General Information about FML Forte
FML Forte is usually well-tolerated by most sufferers, however like several treatment, it could have unwanted effects. The most common side effects are gentle and embody stinging or burning sensation within the eye, temporary blurred imaginative and prescient, or discomfort. These unwanted effects are often temporary and may disappear as the body adjusts to the medication. In uncommon circumstances, some sufferers might expertise extra severe side effects corresponding to elevated stress within the eye or allergic reactions. If these occur, patients ought to seek medical consideration immediately.
One of the benefits of FML Forte is its quick onset of motion. The medicine can start relieving signs in as little as a number of hours, and important improvement may be seen inside a week of therapy. This fast-acting nature makes it a preferred alternative for sufferers who need instant aid from eye inflammation.
The energetic ingredient in FML Forte is fluorometholone, which belongs to a category of medicine known as corticosteroids. Corticosteroids are known for his or her anti-inflammatory properties, and when administered in eye drops, they can shortly relieve irritation and scale back discomfort. The medicine is available as an ophthalmic resolution, which implies it is just meant for use in the eyes.
FML Forte is prescribed by docs for quite so much of eye situations, and the dosage and frequency of use could range depending on the severity of the irritation. It is normally utilized to the eye two to 4 times a day, as directed by the doctor. The eye drops must be used persistently, and the full course of therapy must be completed even if signs enhance. A sudden stop in remedy can worsen the irritation, so you will want to observe the doctor's instructions.
It is essential to follow the instructions for utilizing FML Forte rigorously. Patients ought to avoid touching the tip of the bottle to the attention or any other surface to prevent contamination. It is also beneficial to scrub palms before and after use to avoid any potential infections. Patients who wear contact lenses should take away them earlier than making use of FML Forte and wait quarter-hour before reinserting them.
In conclusion, FML Forte is an effective treatment for treating eye inflammation. Its fast-acting nature and low danger of unwanted side effects make it a popular choice for medical doctors and patients alike. If you expertise any symptoms of eye inflammation, it is necessary to seek the assistance of a doctor for correct prognosis and treatment. With the utilization of FML Forte, sufferers can anticipate aid from eye inflammation and resume their daily actions with consolation and ease.
FML Forte, also called fluorometholone, is a corticosteroid eye drop commonly used for the remedy of eye irritation. It is a stronger model of FML, an older model of the same medicine. FML Forte is efficient in lowering swelling, heat, redness, and ache in the eyes and eyelids. This inflammatory response is usually caused by circumstances similar to conjunctivitis, uveitis, and keratitis.
These muscles are the effectors in the tympanic reflex allergy forecast jupiter fl purchase fml forte 5 ml without a prescription, which is elicited in about one-tenth of a second after a loud, external sound. As a result, the bridge of ossicles in the middle ear becomes more rigid, reducing its effectiveness in transferring vibrations to the inner ear. The tympanic reflex reduces pressure from loud sounds that might otherwise damage the hearing receptors. Ordinary vocal sounds also elicit the tympanic reflex, such as when a person speaks or sings. This action muffles the lower frequencies of such sounds, improving the hearing of higher frequencies, which are common in human vocal sounds. In addition, the tensor tympani muscle maintains tension on the tympanic membrane. This is important because a loose tympanic membrane would not be able to effectively transmit vibrations to the auditory ossicles. For this reason, the tympanic reflex cannot protect the hearing receptors from the effects of very sudden loud sounds, such as from an explosion or a gunshot. This tube allows air to pass between the tympanic cavity and the outside of the body by way of the throat (nasopharynx) and mouth. The function of the auditory tube becomes noticeable during rapid change in altitude. As a person descends from a high altitude, the air pressure on the outside of the tympanic membrane steadily increases. This may push the tympanic membrane inward, out of its normal position, impairing hearing. When the air pressure difference on the sides of the tympanic membrane is great enough, some air may force its way up through the auditory tube into the middle ear. This equalizes the pressure on both sides of the tympanic membrane, which moves back into its regular position, causing a popping sound as normal hearing returns. A reverse movement of air ordinarily occurs when a person ascends from a low altitude. The auditory tube is usually closed by valvelike flaps in the throat, which may inhibit air movements into the middle ear. Swallowing, yawning, or chewing aid in opening the flaps and can hasten equalization of air pressure. Signs of a middle ear infection (otitis media) in a toddler include irritability, fever, and tugging on the painful ear. Using an instrument called an otoscope reveals a red and bulging tympanic membrane. Inner (Internal) Ear the inner ear is a complex system of intercommunicating chambers and tubes called a labyrinth (labi-rinth). The bony (osseous) labyrinth is a cavity within the temporal bone; the membranous labyrinth is a tube that lies within the bony labyrinth and has a similar shape (fig. Between the bony and membranous labyrinths is a fluid called perilymph, secreted by cells in the wall of the bony labyrinth. The parts of the labyrinths include a cochlea (kokle-ah) that functions in hearing and three semicircular canals that provide a sense of equilibrium. A bony chamber called the vestibule, between the cochlea and the semicircular canals, houses membranous structures that serve both hearing and equilibrium. The cochlea is a tube shaped a bit like a snail shell, coiled around a bony core, the modiolus. A thin, bony shelf (spiral lamina) extends out from the core and coils around it within the tube (fig. A portion of the membranous labyrinth in the cochlea, called the cochlear duct (scala media), runs inside the tube opposite the spiral lamina, and together these structures divide the tube into upper and lower compartments. The upper compartment, called the scala vestibuli, leads from the oval window to the apex of the spiral. The lower compartment, the scala tympani, extends from the apex of the spiral to a membrane-covered opening in the wall of the inner ear facing the tympanic cavity, called the round window. These compartments form the bony labyrinth of the cochlea, and they are filled with perilymph. At the apex of the cochlea, beyond the tip of the cochlear duct, a small opening, the helicotrema, connects the perilymph in the upper and lower compartments and allows the fluid pressures in them to equalize (fig. The basilar membrane extends from the bony shelf of the cochlea and forms the floor of the cochlear duct. It has many thousands of elastic fibers and becomes thinner from the base of the cochlea to its apex. Vibrations entering the perilymph at the oval window travel along the scala vestibuli and pass through the vestibular membrane to enter the endolymph of the cochlear duct, where they move the basilar membrane. After passing through the basilar membrane, the vibrations enter the perilymph of the scala tympani, and movement of the membrane covering the round window dissipates their force into the air in the tympanic cavity (fig. The spiral organ (organ of Corti), which contains about 16,000 hearing receptor cells, is on the superior surface of the basilar membrane and stretches from the apex to the base of the cochlea. The receptor cells, called hair cells, are in four parallel rows, with many hairlike processes known as stereovilli (also called stereocilia) that extend into the endolymph of the cochlear duct. Above these hair cells is a tectorial membrane, attached to the bony shelf of the cochlea. It passes like a roof over the receptor cells, contacting the tips of their hairs (figs. Different frequencies of vibration move different regions along the length of the basilar membrane. A particular sound frequency bends the hairs of a specific group of receptor cells, activating them. If sound activates receptors at different places along the basilar membrane simultaneously, we hear multiple tones at the same time.
After age seventy allergy medicine congestion purchase generic fml forte canada, the pupil cannot dilate as well as it once did, halving the amount of light that can enter the eye. Glaucoma develops in the eyes as a person ages when the rate of aqueous humor formation exceeds the rate of its removal. As this pressure is transmitted to all parts of the eye, in time, the blood vessels that supply the receptor cells of the retina may squeeze shut, cutting off the nutrient and oxygen supply. Drugs, or traditional or laser surgery to promote the outflow of aqueous humor, can treat glaucoma if it is diagnosed early. However, because glaucoma in its early stages typically produces no symptoms, discovery of the condition usually depends on measuring the intraocular pressure using an instrument called a tonometer. Clear images cannot focus on the retina, and in time, the person may become blind. Removing the lens with a laser and replacing it with an artificial implant can treat cataract. In a form of age-related macular degeneration, and also in people with diabetes who develop diabetic retinopathy, tiny blood vessels extend into the macula, making images in the center of the visual field appear wavy. Despite these various problems, many older individuals continue to enjoy sharp, functional senses well into the upper decades of life. Receptor potentials are transferred to nerve fibers, triggering action potentials. Perception is when a particular part of the sensory cortex interprets the sensory stimulation. Projection occurs when the cerebral cortex interprets a sensation to come from the receptors being stimulated. Sensory adaptation is the adjustment of sensory receptors to continuous stimulation. The major types of receptors include: (1) Chemoreceptors, sensitive to changes in chemical concentration. Free nerve endings, common in epithelial tissues, are responsible for the sensation of itching. Lamellated corpuscles are the receptors for the sensations of heavy pressure and vibrations. Thermoreceptors include two sets of free nerve endings that are heat and cold receptors. Combinations of input from both receptor types are interpreted as intermediate temperatures. Pain receptors (1) Pain receptors are free nerve endings that tissue damage stimulates. Pain pathways (1) the two main types of pain fibers are acute pain fibers and chronic pain fibers. Regulation of pain impulses (1) Awareness of pain occurs when impulses reach the thalamus. Muscle spindles are stimulated when a muscle is relaxed, and they initiate a reflex that contracts the muscle. Golgi tendon organs are stimulated when muscle tension increases, and they initiate a reflex that relaxes the muscle. Olfactory receptors (1) Olfactory receptors are chemoreceptors that chemicals dissolved in nasal secretions stimulate. Olfactory organs (1) the olfactory organs consist of receptor cells and supporting cells in the nasal cavity. Olfactory stimulation (1) Olfactory impulses may result when an odorant molecule stimulates a distinct set of receptor cells. Taste sensations (1) the five primary taste sensations are sweet, sour, salty, bitter, and umami. Taste pathways (1) Sensory information from taste receptors travels on fibers of the facial, glossopharyngeal, and vagus nerves. The outer ear includes the auricle, the external acoustic meatus, and the tympanic membrane. It collects sound waves created by vibrating objects and transfers the vibrations to the middle ear. Middle ear (1) Auditory ossicles of the middle ear transfer sound waves from the tympanic membrane to the oval window of the inner ear. Auditory tubes connect the middle ears to the throat and help maintain equal air pressure on both sides of the tympanic membranes. Inner ear (1) the inner ear consists of a complex system of connected tubes and chambers-the bony labyrinth and the membranous labyrinth. Auditory pathways (1) the axons from hearing receptors are found in the cochlear branch of the vestibulocochlear nerves. Static equilibrium maintains the stability of the head and body when they are motionless. Dynamic equilibrium balances the head and body when they are suddenly moved or rotated. Other structures that help maintain equilibrium include the proprioceptors associated with certain joints and the eyes. Visual accessory organs include the eyelids and lacrimal apparatus that protect the eye and the extrinsic muscles that move the eye. Structure of the eye (1) the wall of the eye has an outer, a middle, and an inner tunic that function as follows: (a) the outer layer (sclera) is protective, and its transparent anterior portion (cornea) refracts light entering the eye.
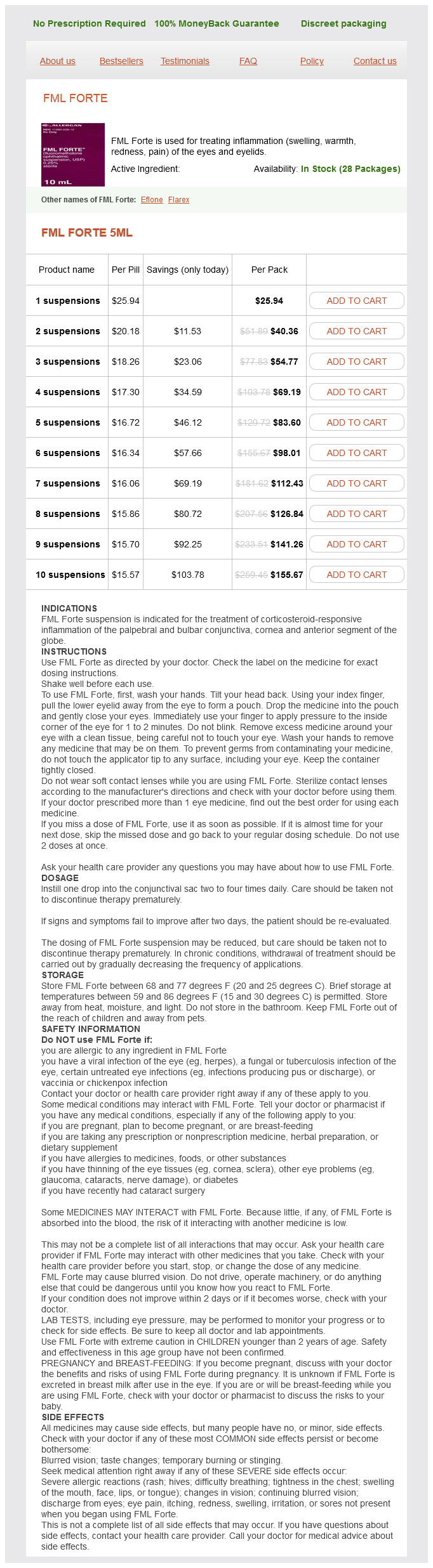
FML Forte Dosage and Price
FML Forte 5ml
- 1 suspensions - $25.94
- 2 suspensions - $40.36
- 3 suspensions - $54.77
- 4 suspensions - $69.19
- 5 suspensions - $83.60
- 6 suspensions - $98.01
- 7 suspensions - $112.43
- 8 suspensions - $126.84
- 9 suspensions - $141.26
- 10 suspensions - $155.67
These vessels descend on either side of the neck allergy vs adverse drug reaction cheap fml forte generic, passing over the sternocleidomastoid muscles and beneath the platysma. The internal jugular veins, which are somewhat larger than the external jugular veins, arise from many veins and venous sinuses of the brain and from deep veins in parts of the face and neck. They descend through the neck beside the common carotid arteries and also join the subclavian veins. These unions of the internal jugular and subclavian veins form large brachiocephalic veins on each side. These vessels then merge in the mediastinum and give rise to the superior vena cava, which enters the right atrium. A lung cancer, enlarged lymph node, or an aortic aneurysm can compress the superior vena cava, interfering with return of blood from the upper body to the heart. This produces pain; shortness of breath; distension of veins draining into the superior vena cava; and swelling of tissues in the face, head, and upper limbs. The right and left ascending lumbar veins, with tributaries that include vessels from the lumbar and sacral regions, also connect to the azygos system. Veins from the abdominal Viscera Veins transport blood directly to the atria of the heart, except for portal veins, such as those that drain the abdominal viscera (fig. They originate in the capillary networks of the stomach, intestines, pancreas, and spleen and transport blood from these organs through a hepatic portal (portal) vein to the liver (fig. This unique venous pathway is called the hepatic portal system, which allows blood to flow from the gastrointestinal organs to the liver before returning to the heart. It regulates blood glucose concentration by polymerizing excess glucose into glycogen for storage or by breaking down glycogen into glucose when blood glucose concentration drops below normal. The liver helps regulate blood concentrations of recently absorbed amino acids and lipids by modifying them into forms cells can use, by oxidizing them, or by changing them into storage forms. Blood in the hepatic portal vein nearly always contains bacteria that have entered through intestinal capillaries. Large Kupffer cells lining the hepatic sinusoids phagocytize these microorganisms, removing them from the portal blood before it leaves the liver. After passing through the hepatic sinusoids of the liver, the blood in the hepatic portal system travels through a series of merging vessels into hepatic veins. These veins empty into the inferior vena cava, returning the blood to the general circulation. In the bend of the elbow, a median cubital vein ascends from the cephalic vein on the lateral side of the forearm to the basilic vein on the medial side. It is often used as a site for venipuncture, when it is necessary to remove a sample of blood for examination or to add fluids to the blood. Veins from the abdominal and Thoracic Walls Tributaries of the brachiocephalic and azygos veins drain the abdominal and thoracic walls. For example, the brachiocephalic vein receives blood from the internal thoracic vein, which generally drains the tissues the internal thoracic artery supplies. The azygos (azi-gos) vein originates in the dorsal abdominal wall and ascends through the mediastinum on the right side of the vertebral column to join the superior vena cava. Tributaries of the azygos vein include the posterior intercostal veins on the right side, which drain the intercostal spaces, and Veins from the Lower Limb and Pelvis Veins that drain the blood from the lower limb can be divided into deep and superficial groups, as in the upper limb (fig. The deep veins of the leg, such as the paired anterior and posterior tibial veins, have names that correspond to the arteries they accompany. Small intestine Ascending colon Inferior vena cava Descending colon Right common iliac v. This vein continues upward through the thigh as the femoral vein, which, in turn, becomes the external iliac vein. The superficial veins of the foot, leg, and thigh connect to form a complex network beneath the skin. The small saphenous (sah-fenus) vein begins in the lateral portion of the foot and passes upward behind the lateral malleolus. It ascends along the back of the calf, enters the popliteal fossa, and joins the popliteal vein. The great saphenous vein, the longest vein in the body, originates on the medial side of the foot. It ascends in front of the medial malleolus and extends upward along the medial side of the leg and thigh. In the thigh just below the inguinal ligament, it deeply penetrates and joins the femoral vein. Near its termination, the great saphenous vein receives tributaries from a number of vessels that drain the upper thigh, groin, and lower abdominal wall. In addition to communicating freely with each other, the saphenous veins communicate extensively with the deep veins of the leg and thigh. These veins are formed by tributaries corresponding to the branches of the internal iliac artery, such as the gluteal, pudendal, vesical, rectal, uterine, and vaginal veins. Typically, these veins have many connections and form complex networks (plexuses) in the regions of the rectum, urinary bladder, and prostate gland (in the male) or uterus and vagina (in the female). The internal iliac veins originate deep within the pelvis and ascend to the pelvic brim. There they unite with the right and left external iliac veins to form the common iliac veins. Autopsies of soldiers killed in the Korean and Vietnam Wars, for example, revealed significant plaque buildup in the arterial walls of otherwise healthy young men. Incidence of disease of the heart and blood vessels increases exponentially with age. About 60% of men over age sixty have at least one narrowed coronary artery; the same is true for women over age eighty. Assessing cardiac output over a lifetime vividly illustrates how cardiovascular disease prevalence can interfere with studying the changes associated with normal aging.