General Information about Dutasteride
While Dutasteride has been confirmed to be efficient within the remedy of BPH, it might even have some potential unwanted effects. These can embrace headache, dizziness, decreased libido, and erectile dysfunction. In rare cases, it could additionally cause breast tenderness or enlargement, so it is essential to talk about any concerns with a health care provider.
In conclusion, Dutasteride is a broadly used and efficient medication in the therapy of BPH. It works by lowering the levels of DHT, which helps to shrink the prostate gland, relieving urinary signs and enhancing the quality of life for patients. It is important to observe the recommended guidelines for its use and seek the assistance of with a healthcare skilled if any unwanted effects or issues come up.
In addition to its use within the remedy of BPH, Dutasteride has also been found to be effective in treating male pattern baldness. As DHT can be responsible for hair loss in males, lowering its ranges can contribute to hair regrowth. However, you will need to observe that it isn't particularly accredited for this function.
The major goal of treatment for BPH is to alleviate these urinary symptoms and improve the standard of life for patients. Medications like Dutasteride are sometimes the primary line of therapy for BPH, earlier than considering surgical procedure.
Dutasteride, also identified by its model name Avodart, is a drugs used for the therapy of Benign Prostatic Hyperplasia (BPH). BPH is a situation during which the prostate gland turns into enlarged, causing urinary symptoms such as frequent or troublesome urination. Dutasteride works by inhibiting the conversion of testosterone to dihydrotestosterone (DHT), a hormone that's answerable for prostate development.
As talked about earlier, Dutasteride works by inhibiting the conversion of testosterone to DHT. DHT is a potent hormone that is responsible for the growth of the prostate gland. By decreasing the levels of DHT in the physique, Dutasteride helps to shrink the prostate gland, thereby reducing the strain on the urethra and assuaging urinary symptoms.
Dutasteride ought to be taken exactly as prescribed by a doctor, usually once a day with or with out food. It could take as much as six months to see the full results of treatment, and the medication ought to be taken consistently to take care of its advantages. As with any medication, it's essential to follow the directions and precautions outlined by a health care provider or pharmacist.
Originally developed and marketed by GlaxoSmithKline, Dutasteride was accredited by the US Food and Drug Administration (FDA) in 2002 for the remedy of BPH. It is on the market as an oral capsule in strengths of zero.5 mg.
BPH is a typical situation, significantly in men over 50 years of age. As the prostate gland continues to grow throughout a man's life, it may possibly put strain on the urethra, the tube that carries urine from the bladder out of the physique. This pressure can lead to urinary symptoms corresponding to issue in beginning urination, weak urinary move, the want to urinate incessantly, and the sensation of incomplete voiding.
The name diverticulosis is used merely to indicate the presence of multiple diverticula in the large intestine hair loss in men makeup cheap 0.5 mg dutasteride with mastercard, with or without the accompanying muscle abnormality found in classic diverticular disease and irrespective of aetiology or symptomatology. Diverticular disease, on the other hand, is used to describe a specific clinical disorder with defined radiological and pathological appearances, in which there is a characteristic muscle abnormality, usually, but not invariably, accompanied by the presence of diverticula that may or may not be inflamed. Diverticulitis is applied when one or more diverticula are the source of visible macroscopic inflammation. Epidemiology the prevalence of diverticular disease has been calculated from radiological studies [14], colonoscopy [5] and at necropsy [69]. Several studies have been published looking at admissions to hospital, hospital-related episodes and mortality [1014]. In most studies from western nations, the incidence of diverticular disease rises steadily with increasing age, up to approximately 30% over the age of 60. There are no or only minor differences in incidence between males and females, with some studies showing a small excess in females [39,12]. Diverticular disease is common in northern Europe, North America and Australia [7,13,14], but is less common in southern Europe and South America, where the population is mainly of Latin origin. There are also variations, both racial and socio-economic, within national boundaries [4,5]. Diverticulosis is eight times more common in white people than among the black population of Johannesburg, where the condition is much more common in urban communities than in rural areas [17]. In Israel it is much more common among the Ashkenazim than in Sephardic and Oriental Jews and Arabs; the incidence is increasing in the latter groups but is stable in the Ashkenazi population [18]. The differences between the lower rates in non-western immigrants and the native western population appears to diminish with time in the country, as noted in a large population study in Sweden [12]. Although only 12% of affected individuals ever develop symptoms, most commonly diverticulitis, and only about 0. Regardless of the length of colon affected, the number of diverticula is variable, ranging from 1 or 2 to over 100. We have seen a few examples of diverticulosis confined to the right colon, but this seems to be a separate condition (see below). So-called diverticula of the rectum are congenital duplications and unrelated to diverticular disease of the colon. Macroscopic and microscopic appearances From an anatomical point of view diverticula of the colon are of typical pulsion type, consisting of a pouch of mucous membrane (including muscularis mucosae) projecting through and beyond the circular muscle layers of the bowel wall, so that the diverticula come to lie in the pericolic fat and appendices epiploicae. They remain covered by the investing layer of longitudinal muscle, but this is extremely thin. It has been confirmed that most diverticula pass through the bowel wall at weak points in the circular muscle layer, through which the main blood vessels pass to supply the colonic mucosa [19]. This important anatomical fact explains the complication of diverticular haemorrhage, discussed later. In about 50% of cases a third row of very small diverticula can be found between the two anti-mesenteric taeniae [20]. In western populations, diverticula are most common in the sigmoid colon; indeed they are confined to this segment in most patients. In classic diverticular disease, the proximal colon is affected only when the sigmoid is also diseased and involved in continuity; total colonic diverticulosis is not so very uncommon. The mouths of diverticula lie between the corrugations, reaching the pericolic fat. The muscle the muscle abnormality is the most striking and consistent abnormality in diverticular disease of the sigmoid colon [9,21,22]. The taeniae coli appear thick, assuming an almost cartilaginous consistency in some cases. The circular muscle is also much thicker than normal and has a corrugated or concertina-like appearance (the so-called saw-tooth sign on barium enema radiographs). In between these muscular corrugations, the mouths of the diverticula are found penetrating the bowel wall to reach the pericolic fat. Sometimes, the bowel wall between the corrugations shows no diverticulum formation but rather a tendency to sacculation. In some specimens the mucosal surface between the corrugations appears trabeculated and looks very similar to the trabeculation of the bladder seen in chronic prostatic obstruction. If the structure of the bowel is studied in transverse section or by opening longitudinally without bisection it can be seen that these inter-digitating processes are not continuous around the circumference of the bowel wall. They are, in fact, semilunar arcs of muscle confined to the zone between the mesenteric and anti-mesenteric taeniae. In some specimens of long-standing disease the number of arcs of circular muscle is so great that they appear fused. The circular muscle between the anti-mesenteric taeniae of the sigmoid shows only small muscle ridges projecting in to the lumen of the bowel. The degree of muscular thickening is variable, being particularly obvious in specimens from the sigmoid. Corrugation is never present to the same degree in other parts of the colon containing diverticula, although slight muscle thickening with an increase in the number of haustral clefts can be seen in the ascending and transverse colon of otherwise normal specimens. Excess fat around the sigmoid colon has been described in many patients with diverticular disease. It has been suggested that this results from a local response to chronic inflammation. It is also possible, however, that this observation merely reflects the fact that overweight middle-aged people (who have more intra-abdominal fat) are more susceptible to the disease.
Seldom is histopathological assessment required hair loss diet discount dutasteride, except in longer duration ente- rocolitis [52]. In severe cases, the changes of acute colitis may be prominent whereas the small bowel mucosa shows more subtle signs [53]. Entry of cells is followed by interference with normal mechanisms to create a phagolysosome engulfing the salmonellae and alteration of the immune response to favour bacterial survival. SipA interacts with actin and is crucial for cytoskeletal changes, SipC interferes with normal intracellular trafficking and SipB promotes chloride secretion. Infection occurs in all age groups and results in a syndrome of acute abdominal pain, fever and inflammatory enterocolitis, which ranges from a generally mild secretory diarrhoea to a severe dysentery-like syndrome. The variable clinical picture is probably more due to the host immune response than to strain virulence factors. Campylobacter jejuni causes local acute inflammation in both the small and the large intestine [55]. The enteric fevers: typhoid and paratyphoid Typhoid fever, caused by Salmonella enteritidis serovar typhi, remains a serious health problem throughout the world, especially in south and south-east Asia and South America, with an estimated 1633 million cases and about half a million deaths annually. This fall and the great improvement in its prognosis are due to improved living conditions and sanitation and the introduction of effective antibiotic therapy. The incidence is estimated to be 330 cases per 100 000 travellers to developing countries [57]. The disease is characterised by a sudden onset of fever, headache, nausea, loss of appetite, abdominal discomfort and constipation or diarrhoea in young children. On contact with these cells they are rapidly internalised and transported in to the submucosal lymphoid tissue, where they may enter the bloodstream, without producing any local lesions, and may be isolated by blood culture during the first week or two of the illness. After multiplication in the bloodstream, the organisms are excreted by the liver in to the bile, and enter the gallbladder and intestinal contents in rapidly increasing numbers; they can be cultured from the faeces in an increasing proportion of cases, the highest incidence of positive stool cultures occurring in the third week of the illness. As a result of the marked inflammatory reaction and oedema, the ulcers are often raised above the surrounding mucosa, from which they are sharply demarcated. The base of the ulcer contains black necrotic material: healing begins with shedding of the slough. Healing is complete within a week or so of the subsidence of the acute manifestations of the illness and there is little fibrosis. This accounts for the low frequency of strictures as a result of previous typhoid fever. Local lymph nodes are considerably enlarged, soft and hyperaemic at the height of the disease. Histologically, enteric fever shows hyperaemia and oedema in the early stages with proliferation of large, often deeply staining mononuclear cells, which are modified phagocytes (containing intracellular organisms) [60]. Moderate numbers of lymphocytes and plasma cells are present but neutrophil polymorphs are strikingly rare, accounting for the typical neutropaenia found in the blood. Later, focal necrosis develops in lymphoid tissue, the necrotic foci becoming confluent and ulceration occurs. Large numbers of typhoid bacilli are present in the intestinal lesions and regional lymph nodes. Enteric fever is associated with significant local complications such as perforation of the ulcers and haemorrhage. Perforation occurs most frequently in the terminal ileum, in about 510% of cases, and it may be that many ulcers perforate or are close to perforation at the same time [61]. At surgery, the small bowel is markedly friable and perforation is a common cause of death from the disease. Haemorrhage from the ulcers is the next most frequent complication and occurs at about the same stage in the course of the disease. Acute bronchitis, meningitis, nephritis, orchitis, arthritis and osteitis due to the presence of typhoid bacilli in the tissues concerned have all been described. It can be caused by any of the three serotypes of Salmonella paratyphi, now named S. Pathologically the lesions resemble those of typhoid, but they are confined to a smaller area of the terminal ileum. Ulceration is not such a marked feature, and serious complications, comparable with those of typhoid fever, are rare. Cholera Cholera is an acutely dehydrating, watery diarrhoeal disease caused by Vibrio cholerae serotype O1, a Gramnegative bacterium. Before the advent of an effective rehydration therapy, cholera epidemics were associated with case fatality rates exceeding 40%. Although the disease no longer poses a threat to countries with good standards of hygiene, it remains a challenge to countries where access to safe water and proper sanitation is not guaranteed [1]. There the organism penetrates the mucous gel and adheres to the brush border of intestinal epithelial cells via specific adhesins. The organism will produce a number of proteins secreted extracellularly, including cholera toxin. This mol- Inflammatory disorders of the small intestine 321 ecule has two important functioning moieties. There is not often cause to seek the histopathological features of cholera because treatment is largely supportive and biopsy adds little to the management of the disease. Clinical and experimental studies have shown villous damage with necrosis of enterocytes, disruption of the underlying basement membrane and necrosis of lymphoid tissue [62]. In the lamina propria there is commonly an increase of lymphocytes and plasma cells but not of eosinophils or neutrophils [63]. Ultimately the cell is killed but this killing seems slower and less efficient than the killing by invasive bacteria [50]. The heat-labile toxin leads to activation of epithelial adenylyl cyclases whereas the heat-stable toxin activates guanylyl cyclases.
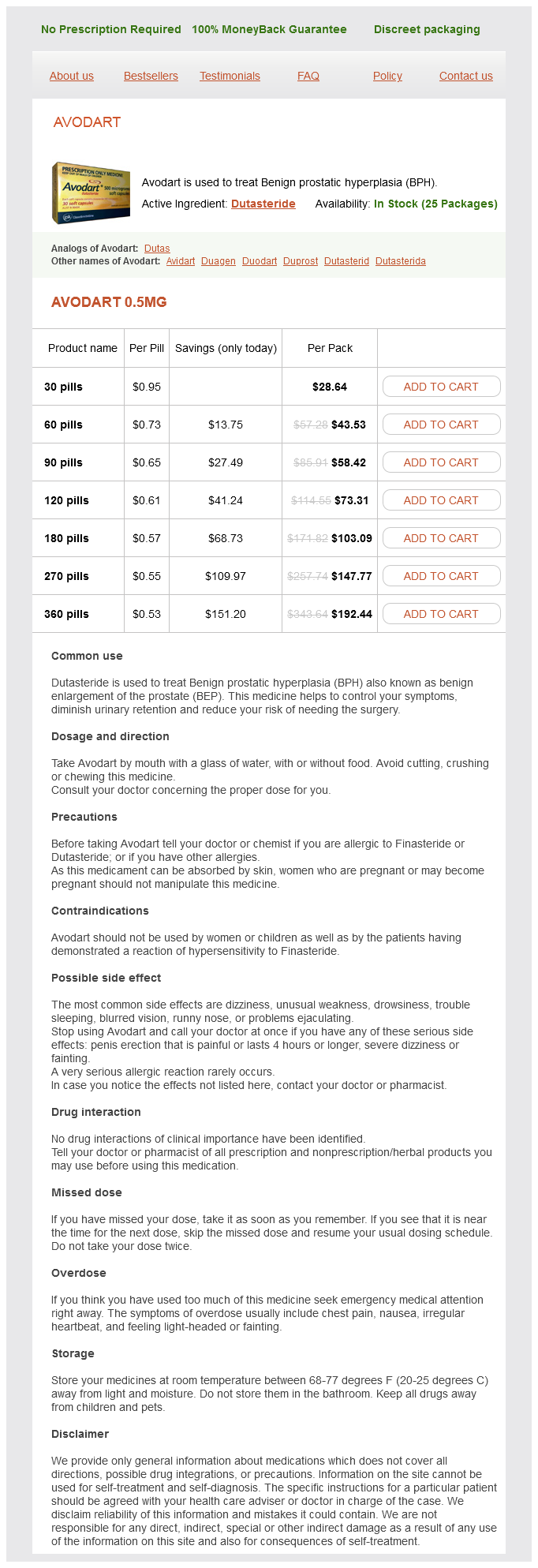
Dutasteride Dosage and Price
Avodart 0.5mg
- 30 pills - $28.64
- 60 pills - $43.53
- 90 pills - $58.42
- 120 pills - $73.31
- 180 pills - $103.09
- 270 pills - $147.77
- 360 pills - $192.44
Sometimes the polyps are remarkably thin and filiform hair loss cure 768 cheap 0.5 mg dutasteride with mastercard, and they may have a curious resemblance to worms. Ulceration is conspicuous by its absence on macroscopic inspection and adjacent flat mucosa can appear quite normal. If there is no ulceration or transmural inflammation, and the disease is confined to the polypoid mucosa, then a diagnosis of ulcerative colitis is more likely. Faeces tend to become trapped within the maze of mucosal fronds and this can cause local inflammation. The pathogenesis of this inflammatory polyposis reflects previous severe ulceration, islands of preserved inflamed and oedematous mucosa that eventually take the shape of polyps [417,456]. The main problems with these lesions are that they may cause obstructive symptoms and it is also virtually impossible to carry out surveillance, so their presence leads to serious consideration of colectomy. In ulcerative colitis, such (giant) inflammatory polyposis of the colorectum has especial features for which there have been few sensible explanations. First, the disease is often very sharply localised, especially in the descending colon and sigmoid colon, whereas the rest of the colorectum shows characteristic features of ulcerative colitis but without very much inflammatory polyposis. This may provide that unusual indication in the management of ulcerative colitis for a segmental colectomy (often because of obstructive symptoms). Second, it is a characteristic feature that, although the flat mucosa shows the distinctive changes of ulcerative colitis, especially in the form of crypt architectural distortion, the mucosa lining the filiform polyps often appears relatively normal having few, if any, features of chronic ulcerative colitis. The importance of examining the mucosa away from the polyposis areas for evidence of ulcerative colitis cannot be over-emphasised in this situation. A third feature is that (giant) inflammatory 600 Large intestine polyposis of the colorectum complicating ulcerative colitis is especially prone to submucosal epithelial misplacement (colitis cystica profunda), and this may show profound mimicry of, admittedly very well differentiated, adenocarcinoma. It is also one occasion where a disease that looks identical to ulcerative colitis has rectal sparing. Worse, because one of the complications of complex diverticular disease is fistula formation, the presence of fistulae can further confuse the picture. In some cases of diverticulosis, the mucosa between the diverticula may be normal. Mechanical damage to the redundant mucosa, a feature of diverticular disease, may account for this. Only two biopsies (towards the right-hand end) show chronic inflammatory changes with crypt architectural distortion and these derive from the sigmoid colon. Inflammatory disorders of the large intestine 601 seems to us the most simple and applicable appellation) or diverticulosis-associated colitis. The key to excluding ulcerative colitis is to take biopsies from the rectum, because these will be normal. However, an important caveat here is that a small number of cases of diverticular colitis, without evidence of rectal involvement, will ultimately evolve in to classic ulcerative colitis [460,466,468]. This is one of the few examples when ulcerative colitis does not start in the rectum. Diverticular colitis represents an unusual spectrum of pathology in the sigmoid colon afflicted by diverticulosis. Ischaemia, for example, is a consideration in elderly people but is very unlikely in a teenager. Recent antibiotics or recent travel may also direct attention to the relevant clinical diagnosis. Classification is bedevilled by the problem that there is no single histological feature that is invariably present in any one condition and invariably absent from the others. In remission, the architectural distortion so typical of chronic ulcerative colitis seldom causes diagnostic confusion. Crypt architectural distortion, a villiform surface, goblet cell depletion, prominent crypt abscesses and a diffuse, predominantly plasma cell infiltrate of the lamina propria, point strongly to a diagnosis of ulcerative colitis. Neutrophils are the most conspicuous inflammatory cell, migrating in a characteristic way between the crypt epithelial cells to produce a cryptitis, and also seen clustered in the lamina propria. There is frequently obvious mucosal oedema and the plasma cell infiltrate is light to moderate. Granulomas may occur in campylobacter colitis, chlamydia proctitis, yersiniosis and of course tuberculosis [91,104]. A similar histological appearance can also be seen as a local reaction to malignant disease [472]. Involvement of the large bowel in sarcoidosis is extremely rare and is usually clinically silent [473,474]. Active chronic inflammation of the large intestinal mucosa with granulomas has recently been described in the cord colitis syndrome [475], a novel form of intestinal inflammation occurring in recipients of stem cell transplants with umbilical cord blood (but not with other allogeneic haematopoietic tissues). The condition appears to be different from graft-versus-host disease and usually responds to antibiotics, despite an inability to demonstrate any infective agent (see Chapter 40). Neutrophils may form crypt abscesses but their numbers seldom match those seen in ulcerative colitis or infection, although at times they can be more intense and also exquisitely focal. A pitfall is the biopsy appearance of a patient with resolving ulcerative colitis. Considerable reliance must be placed on crypt distortion with the caveat that this can be irregular in areas of healing ulceration of whatever aetiology. The presence of crypt irregularity has been shown to be reliable in several studies militating against a diagnosis of infection [72,73,478481]. In severe shigella dysentery, however, extensive crypt distortion is well described [26,28]. A problem facing the pathologist is to know how often a biopsy of these two conditions may mimic infection or vice versa.