General Information about Fluvoxamine
Fluvoxamine should not be taken with different medicines that improve serotonin ranges, such as certain antidepressants and migraine medications, as this could result in a uncommon but serious condition referred to as serotonin syndrome. It is essential to consult with a healthcare professional before beginning Fluvoxamine to make certain that it's safe so that you just can take.
In Conclusion
The burden of Obsessive Compulsive Disorder (OCD) is usually overlooked, with many individuals assuming it is just a little quirk or an eccentricity. However, for those living with OCD, it is a debilitating and life-changing dysfunction. Obsessive Compulsive Disorder is a mental well being condition characterised by obsessive thoughts and compulsive behaviors that may eat a sufferer's life. It impacts approximately 1 in each 40 adults and might manifest in a variety of signs, similar to extreme hand washing, counting, or checking behaviors.
While OCD has been studied for many years, the understanding and remedy of this disorder have been repeatedly evolving. One of probably the most revolutionary treatments for OCD is Fluvoxamine, a selective serotonin reuptake inhibitor (SSRI) that is proving to be an efficient medication for patients suffering from this debilitating disorder.
Fluvoxamine: The Science Behind It
Several medical trials have been carried out to evaluate the effectiveness of Fluvoxamine in treating OCD. In one research, 104 sufferers with OCD have been randomly assigned both to take Fluvoxamine or a placebo for eight weeks. The outcomes confirmed that 75% of the sufferers who took Fluvoxamine had a significant reduction of their signs, in comparability with solely 33% of those that took the placebo.
Side Effects and Precautions
Clinical Trials and Efficacy of Fluvoxamine
Fluvoxamine was first developed within the Nineteen Sixties, but it wasn't till the Nineteen Eighties that it was tested for its effectiveness in treating OCD. Its major mechanism of action is by selectively inhibiting the reuptake of serotonin in the brain, which outcomes in elevated levels of this neurotransmitter. Serotonin performs an important function in regulating mood, emotions, and habits, making it a possible goal for treating psychological health circumstances corresponding to OCD.
Benefits of Fluvoxamine Over Other Treatments
Obsessive Compulsive Disorder can considerably impair one's high quality of life, and for many sufferers, finding the best remedy could be a irritating and difficult journey. However, with the introduction of Fluvoxamine, there is hope for those living with OCD. This groundbreaking treatment has been proven to be effective in decreasing the symptoms of OCD and has the advantage of getting fewer unwanted facet effects compared to different remedies. If you or somebody you realize is struggling with OCD, converse to a healthcare skilled in regards to the potential benefits of Fluvoxamine and how it could be the necessary thing to regaining management of your life.
Like any medication, Fluvoxamine can have unwanted facet effects, together with nausea, diarrhea, dizziness, and insomnia. However, these unwanted facet effects are often gentle and sometimes dissipate inside the first few weeks of remedy. In some instances, Fluvoxamine could trigger elevated anxiety or agitation, but this is rare and might normally be resolved by adjusting the dosage.
While different SSRIs have also been discovered to be effective in treating OCD, research have shown that Fluvoxamine has certain advantages over them. For instance, Fluvoxamine has been discovered to have a faster onset of action, which means that patients can experience enchancment of their signs before with different drugs. Additionally, Fluvoxamine has fewer unwanted effects in comparability with different SSRIs, making it a greater option for sufferers who may be sensitive to these type of medications.
Another study in contrast Fluvoxamine to another commonly used antidepressant, clomipramine, in the therapy of OCD. The results showed that each medicines were efficient in lowering OCD signs, however Fluvoxamine had fewer unwanted aspect effects, making it a preferable option for sufferers.
Fluvoxamine: The Revolutionary Treatment for Obsessive Compulsive Disorder (OCD)
Randomized trials have shown that efficacy of aromatase inhibitors is similar or superior to that of tamoxifen and that these drugs have an acceptable side-effect profile anxiety symptoms 3 days fluvoxamine 100 mg buy line. Multiple trials have compared monotherapy with tamoxifen, an aromatase inhibitor, A10 or sequential therapy; in aggregate, they suggest that the use of an aromatase inhibitor at some point should be considered for most postmenopausal women with steroid receptorpositive invasive breast cancer. A patient-level meta-analysis of randomized trials in postmenopausal women with estrogen receptorpositive early breast cancer showed that aromatase inhibitors reduce recurrence rates by about 30% (proportionately) compared with tamoxifen while treatments differ, but not thereafter. A11 Side effects include postmenopausal symptoms, osteoporosis and fractures, and arthralgias. Aromatase inhibitors are not useful for receptor-negative breast cancer, nor should they be used as monotherapy in premenopausal women or men with breast cancer. The simultaneous administration of tamoxifen plus aromatase inhibitor does not improve outcome over aromatase inhibitor alone. Direct evidence suggests that at least 5 years of adjuvant endocrine therapy is associated with better outcomes than shorter periods. Information from randomized trials about longer duration of aromatase inhibitors is beginning to emerge and suggests that the greatest benefit of longer term therapy is prevention of contralateral breast cancer. A12 Increased understanding of growth and death pathways of breast cancer led to the identification of critical nonendocrine pathways that are potential targets for therapy. More recent trials suggest that 1 year of therapy is better than 6 months and 2 years is no better than 1 year. Because a large randomized trial showed that concurrent chemotherapy plus tamoxifen led to worse outcome than chemotherapy followed by tamoxifen, most practitioners delay the administration of endocrine therapy until after completion of chemotherapy. Conversely, the benefit of trastuzumab appears to be greater when it is coadministered with taxane chemotherapy rather than following completion of taxane. A randomized trial showed no clear difference between the sequence of chemotherapy followed by radiotherapy compared with radiotherapy followed by chemotherapy. A number of trials have tested the concept that administration of systemic therapy before primary surgery would improve outcome over the standard sequence of surgery followed by systemic therapy. Together they suggest that, compared with adjuvant therapy, preoperative (also termed neoadjuvant) systemic therapy improves the rate of breast conservation but does not enhance disease-free or overall survival. The possibility that preoperative therapy can provide an in vivo assessment of tumor response to therapy is suggested by the correlation between the finding of a pathologic complete response (absence of invasive cancer in the surgical specimen) and long-term disease-free survival in some studies. Follow-Up of Early-Stage Breast Cancer Survivors adjuvant anti-Her2 therapy A critical question is how longitudinal medical follow-up should be conducted in women who have received appropriate local and systemic therapy for early breast cancer. Randomized trials have addressed the question of the value of serial laboratory and radiology testing, as well as the role of primary care versus oncology specialist follow-up. On the basis of these and other studies, the American Society of Clinical Oncology has published evidence-based guidelines for follow-up of asymptomatic survivors of early-stage breast cancer. It is characterized by large primary tumor, fixed tumor or lymph nodes, or neoplastic invasion of the skin or chest wall. It has a clinical presentation of breast swelling, warmth, and erythema and may or may not be associated with a mass. Breast cancer follow-up and management after primary treatment: American Society of Clinical Oncology clinical practice guideline update. The limited examination should include an assessment of nodes, axillae, lumpectomy or mastectomy site, contralateral breast, chest, and abdomen. Diagnosis is usually established by fine-needle aspiration or core biopsy, and combined-modality therapy is used to maximize control of local disease and distant micrometastases. Several months of preoperative endocrine therapy or chemotherapy results in tumor regression in most patients, thereby allowing definitive breast surgery of some type to be performed. Multimodality therapy results in a 5-year disease-free survival rate of approximately 50%. Endocrine therapy is preferred as the first intervention for metastatic breast cancer whenever feasible because of its favorable therapeutic index. Factors that support the use of endocrine therapy include the expression of hormone receptors, a long disease-free interval, and absence of symptoms or visceral disease. More than half of the women who meet these criteria respond to an initial course of hormone therapy, with a median response duration of 9 to 12 months. Length of response is a good predictor for the likelihood of response to a second course of endocrine therapy when the first agent fails. A second course of endocrine therapy is less likely to be successful, and the duration of response is shorter; again, duration of response predicts for likelihood of success with third-line therapy. Successful application of this algorithm can result in good disease control with little toxicity for several years in some women. Selection is usually made on the basis of efficacy, toxicity, and menopausal status. Serial administration of agents is the norm, although one study in estrogen receptorpositive postmenopausal metastatic breast cancer showed that the combination of the aromatase inhibitor anastrozole with fulvestrant was superior to anastrozole alone or sequential anastrozole and fulvestrant. A15 Other combination therapies (with the possible exception of ovarian suppression plus tamoxifen) do not improve outcomes. Inhibitors of cyclin-dependent kinases 4 and 6, which promote progression from the G1 phase to the S phase of the cell cycle, are now commonly used with endocrine therapy to improve outcomes. Finally, recent work has also demonstrated the value of everolimus, but not temsirolimus, combined with an aromatase inhibitor to improve progressionfree survival compared with an aromatase inhibitor alone in patients with hormone receptorpositive advanced breast cancer previously treated with nonsteroidal aromatase inhibitors. A16 Several months of therapy are needed before the efficacy of a newly introduced endocrine therapy can be assessed. Patients and clinicians should be aware of the possibility of treatment-related tumor flare-a syndrome of worsening symptoms and increased circulating tumor markers-that can occur within the first few weeks of treatment.
Other Drugs Potassium iodide transiently inhibits the synthesis and release of thyroid hormone from the gland and is rarely used to accelerate recovery after radioactive iodine treatment anxiety symptoms menopause buy generic fluvoxamine 100 mg on-line, to prepare patients for thyroidectomy, and to augment other treatments used to control severe thyrotoxicosis (see later). It can also temporarily control hyperthyroidism if severe allergies preclude the use of other medications. Surgery Antithyroid Drugs Methimazole, carbimazole, and propylthiouracil inhibit thyroid hormone biosynthesis by competitively inhibiting iodine organification and iodotyrosine coupling. Propylthiouracil, but not methimazole or carbimazole, inhibits the conversion of T4 to T3 in peripheral tissues. These agents are used for the treatment of thyrotoxicosis caused by overproduction of thyroid hormones. Because the thionamides block only new thyroid hormone synthesis, glandular stores of preexisting thyroid hormone must be exhausted before they are fully In the United States total thyroidectomy is seldom recommended for hyperthyroid Graves disease, except when radioiodine therapy is contraindicated, when malignancy is suspected in a thyroid nodule, or when concomitant hyperparathyroidism also requires surgical intervention. It may be first-line therapy, however, if a woman with Graves disease wishes to become pregnant and avoid taking antithyroid drugs during pregnancy. Thyroidectomy is the treatment of choice for toxic multinodular goiters that cause cosmetic disfigurement or compressive symptoms. In more severe cases, high-dose systemic glucocorticoid therapy can sufficiently diminish orbital inflammation so that orbital irradiation, which was recommended in the past, does not have added benefit. A5 Teprotumumab, a humanized monoclonal antibody that inhibits the insulin-like growth factor-I receptor, also reduces proptosis in active ophthalmopathy. A6 Orbital decompression surgery may occasionally be required for persistent corneal complications, optic nerve compression, or cosmetic reasons. Infiltrative dermopathy may respond to topical glucocorticoids, but intradermal or systemic glucocorticoids, long-acting somatostatin analogues, and surgery have been tried for advanced disease. In pregnant patients, Graves disease is almost always the underlying cause of the hyperthyroidism. If hyperthyroidism is confirmed, -blockers should be used only transiently for severe symptoms. Propylthiouracil can cause congenital malformations but is the preferred medication for the first trimester because methimazole has been linked to more severe birth defects. However, methimazole is preferred after the first trimester because of its better side-effect profile. If Graves disease has been well controlled on low-dose methimazole, it can be discontinued with careful monitoring prior to conception with the goal of avoiding its use during pregnancy. Because Graves disease often remits in late pregnancy, the dose of the antithyroid drug often can be reduced. Laboratory Findings Laboratory testing initially shows evidence of overt thyrotoxicosis, with T4 levels proportionately higher than T3 levels. On scanning, the fractional radioiodine uptake typically is less than 2% at 24 hours (see Table 213-6). Transient symptoms of thyrotoxicosis will respond after 1 to 3 weeks of -blocker treatment. Subsequent symptomatic hypothyroidism may require short-term thyroxine, but long-term thyroid hormone replacement usually is not required. Silent Thyroiditis Silent thyroiditis (also known as painless or lymphocytic thyroiditis) occurs more commonly in women than men, with a peak age of incidence at ages 30 to 40 years. This painless inflammation of the thyroid gland is characterized by diffuse lymphocytic infiltration. Based on this finding and the presence of thyroid peroxidase antibodies in about 50% of patients, this condition is believed to be autoimmune. Silent thyroiditis typically follows the same triphasic course as subacute thyroiditis, with transient thyrotoxicosis followed by transient hypothyroidism and eventual return to euthyroidism. The thyrotoxic phase may be less frequently recognized than the hypothyroid phase. Each of these phases of thyroid dysfunction can have a variable duration of weeks to months. The diagnosis of silent thyroiditis may be suspected when a patient presents with symptoms of hypothyroidism that were preceded by symptoms of hyperthyroidism. The thyroid gland is either normal in size or modestly enlarged and is not tender. The fractional uptake of radioiodine is very low or absent during the thyrotoxic phase and then returns to normal as the gland recovers (see Table 213-6). Clinical findings include fever, atrial tachyarrhythmias, heart failure, nausea, vomiting, diarrhea, and seizures. Treatment should include acetaminophen, external cooling, -blockers, thionamides, potassium iodide, and glucocorticoids, as well as rapid evaluation and aggressive management of any underlying medical problems. Addition of bile acid sequestrants can lower free T4 levels faster than antithyroid drugs alone. Salicylates are contraindicated because they can increase serum levels of free T4 and T3 by displacing thyroid hormones from thyroid binding proteins. Plasmapheresis has also been used in critically ill patients not responding to traditional pharmacologic therapies. Hypothyroidism then ensues for about one month, after which normal thyroid function returns in most patients. Patients usually have pain that is localized to the thyroid gland, but pain can radiate to the throat, ears, or jaw.
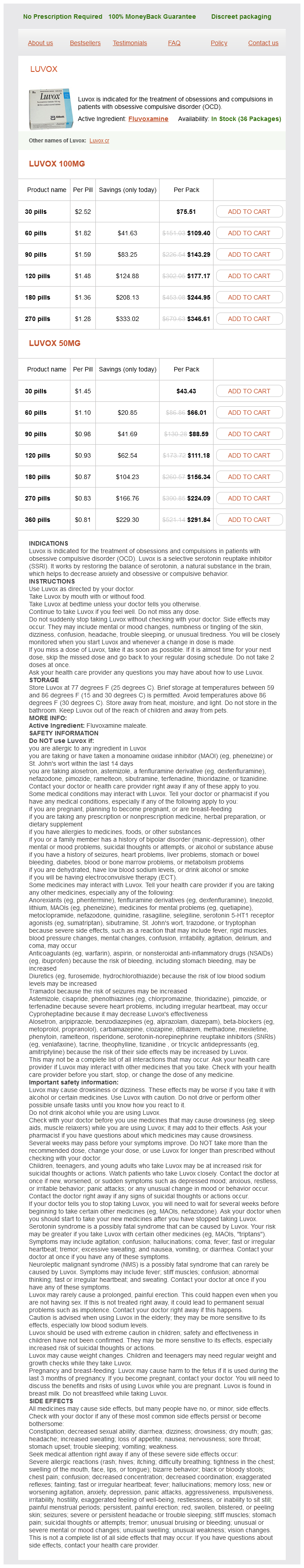
Fluvoxamine Dosage and Price
Luvox 100mg
- 30 pills - $75.51
- 60 pills - $109.40
- 90 pills - $143.29
- 120 pills - $177.17
- 180 pills - $244.95
- 270 pills - $346.61
Luvox 50mg
- 30 pills - $43.43
- 60 pills - $66.01
- 90 pills - $88.59
- 120 pills - $111.18
- 180 pills - $156.34
- 270 pills - $224.09
- 360 pills - $291.84
Specialized binding proteins for cortisol anxiety poems purchase fluvoxamine with a visa, androgens, estrogens, and thyroid hormones are selective for their cognate hormone. The free circulating hormone concentration is only a small fraction of the total hormone measured by routine analytic methods. Binding protein abnormalities can occur in liver disease because most are synthesized by the liver. Thus, the determination of free as opposed to total plasma hormone concentration may be critical to accurate diagnosis in certain clinical conditions. Even some peptide hormones such as angiotensin must undergo enzymatic conversion from secreted precursor form to generate the active hormone. The central question in hormone action is how a hormone circulating in the blood stream in minute concentrations recognizes its specific target cells and regulates physiologic processes within them. Research addressing this question over the past four decades defined receptors, previously a purely theoretical concept, in molecular terms. Receptors are highly selective molecules that bind their cognate hormones with high affinity and specificity. Hormones regulate cellular physiologic processes such as secretion of hormones, enzymes, and other compounds, muscle contraction, growth, and proliferation. Signal transduction is the general term for the biochemical steps between hormone binding to receptor and alterations in cell physiology. Cell surface receptors may generate "second messengers," which in turn regulate a kinase cascade. Receptor activation may have rapid effects such as exocytosis of secretory granules, but longer-term actions involving gene regulation may also be a consequence of second messenger and kinase cascade activation. Steroid and thyroid hormones and vitamin D bind to members of the nuclear receptor family. Left, glucocorticoid receptor family members bind as homodimers to palindromic dnA sites. Thyroid hormone receptor family members bind primarily as heterodimers with retinoid X receptor to direct repeat dnA sites separated by varying numbers of base pairs. Right, As a result of hormone binding, repressor complexes dissociate and activator complexes bind to nuclear receptors. Genetic endocrine diseases include those caused by mutations in one component of a signal transduction pathway leading either to hormone "resistance" or hormone-independent activation (Tables 209-1 and 209-2). In the former, subjects present with apparent hormone deficiency, but direct hormone measurement reveals high concentrations of bioactive hormone that fails to act owing to target organ resistance. In the latter, patients present with apparent endocrine hyperfunction, but direct measurement reveals suppressed hormone concentration due to intact negative feedback. Loss-of-function mutations in receptors and in signaling intermediates such as G proteins have been identified in patients with hormone resistance. The converse, mutations that constitutively activate receptors or downstream signaling components,7 have been identified in endocrine hyperactivity diseases such as familial male precocious puberty and familial nonautoimmune hyperthyroidism. Receptor inactivating mutations that lead to hormone-resistance diseases, such as the androgen receptor mutations responsible for varying degrees of testosterone insensitivity,8 have been identified for both the cell surface and nuclear classes of receptors. Mutations in genes encoding proteins such as corepressors that form part of the nuclear receptor complex may also cause hormone resistance. Peptidyl hormones of endocrine cells origin in the gut-their discovery and physiological relevance. Levels of glucose-regulatory hormones in patients with non-islet cell tumor hypoglycemia: including a review of the literature. D is incorrect because outputs other than hormones can exert negative feedback suppression. When activated, may exert their effects by directly regulating gene transcription D. Irrespective of starting location, always translocate to the nucleus to exert their actions E. Both B and C Answer: E Because there are cell surface receptors that do not translocate to exert their action and nuclear receptors for steroid hormones, A and D are incorrect. May be caused by loss-of-function mutations in genes encoding cell surface or nuclear receptors or other components of the signal transduction pathway E. Are generally associated with autoimmune disease Answer: D All the cited examples may be causes of inherited hormone resistance diseases, not just B. Cells dispersed throughout the lining of the small intestine and within the pancreas C. All of the above Answer: E Research has shown that not only classical endocrine glands such as the thyroid and adrenal, but also dispersed enteroendocrine cells in the gut lining and islets in the pancreas, neuroendocrine cells in the posterior pituitary, and nonclassical hormone-secreting sites such as kidney, heart, and adipose are all sources of hormone secretion. All of the above Answer: A A mutation in the hormone gene altering the signal sequence of a peptide hormone and thereby impairing its ability to be secreted may cause genetic forms of hormone deficiency such as hypoparathyroidism. The mechanism whereby an "output" regulated by a hormone feeds back to regulate the secretion of that hormone C. The most important environmental factors are temperature and light, which fluctuate in a predictable way each day. Humans have a circadian clock that makes sure that the physiology and behavior are attuned to the time of day. The nervous system senses temperature and light, and it uses them as clues to guide eating, activity, sleep, and other essential life functions. The neurohypophysial neurons originate from the paraventricular and supraoptic nuclei and traverse the hypothalamic-pituitary stalk to the posterior pituitary, where nerve endings release vasopressin and oxytocin. The blood supply of the median eminence comes from the superior hypophysial artery and its richly arborized capillary beds that extend into the median eminence and then coalesce to form the portal veins that traverse the pituitary stalk and terminate in the pituitary gland. The neuroendocrine system relies on a series of feedback loops, which regulate pituitary hormones as well as the levels of target organ hormones.