance of with a healthcare professional who can determine if Glucophage SR is the best alternative for you.
Prevention is based on avoiding these agents in high-risk patients medicine identification order glucophage sr on line, whereas therapy for osmotic nephropathy is supportive with avoidance of further exposure. Clinicopathological features of acute kidney injury associated with immune checkpoint inhibitors. Renal replacement therapies for prevention of radiocontrast-induced nephropathy: a systematic review. Advanced kidney disease, gadolinium and nephrogenic systemic fibrosis: the perfect storm. Nephrotoxicity from chemotherapeutic agents: clinical manifestations, pathobiology and prevention/therapy. Association of acute interstitial nephritis with programmed cell death 1 inhibitor therapy in lung cancer patients. Li+ adversely affects several organ systems, including the kidney, which excretes this cation. This decreases expression and attenuates luminal targeting of aquaporin-2 water channels in renal epithelial cells. Although polyuria generally improves with Li+ withdrawal, amiloride therapy can further reduce urine volume by antagonizing epithelial sodium channels, which may be useful in patients who must continue on Li+. Long-term Li+ therapy can cause chronic tubulointerstitial nephritis, characterized by tubular atrophy and interstitial fibrosis, with cortical and medullary tubular microcysts. In adults, these conditions are associated with significant medication use, making these patients particularly vulnerable to the accumulation of a drug or its active or toxic metabolites. Thus a more complex adjustment scheme may be required for medications that are extensively metabolized by the liver or for which changes in protein binding and/or distribution volume have been noted. However, alterations in the peak concentration (Cmax) and in the time to which the peak concentration is attained (tmax) have been noted for a few drugs, suggesting that the rate, but not the extent of absorption, is altered. These changes are predominantly the result of altered plasma protein or tissue binding or of volume expansion secondary to reduced kidney sodium and water excretion. Changes in the conformation of albumin binding sites and accumulation of endogenous inhibitors of binding may also contribute to decreased protein binding. Regardless of the mechanism, decreased protein binding increases the free or unbound fraction of the drug. On the other hand, the plasma concentration of the principal binding protein for several basic drug compounds, 1-acid glycoprotein, is increased in kidney transplant patients and in hemodialysis patients. The net effect of changes in protein binding is usually an alteration in the relationship between unbound and total drug concentrations, an effect frequently encountered with phenytoin. The increase in the unbound fraction, to values as high as 20% to 25% from the normal of 10%, results in increased hepatic clearance and decreased total concentrations of phenytoin. Altered tissue binding may also affect the apparent volume of distribution of a drug. The absolute amount of digoxin bound to the tissue digoxin receptor is reduced, and the resultant serum digoxin concentration observed after administration of any dose is greater than expected. Monitoring of unbound drug concentrations is suggested for drugs that have a narrow therapeutic range, those that are highly protein bound (>80%), and those with marked variability in the bound fraction. Alterations in the function of and interactions between them can significantly affect the pharmacokinetic disposition and corresponding patient exposure to drugs that are substrates of nonrenal pathways. Similarly, functional expression of several intestinal and hepatic transporters is altered in experimental models of kidney disease. These studies must be interpreted with caution, however, because concurrent drug intake, age, smoking status, and alcohol intake were often not taken into consideration. However, some qualitative insight may be gained if one knows which enzymes or transporters are involved in the clearance of the drug of interest and how those proteins are affected by a reduction in kidney function. The degree of change in total body drug clearance is dependent on the fraction of the dose that is eliminated unchanged in individuals with normal kidney function, the intrarenal drug transport pathways, and the degree of functional impairment of each of these pathways. The P-gp transport system in the kidney is involved in the secretion of cationic and hydrophobic drugs. However, urine is difficult to collect accurately in most clinical settings, and the interference of many commonly used medications with creatinine measurement limits the utility of this approach. Second, when presented with various kidney function estimates that potentially translate into different drug dosing regimens, clinicians should choose the regimen that optimizes the risk-benefit ratio, given the patient-specific clinical scenario. For drugs with a narrow therapeutic range, typically more conservative kidney function estimates and corresponding doses should be used, particularly if therapeutic drug monitoring is not readily available. Third, when estimating equations are not expected to provide accurate measures of kidney function. All of these methods are poor predictors of kidney function in individuals with liver disease, and their use is not recommended for such patients. Most dosage adjustment reference sources for clinical use have proposed the use of a fixed dose or interval for patients with a broad range of kidney function. Each of these categories encompasses a broad range of kidney function, and the calculated drug regimen may not be optimal for all patients within that range. For antihypertensive agents, cephalosporins, and many other drugs for which there are no target values for peak or trough concentrations, attainment of an average steady-state concentration similar to that in normal subjects is appropriate. The principal means to achieve this goal is to decrease the dose or prolong the dosing interval. If the dose is reduced and the dosing interval is unchanged, the desired average steady-state concentration will be near normal; however, the peak will be lower and the trough higher. Alternatively, if the dosing interval is increased and the dose remains unchanged, the peak, trough, and average concentrations will be similar to those in the patients with normal kidney function. This interval adjustment method is often preferred because it is likely to yield significant cost savings due to less frequent drug administration.
One type of dipstick uses colorimetric detection of albumin bound to gold-conjugated antibody acute treatment order cheap glucophage sr on line. Normally, the urine albumin concentration is less than the 20 µg/L detection threshold for these strips. Unless the urine is very dilute, a patient with no detectable albumin by this method is unlikely to have microalbuminuria. However, because urine concentration varies widely, this assay has the same limitations as any test that only measures concentration. It is useful only as a screening test, and more formal testing is required if albuminuria is detected. A second type of dipstick has tabs for measurement of both albumin and creatinine concentration, permitting estimation of the albumin-to-creatinine ratio. In contrast to the other dipstick tests described in this chapter, these strips cannot be read by simple visual comparison with a color chart. When present on more than one determination, an albumin-to-creatinine ratio of 30 to 300 µg/ mg signifies moderately increased albuminuria. Details on the interpretation of urine albumin concentration are provided in Chapters 5 and 26. Erythrocytes originating in the renal parenchyma are dysmorphic, with spicules or blebs (acanthocytes), submembrane cytoplasmic precipitation, membrane folding, and vesicles. Studies suggest good separation between urologic and intrarenal pathology when phase contrast microscopy is used by experienced observers. In one study, up to 85% of patients with nondysmorphic microscopic hematuria had a urologic disorder, whereas 87. Cutoff points for deciding that hematuria is dysmorphic depend on the method used. The presence of proteinuria by dipstick may corroborate the presence of glomerular kidney disease. Periureteral inflammation, as in regional ileitis or acute appendicitis, may also cause pyuria. Proximal tubular cells are oval or egg shaped and tend to be larger than the cuboidal distal tubular cells. However, because size varies with urine osmolality, these cells cannot be reliably differentiated. The accuracy and reproducibility of this semiquantitative method depend on using the correct volume of urine. Twelve milliliters of urine should be spun in a conical centrifuge tube for 5 minutes at 1500 to 2000 rpm (450 g). The pellet is resuspended in the few drops of urine that remain in the tube after inversion by flicking the base of the tube gently with a finger or with the use of a pipette. The drop should be of sufficient size that a standard 22 × 22 mm coverslip just floats on the urine with a thin rim of urine at the edges. If an excess of urine is applied, it will spill onto the microscope objective or stream distractingly under the coverslip. When conventional microscopy is used, the condenser and diaphragm are adjusted to maximize contrast and definition. When the urine is dilute and few formed elements are present, detection of motion of objects suspended in the urine ensures that the focal plane is correct. One should scan the urine at low power (×100) to obtain a general impression of its contents before moving to high power (×400) to look at individual fields. It is useful to scan large areas at low power and then move to high power when an item of interest is located. In this and subsequent figures, all photographs were made from unstained sediments and were photographed at ×400 original magnification. Innumerable white blood cells as well as individual (small arrows), budding (single thick arrow), and hyphal (open arrow) fungal forms are present. They are rounded cells several times the size of leukocytes and often occur in clumps. They occur in concentrated urine from healthy individuals, as well as in numerous pathologic conditions. Immunofluorescence studies show that the fine granules are derived from altered serum proteins. Immunofluorescence studies demonstrate that they consist of a matrix of Tamm-Horsfall urinary glycoprotein (uromodulin) in the shape of the distal tubular or collecting duct segment where they were formed. The matrix has a straight margin that is helpful in differentiating casts from clumps of cells or debris. In a systematic review, waxy casts were more common in postinfectious glomerulonephritis, amyloidosis, and individuals with reduced kidney function of either short or long duration. Broad casts form in tubules that have become dilated and atrophic, and from their presence one can infer that the patient has chronic parenchymal disease. The hallmark of glomerulonephritis, they are seen less frequently with tubulointerstitial disease, including allergic interstitial nephritis. Occasionally, the evidence for intraparenchymal bleeding is a hyaline cast with embedded red cells. They are characteristic of pyelonephritis and useful in distinguishing that disorder from lower urinary tract infection. They may also chaPter4-urinaLySiSandurineMicroScoPy 39 be seen with interstitial nephritis and other tubulointerstitial disorders. Crystals, starch granules, mineral oil, and other urinary contaminants are also anisotropic. They can be difficult to type because they have similar shapes; the common urinary crystals are described in Table 4. The pH is an important clue to identity because the solubility of many urinary constituents is pH dependent.
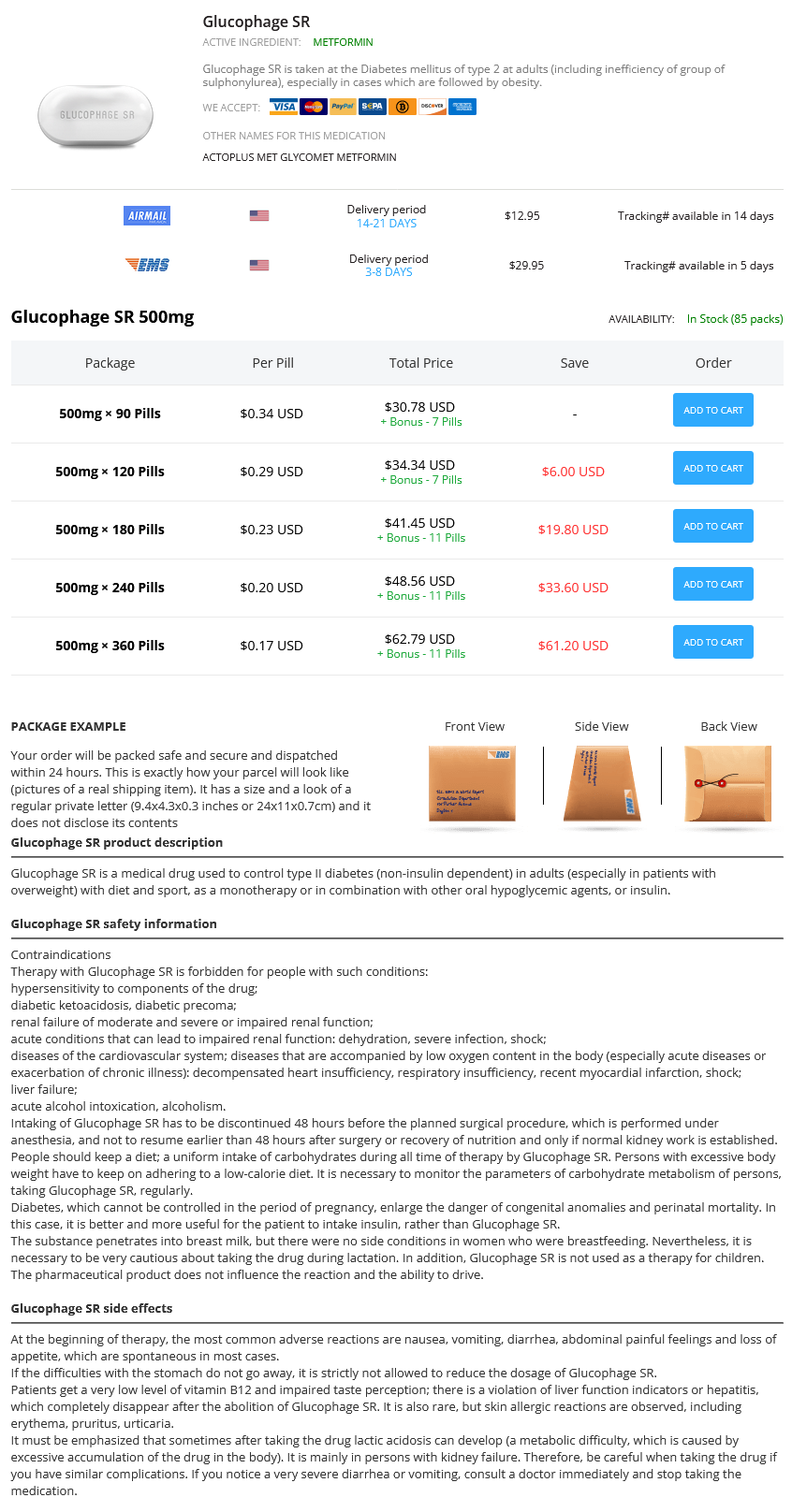
Glucophage SR Dosage and Price
Glucophage SR 500mg
- 90 pills - $30.78
- 120 pills - $34.34
- 180 pills - $41.45
- 240 pills - $48.56
- 360 pills - $62.79
Axial and coronal contrast-enhanced computed tomography images show classic striated nephrogram in the right kidney (A and B) with a solitary abscess medicine used to induce labor order glucophage sr with amex. Radiologic techniques have limited specificity in the diagnosis of various types of diffuse kidney parenchymal diseases because imaging features are overlapping in these pathologies. Nevertheless, there remains a growing clinical need for accurate, reproducible, and noninvasive measures of kidney function. Increased kidney cortical echogenicity may be useful in suggesting the presence of kidney parenchymal disease. It also provides quantitative measures of kidney function that may be applied to each kidney. Impaired transplant function on radionucleotide study is attributed to either obstruction of urine outflow or to other causes. No additional information can be obtained on nuclear medicine examinations to delineate among the causes of kidney failure. It may be used for preoperative imaging evaluation for both potential kidney donors and recipients. Comprehensive pretransplant evaluation of the kidney donor can be performed with assessment of kidney parenchymal, arterial, venous, and ureteric anatomy and measurement of differential kidney function. In posttransplant recipient evaluation, comprehensive structural and functional analysis can be performed. This modality can be useful in the evaluation of a number of posttransplant conditions, including: 1. Renal artery thrombosis or stenosis: Narrowing or abrupt cutoff in the main renal artery or its branch is seen in the angiographic phase. Segmental lack of perfusion in a renal artery territory can be depicted by functional imaging. Renal vein thrombosis: T2W images demonstrate thrombus as loss of patent dark vascular lumen. Hyperacute and accelerated acute rejection: Intrinsic graft dysfunction with ischemic microvascular injury manifests as striated nephrogram. Changes in the renal vascular compliance result in increased in vascular resistance. Ultrasound lacks ionizing radiation and may be used safely for follow-up longitudinal studies. Compare this appearance with the T2 signal and corticomedullary differentiation of a normal transplant kidney (B). The abnormal graft kidney demonstrated surrounding edema on axial T2W fat-saturated images (C, arrow), and dynamic postcontrast functional imaging (D) demonstrated overall reduced perfusion of the transplant kidney. The transplant edema and reduction in perfusion is a pattern that has been seen in acute rejection. Quantitative functional analysis (E) showed marked decreased function of the transplant kidney, and subsequent graft biopsy confirmed acute cellular rejection. Chronic rejection: Loss of kidney corticomedullary differentiation on T2 and T1W images is seen. An understanding of iodinated and gadolinium-chelate-based contrast agents is imperative. Short- and long-term outcomes of percutaneous transluminal angioplasty/stenting of renal fibromuscular dysplasia over a ten-year period. Randomized trials in angioplasty and stenting of the renal artery: tabular review of the literature and critical analysis of their results. Individual kidney blood flow measured by contrast enhanced magnetic resonance first-pass perfusion imaging. Comparative accuracy of renal duplex sonographic parameters in the diagnosis of renal artery stenosis: paired and unpaired analysis. Verbalis the incidence of hyponatremia depends on the patient population screened and the criteria used to define the disorder. Hospital incidences of 15% to 22% are common if hyponatremia is defined as any serum sodium concentration ([Na+]) of less than 135 mmol/L, but in most studies only 1% to 4% of patients have a serum [Na+] lower than 130 mmol/L, and fewer than 1% have a value lower than 120 mmol/L. Multiple studies have confirmed prevalence ranging from 7% in ambulatory populations up to 38% in acutely hospitalized patients. Older individuals are particularly susceptible to hyponatremia, with reported incidence as high as 53% among institutionalized geriatric patients. Although most cases are mild, hyponatremia is important clinically because (1) acute severe hyponatremia can cause substantial morbidity and mortality; (2) mild hyponatremia can progress to more dangerous levels during management of other disorders; (3) general mortality is higher in hyponatremic patients across a wide range of underlying co-morbidities; and (4) overly rapid correction of chronic hyponatremia can produce severe neurologic complications and death. Plasma osmolality (Posm) can be measured directly by osmometry and is expressed as milliosmoles per kilogram of water (mOsm/kg H2O). However, total osmolality is not always equivalent to effective osmolality, which is sometimes referred to as the tonicity of the plasma. Only the concentration of effective solutes in plasma should be used to determine whether clinically significant hypoosmolality is present. Hyponatremia and hypoosmolality are usually synonymous, with two important exceptions. First, pseudohyponatremia can be produced by marked elevation of serum lipids or proteins. In such cases, the concentration of Na+ per liter of serum water is unchanged, but the concentration of Na+ per liter of serum is artifactually decreased because of the increased relative proportion occupied by lipid or protein. Although measurement of serum or plasma [Na+] by ion-specific electrodes, currently used by most clinical laboratories, is less influenced by high concentrations of lipids or proteins than is measurement of serum [Na+] by flame photometry, such errors nonetheless can still occur when serum samples are diluted before measurement in autoanalyzers.