General Information about Fosamax
Fosamax is also used to treat glucocorticoid-induced osteoporosis. Glucocorticoids, also known as steroids, are used to deal with various medical conditions such as bronchial asthma, rheumatoid arthritis, and lupus. However, extended use of these drugs may find yourself in bone loss. Fosamax helps improve bone density in people taking steroids, reducing their risk of osteoporosis.
Fosamax comes in two types – a pill and an oral solution. The tablet is usually taken as soon as per week, whereas the oral solution is taken once a day. It is recommended to take Fosamax on an empty abdomen in the morning with a full glass of water. It is essential to follow the dosing instructions offered by your doctor rigorously. This treatment should be taken consistently to get the most effective outcomes.
One of the commonest causes of osteoporosis in ladies is menopause. During this stage, the physique produces less estrogen, a hormone that helps maintain bone density. This lower in estrogen leads to bone loss, making postmenopausal girls extra prone to osteoporosis. Fosamax has been proven to be effective in stopping and treating osteoporosis in postmenopausal ladies.
Fosamax, additionally known by its generic name alendronate, is a prescription medication that belongs to a category of medication known as bisphosphonates. It is used to treat and stop osteoporosis in both men and women. Fosamax works by slowing down the breakdown of bone and rising bone density, thus decreasing the risk of fractures.
Osteoporosis is a standard situation that impacts tens of millions of individuals, particularly girls after menopause. It is characterised by low bone density, making bones weaker and more prone to fractures. In the United States alone, over 10 million folks have osteoporosis, and virtually 80% of them are ladies. To fight this situation, a number of medicines have been developed, and one such drug is Fosamax.
Another condition that Fosamax is used to deal with is Paget's illness of bone. This is a continual condition where there may be irregular bone development, leading to weak bones that are extra vulnerable to fractures. Fosamax helps regulate the bone progress, reducing the risk of fractures and enhancing bone power.
Fosamax just isn't appropriate for everybody, and certain medical situations can have an effect on its effectiveness. It is essential to tell your physician if you have any kidney illness, vitamin D deficiency, or are unable to sit or stand upright for no less than half-hour. Additionally, it isn't beneficial for pregnant or breastfeeding girls.
Like any medication, Fosamax additionally has its share of side effects. Some common side effects of Fosamax embody mild gastrointestinal signs such as nausea, indigestion, and diarrhea. In uncommon circumstances, it can lead to more extreme unwanted aspect effects, similar to jaw bone problems (osteonecrosis), esophageal ulcers, and irregular heartbeat. It is essential to tell your physician if you experience any of those symptoms while taking Fosamax.
In conclusion, Fosamax is a widely used medication for treating and preventing osteoporosis in both women and men. Its ability to extend bone density and scale back the chance of fractures has made it a popular selection among medical doctors and patients. However, it's important to observe the dosing directions rigorously and inform your doctor of any unwanted effects or medical circumstances before starting Fosamax. With correct use, Fosamax can help improve bone well being and high quality of life for these affected by osteoporosis.
Moreover, Fosamax is also accredited for use in men who have osteoporosis. Although males are less more doubtless to develop osteoporosis in comparability with women, they will still be affected. Fosamax has been proven to extend bone mass in men, making their bones stronger and fewer vulnerable to fractures.
B, Midsagittal T1-weighted magnetic resonance image reveals odontoid migration into the posterior fossa, with compression of the inferior ventral medulla menopause occurs when buy generic fosamax 35 mg on-line. There is atlantoaxial dislocation with fusion between the superior surface of the axis body and the lateral atlantal mass. D, Lateral craniocervical radiograph 6 months after transoral ventral decompression of the atlas and the odontoid process and dorsal occipitocervical fixation with loop instrumentation and rib graft. They found that 62% of these patients had inflammatory changes of the cervical spine, including 17% with atlantoaxial subluxation and 25% with atlantoaxial impaction. This affects the craniocervical junction in much the same way as ankylosing spondylitis. Cervical spine involvement was found in 75% of the group; 13 of 21 had ankylosing characteristics and 8 of 21 had inflammatory characteristics. More recently, Quiero and colleagues117 reviewed a series of 70 patients with psoriatic spondyloarthropathy. They found that 41% of these patients manifested involvement of the cervical spine, but only one patient had atlantoaxial subluxation. Laiho and Kauppi118 reviewed the cervical spine radiographs of 65 patients with psoriatic arthritis and identified 12 patients with cervical spine involvement. Of these 12 patients, 5 had atlantoaxial subluxation and 3 demonstrated atlantoaxial impaction. The relationship between inflammatory bowel disease and craniocervical disease has not often been addressed in the literature. In 1986, Jordan and coworkers99 claimed the first description of a case in which inflammatory bowel disease was associated with atlantoaxial instability. The arthropathy may be acute and is sometimes associated with reactive arthritis; as a result of the synovitis, atlantoaxial subluxation may occur. The mass is ventral to the cervicomedullary junction in the retro-odontoid region. C, Axial computed tomography scan through the plane of the odontoid process and the atlas. They can be approached via the transoral route to halt or reverse the progression to neurological deterioration. Gross total resection was achieved in all cases, primarily via a transoral-transpalatopharyngeal approach. Seventy-six percent of the patients also underwent dorsal occipitocervical fusion. With a mean follow-up of 15 months, 86% of the patients demonstrated improvement or resolution of symptoms. Vertical translocation: the enigma of the disappearing interval in patients with myelopathy and rheumatoid arthritis. Calcium pyrophosphate dihydrate crystal deposition in the craniovertebral junction. Anatomy and biomechanics of normal craniovertebral junction (a) and biomechanics of stabilization (b). Mechanisms of disease: the molecular and cellular basis of joint destruction in rheumatoid arthritis. Combination drug therapy retards the development of rheumatoid atlantoaxial subluxations. A prospective study of the progression of rheumatoid arthritis of the cervical spine. Cervical spine surgery in patients with rheumatoid arthritis: long-term mortality and its determinants. Shah n Paul Santiago Knowledge of normal embryologic development is required to understand the various congenital abnormalities affecting the thoracic and lumbar spine. These abnormalities arise from failure of the normal progression of spinal development. The principal congenital pathologies presenting in adulthood include congenital kyphosis, scoliosis, lordosis, sacral dysgenesis, and closed spinal dysraphism (spina bifida occulta). Open neural tube defects are evident at birth and are beyond the scope of this chapter. The seven causes of closed or occult spinal dysraphism are lipomyelomeningocele, fatty filum terminale, split cord malformations, "meningocele manqué," dermal sinus tract, and neurenteric and dermoid cysts. In this chapter, we review spinal embryology with specific emphasis upon the points of the embryogenesis where errors lead to congenital anomalies. After this review, we discuss the management of congenital spinal abnormalities, including closed spinal dysraphism. However, the utility, safety, and widespread availability of this imaging modality should be considered. At our institution, weight-bearing standing long-cassette scoliosis films are used preoperatively to assess three-plane balance with gravitational load. In the setting of spondylolisthesis, flexion-extension standing films are routinely obtained for assessment of dynamic instability. Spinal dysraphism is seen in 20 of every 100,000 births in the United States and higher in offspring of affected parents. In one series, up to 61% of patients with congenital spine disease had another system involved. Oskovian and associates and Macewen and colleagues found 18% of their congenital scoliosis patients to have urologic abnormalities.
Rarely, seizures occur in the post-treatment period, usually in patients with supratentorial lesions and in those with a history of seizure disorders 1st menstrual cycle buy fosamax 35 mg cheap. Overall, radiosurgery does not appear to significantly alter the seizure threshold in patients with intracranial disease. The onset of these changes occurred 3 to 15 months after treatment in the majority of patients (92%) and more than 26 months after treatment in 8%. The clinical manifestations included headache, symptoms of raised intracranial pressure, and focal neurological deficits. In a small percentage of patients, it is associated with focal damage to neural tissue. Neurological deficits were still present at the time of the last follow-up in 3% of patients. The 7-year actuarial rate for the development of persistent symptomatic radiation-induced changes was 5. These changes presumably represent a whole gamut of pathologic processes ranging from gliosis to true necrosis. Radiation-Induced Neoplasia Cahan and associates defined the criteria for a tumor to be considered a result of irradiation: (1) the tumor must occur in the irradiation field; (2) it cannot be present before irradiation; (3) any primary tumor must differ histologically from the induced tumor; and (4) there must be no genetic predisposition for the occurrence of a secondary malignancy or tumor progression. With a group of 5000 patients and more than 30,000 patient-years of data, 1 patient was found to have new malignant brain tumors. A subset of 288 patients in this group underwent neuroimaging and participated in clinical follow-up for at least 10 years. Each of the patients was found to have an incidental, uniformly enhancing, dura-based mass lesion. From our series, if we conservatively estimate the radiosurgery-induced lesions that would be evident within a 10-year interval, our incidence of radiosurgeryinduced neoplasia would 2 in 2880 person-years or 69 in 100,000 person-years. Therefore, even though the risk for radiosurgery-induced secondary tumors is low, it must be weighed in the treatment of pediatric patients and in those with benign tumors and a long life expectancy. Cranial Nerves the mechanism of radiation injury to cranial nerves is most probably secondary to damage to small vessels and protective Schwann cells or oligodendroglia. There is a difference in tolerance of the various cranial nerves, with sensory nerves (optic and acoustic nerves) tolerating the least radiation and nerves in the parasellar region, the facial nerves, and the lower cranial nerves tolerating higher doses. This may be due to the fact that both the optic and acoustic nerves are actually fiber tracts of the central nervous system and carry more complex data. Clinical experience suggests that these specialized sensory nerves typically do not have the capacity to recover fully from injury. The radiosensitivity of cranial nerves often necessitates limits on the doses given to tumors in close proximity to these structures. Although the precise dose tolerance of cranial nerves is unclear, the anterior visual pathways seem to be the least radioresistant to single doses above 8 Gy. Small volumes of the optic pathways, however, can probably tolerate doses higher than 8 Gy in a single session. The distance between the nerve and the lesion being treated should be assessed carefully. A distance of 5 mm between the tumor and the optic apparatus is desirable to achieve optimal dose falloff, but occasionally a distance as little as 2 mm may be acceptable because of the shielding capabilities of the Gamma Knife. The tolerable distance is a function of the degree to which a dose plan can be designed to deliver a suitable radiation dose to the tumor and yet spare the optic apparatus. The largest experience on the radiation tolerance of cranial nerves comes from radiosurgical studies on the trigeminal and facial nerves. In our series of 151 patients who underwent radiosurgery for trigeminal neuralgia, 12 patients (8%) had new-onset facial numbness after treatment. The conclusion of this study was that doses up to 40 Gy are relatively safe for nerves in the parasellar region. The clinical effectiveness of radiosurgery is not fully explained by the linear quadratic model. The medical physics fundamentals related to the delivery of radiosurgery are more complicated than conventional fractionation algorithms. Through refinements in our understanding of the radiobiology of radiosurgery and advances in medical physics, the application of radiosurgery for central nervous system pathologies has expanded and the safety profile has improved. The application of the linear-quadratic dose-effect equation to fractionated and protracted radiotherapy. Use of normalized total dose to represent the biological effect of fractionated radiotherapy. Radiological aspects of gamma knife radiosurgery for arteriovenous malformations and other non-tumoural disorders of the brain. Cerebral radiation surgery using moving field irradiation at a linear accelerator facility. In contrast, metastatic tumors to the brain are a commonly encountered clinical situation, but patients have even poorer outcomes than those with primary brain tumors. Estimated rates depend on whether the incidence is calculated from autopsy data, clinical studies, tumor registries, hospital records, or other sources. Lung cancer accounts for approximately half of all secondary tumors to the brain; other primary tumors commonly causing brain metastases include breast cancer and melanoma. In terms of disease-specific risk, melanoma has the greatest likelihood of metastasizing to the brain. The overall incidence of brain metastases is probably increasing because of the combination of better diagnostic techniques and small gains in systemic therapy. Improved systemic therapeutic options have altered the conventional disease course such that patients with primary cancers live longer. With longer survival, asymptomatic micrometastatic disease in the brain is more likely to become overt, thereby inflating the incidence of the problem. Furthermore, the brain has traditionally been thought to represent a sanctuary site by not permitting penetration of most cytotoxic chemotherapeutic agents when the blood-brain barrier is intact.
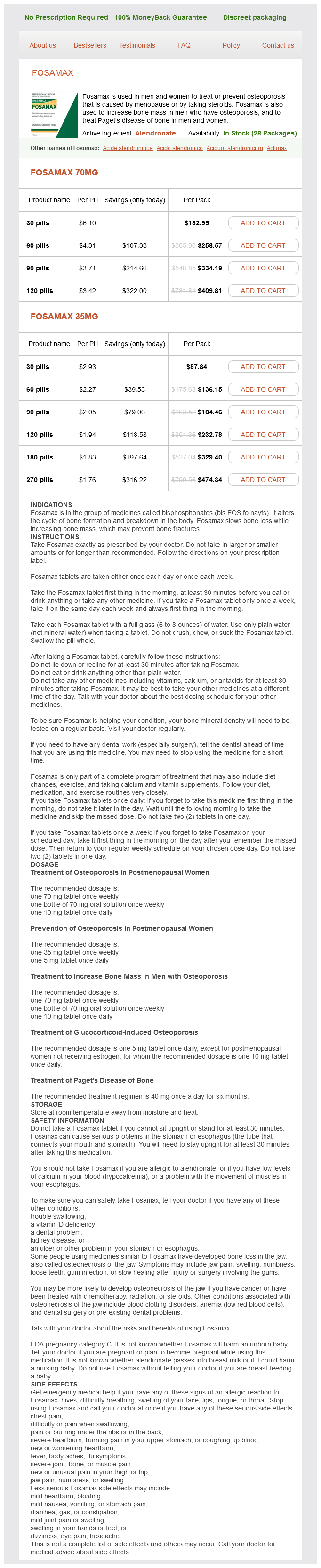
Fosamax Dosage and Price
Fosamax 70mg
- 30 pills - $182.95
- 60 pills - $258.57
- 90 pills - $334.19
- 120 pills - $409.81
Fosamax 35mg
- 30 pills - $87.84
- 60 pills - $136.15
- 90 pills - $184.46
- 120 pills - $232.78
- 180 pills - $329.40
- 270 pills - $474.34
The more commonly used 12- and 15-mm drill bits, taps, and screws are color-coded (blue and gold, respectively) to simplify use of the system breast cancer zip up fleece jacket buy generic fosamax 70 mg online. However, a wide range of screw lengths is available and can be inserted using the available variable depth drill guide and taps. The recommended screw placement is 10 degrees medially and parallel to the orientation of the adjacent disk space in the sagittal plane. The recommended plate length is from the rostral subchondral region of the most rostral vertebral body to the caudal subchondral region of the most caudal vertebral body included in the fusion construct. The system includes specific drill guides that either lock in a fixed position in the plate screw hole (12 degrees divergent in sagittal plane, 6 degrees medially convergent) or allow variable angulation through an arc of approximately 31 degrees relative to the axis of the screw hole. The diameter of the holding pin available for hands-off stabilization of the plate during drilling is small enough that an anchoring screw can ultimately be passed along its track. The option of fixed or variable screw trajectories within any one plate-hole site enables the production of constrained, nonconstrained, or hybrid biomechanical constructs based on the underlying pathology of the vertebral column. Similar to the Codman system, extremes in screw angulation can result in an incomplete interface between the anchor screw and locking mechanism. At the time of screw insertion, it is important to make certain that the locking washer remains above the level of the fixation screw head. Due to its mobility while in an unlocked position, the locking washer can be caught under the head of the anchor screw as the latter is advanced into the vertebral body. The anchor screw would then be prevented from fully seating within its plate hole, and locking the pair of anchor screws to the plate would be precluded. The Atlantis plate is manufactured with all of the locking screws in the open, elevated position. Before the wound is closed, all locking screws should be recessed to minimize the profile of the fixation construct. The screw head consists of five compressible petals that snap into the plate slot and prevent the screw from backing out. Although the angle between the screw head and plate is fixed (constrained), the screws can migrate vertically within their slots. This capacity to maintain axial loading despite graft subsidence permits load sharing by minimizing the presence of stress shielding and promotes fusion. The system design allows angulation of ±30 degrees in the vertical axis and ±8 degrees medially and laterally in the coronal axis. Theslottedconfiguration promotes load sharing by allowing vertical settling of the fixationconstruct. In other words, 50% of the screw slot should overlap the graft and 50% should overlap the adjacent vertebral body. To further accommodate settling, the individual screws should be positioned at the most distal aspect of their respective slots. These positions should correspond to an entry site at the most caudal end of the rostral vertebral body and the rostral end of the most caudal vertebral body. Complications the risks related to screw-plate stabilization of the cervical spine include all risks intrinsic to a routine anterior cervical discectomy and fusion procedure52,53: injuries to vertebral and carotid Atlantis Translational System An example of translational plates is the new Atlantis Translational system, which became available in 2007. The plate features fixed and variable angle screws allowing constrained, nonconstrained, or hybrid biomechanical constructs. The intention of this new plate is to maintain constant graft compression throughout the range of motion of the cervical spine by allowing unidirectional translation up to 2 mm per level in 1-mm increments. Unlike bidirectional translational plates that allow graft unloading during extension, unidirectional translational plates maintain constant graft loading even during extension. In addition, this plate allows in situ compression of the plate to maintain active compression of the interbody graft. This feature could be particularly helpful for the treatment of traumatic distraction injuries. The plate can be compressed up to 2 mm per level using a plate compressor that fits in the locking mechanism. Compared with all the systems discussed previously, it features one column of screws instead of two columns with one screw hole per vertebral body level. It is available with two or three screw holes and thus can be applied after a one- or two-level anterior cervical discectomy and fusion. As experience with anterior cervical plating systems has increased, the differences in operative time between procedures that incorporate plating and those that do not continue to narrow. Later generations of screw-plate systems have become progressively easier to insert, offering the convenience of unicortical bone screw purchase, an integrated locking mechanism to prevent retropulsion of the anchoring screws, and self-tapping screws. Anterior cervical plates are an integral method of treatment for the diseased cervical spine. Anterior cervical interbody fusion using autogeneic and allogeneic bone graft substrate: a prospective comparative analysis. Anterior cervical fixation: analysis of load-sharing and stability with use of static and dynamic plates. Surgical anatomy of the anterior cervical spine: the disc space, vertebral artery, and associated bony structures. Three-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. The safety and efficacy of anterior cervical discectomy and fusion with polyetheretherketone spacer and recombinant human bone morphogenetic protein-2: a review of 200 patients. Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. The development of pseudarthrosis (fibrous union) and instrumentation failure are intimately related. The primary occurrence of either can result directly in the other and necessitate revision of the entire fusion and fixation construct. Alternatively, successful arthrodesis can develop in the presence of failed instrumentation,54,55 thus illustrating the race between bony healing and implant fatigue.