General Information about Diovan
In recent years, Diovan has also been accredited for the therapy of coronary heart failure, a situation by which the center is unable to pump blood successfully. By decreasing the strain on the center and bettering blood circulate, Diovan might help enhance the signs of heart failure and reduce the chance of hospitalization.
One of the primary advantages of Diovan is its capability to selectively block the angiotensin II receptors, not like some other medications that work by inhibiting angiotensin-converting enzyme (ACE). This makes Diovan a well-tolerated drug, with few unwanted effects reported by sufferers. Some frequent side effects could embody dizziness, headaches, and fatigue, however these are usually mild and momentary. It is essential to notice that Diovan should not be used by pregnant ladies as it could harm the unborn baby.
High blood strain is a common condition that affects hundreds of thousands of individuals worldwide. It happens when the force of blood against the artery walls is simply too high, placing strain on the heart and blood vessels. If left untreated, high blood pressure can result in severe well being problems corresponding to heart illness, stroke, and kidney failure. That's why it is necessary for individuals with hypertension to lower their blood pressure to a healthy stage.
Diovan works by blocking the motion of angiotensin II, a hormone that causes blood vessels to constrict and slim. This leads to relaxation and widening of the blood vessels, which allows for increased blood move and reduces the blood pressure. The medicine additionally helps the kidneys to remove extra fluid and sodium, which additional lowers the blood pressure. By targeting these two mechanisms, Diovan successfully lowers blood pressure and reduces the chance of cardiovascular ailments.
In conclusion, Diovan is an effective and well-tolerated medication for the treatment of hypertension and coronary heart failure. With its ability to relax blood vessels and lower blood pressure, it plays a vital role in lowering the danger of cardiovascular ailments. As with any treatment, it is necessary to follow the prescribed dosage and consult with a physician earlier than making any adjustments. With Diovan, patients can take control of their blood pressure and improve their total health and well-being.
Diovan, also known by its generic name Valsartan, is a drugs used to deal with hypertension, or high blood pressure. It belongs to a category of medicine generally known as angiotensin receptor blockers (ARBs) and works by enjoyable blood vessels, which helps to lower blood pressure. First launched in 1996, Diovan has turn into a preferred choice for docs and patients looking for an effective and well-tolerated therapy for hypertension.
Diovan is on the market in pill type and is normally taken as quickly as a day, with or without food. The dosage could range relying on the person's medical situation and response to remedy. It's necessary to follow the prescribed dosage and to not stop taking the medicine without consulting a doctor, even when the signs enhance. Suddenly stopping Diovan may cause a sudden improve in blood strain, which may lead to serious well being penalties.
Diovan has been extensively studied in giant medical trials and has proven to be an efficient treatment for hypertension. In addition to lowering blood strain, it has additionally been proven to enhance blood circulate and cut back stress on the center, making it a perfect selection for sufferers with underlying coronary heart conditions. It has additionally been discovered to be effective in stopping strokes in patients with high blood pressure.
All patients should have undergone a thorough psychological assessment and clearance blood pressure medication nausea cheap diovan 80 mg on-line. On the morning of the procedure, the patient is admitted to outpatient surgery for the trial stimulation procedure and 24-hour observation. Minimal intravenous sedation is given because it is important to be able to communicate with the patient while positioning the stimulating electrode. The patient is then prepared and draped in a sterile fashion, and local anesthetic is infiltrated at the site of entry. An electrode array is placed through the needle to the epidural space and threaded to the appropriate level. A small bend in the electrode array just distal to the end facilitates steering of the electrode to a specific site. A trial-stimulating unit is connected to the proximal end of the electrode array to the power source. The distal end of the catheter electrode is anchored with skin suture and dressing. E, the verification screening electrode is now connected to the stimulator screening box to test stimulation. F, Once the electrode is in good position, the Tuohy needle is cautiously removed without pushing the electrode any further. The patient is prepared and draped in the usual manner for surgery, with a strict aseptic technique. Fluoroscopy is used to guide and confirm the needle of entry into the epidural space. Care must be taken to drape the fluoroscopy unit and to provide an extra side drape, to prevent contamination of the surgical field during cross-table views. Fluoroscopy helps guide placement of two leads, if needed, for bilateral pain distribution. In the anteroposterior view, the site of entry of the Tuohy needle between L1-L2 interspace just lateral to the spinous process. In this radiograph the electrode has gone anteriorly and the tip is bounced back posteriorly. It is important to keep the angle of entry as shallow as possible, to more easily advance the lead cephalad. With a shallower angle, steering of the lead is easier because of the mechanical advantage it affords. Fluoroscopy combined with the standard loss-ofresistance technique increases the chance of nontraumatic entry into the epidural space. Real-time imaging can often guide placement of the lead through resistance in the epidural space, along the way to final placement. A single lead should be placed slightly ipsilateral to the painful side and as close as possible to the physiologic midline for bilateral pain coverage. Coverage of the painful region with stimulation paresthesia determines the final lead placement. A dual lead may be necessary for better coverage in the same side or for bilateral coverage of the extremity, as well as for capturing axial low back pain. As the fibrous tissue invests the lead electrodes, resistance to delivery of the electrical impulses can increase. This should be expected, and the patient made aware that it is a normal occurrence. This maturation process can often require reprogramming of the electrode array, pulse width, and frequency. The three-dimensional space surrounding the lead can be altered by the natural process of healing in a manner that renders the stimulator system ineffective, despite a successful trial. Migration of the lead after maturation is much less likely, but it still can occur. Accommodation describes the phenomenon by which the body comes to "ignore" a steady, unvarying electrical stimulus over time. Patients who leave their stimulator systems on continuously may accommodate much more rapidly, causing the stimulation to become ineffective. The body has now formed a fibrous capsule around the various components of the implant, which is less likely to migrate or produce any of the complications mentioned in the previous section. Several potential difficulties still lie in wait for the unsuspecting physician implanter. There are four anterior sacral foramina through which the sacral nerves exit and lateral sacral arteries enter. The sacral hiatus is formed by the failure of the laminae of S5 to unite posteriorly. The bodies of S1 and S2 may fail to unite or the sacral canal may remain open throughout its length. Laboratory Studies Complete blood count with platelets Prothrombin time, partial thromboplastin time Platelet function test or bleeding times Urinalysis Magnetic resonance imaging (optional) for canal size Voiding disorders (urinary incontinence, urinary retention, voiding dysfunction) Chronic pelvic pain (interstitial cystitis, pudendal neuralgia, vulvodynia) Preoperative Medication For preoperative medication, use the standard recommendations for conscious sedation by the American Society of Anesthesiologists. If adequate responses are obtained during the acute testing, then test stimulation needs to be conducted for several days (not to exceed 7 days). Stimulation is achieved by replacing the stimulation needle with a temporary screening lead placed through the needle and connected to the same external screener that is used during the test phase. The patient controls the amplitude of the stimulation so that it is sensate but painless. Patients are informed that 516 Advanced Techniques discomfort threshold is the amplitude at which the paresthesias become uncomfortable. In all patients, criteria for a successful trial generally includes greater than 50% reduction in pain level, reduced consumption of pain medications, and increased activities of daily living.
Posterior segmental arteries are more numerous and evenly distributed than anterior segmental arteries and supply the posterior spinal arteries heart attack demi lovato mp3 buy diovan 80 mg free shipping. Trauma to the epidural arteries can result in epidural hematoma formation and compromise the blood supply to the spinal cord itself. The lymphatics of the epidural space are concentrated in the region of the dural roots, where they remove foreign material from the subarachnoid and epidural spaces. The entry level of the epidural space should be inferior to the level of stenosis whether a singleshot or catheter technique is used. While these patients should be classified as having chronic pain, they are sometimes reasonable candidates for subacute, new radicular symptoms. The epidural space contains adipose, connective tissue, nerves, arteries, lymphatics, and a venous plexus. The amount of epidural fat varies in direct proportion to the amount of fat stored elsewhere in the body. Great care is needed to avoid dural punctures or other mechanical complications, such as loculation. Some would advocate a technique such as catheter placement from a thoracic level or transforaminal blunt needle approach as an alternative to a cervical interlaminar approach. If small-caliber (2022 gauge) needles are used, it is more likely to penetrate to an unknown depth, especially if a lateral view is not obtained. Even small amounts of intracord injection may lead to syrinx formation and/or permanent cord injury. Procedures for patients who cannot be visualized adequately with fluoroscopy or who have abnormal or questionable contrast distribution should be aborted. Obese patients and patients with posterior hardware are frequently difficult to visualize, and it is best to terminate the procedure and simply explain the safety concern to the patient. Contrast should be visualized in the epidural space, which is distinguishable from subarachnoid collection. Subdural contrast injection is of concern and sometimes requires multiple views to confirm. Intravascular injection may be detected by visualized contrast flow in a vein or artery but also may only be recognized by a lack of contrast collection in the area of the needle. Patients with rapidly worsening pain, numbness, weakness, hyperreflexia, changes in bladder function, and other neurological symptoms should prompt a reevaluation and surgical evaluation when indicated. A suspected cord lesion from a hematoma or other compression requires emergent imaging. A contingency plan needs to be in place with the radiology department to short-circuit delays under these circumstances. Active illness or disease, such as a febrile patient, local infection, or coagulopathy, are contraindications. Anticoagulation with prescription medications is becoming more common for patients with atrial fibrillation, coronary artery disease, cerebrovascular, peripheral vascular disease, and in the postoperative period. Patients need to discuss their periprocedure anticoagulation with the prescribing physician. Patients with mechanical valves, recent deep venous thrombosis, or other conditions prohibiting discontinuing anticoagulation may convert from coumadin to lovenox 5 days prior to the procedure, and lovenox can be held for 12 hours immediately prior to the procedure. Plavix should be held for 1 week, and other prescription anticoagulants should be held for the appropriate time. Aspirin is stopped 1 week prior to a procedure and nonsteroidal anti-inflammatory drugs are discontinued 2 days prior to procedures. Patients should be asked about over-the-counter medication including herbal products such as ginko, garlic, ginseng, vitamin E, and so on. Patients of reproductive age should be questioned about pregnancy, tested if necessary, and shielded from fluoroscopy. Uncontrolled diabetes, hypertension, and heart failure may become exacerbated by corticosteroid administration. Patients with substance abuse, pain disorder with predominant psychological factors, or other psychiatric problems should be stabilized or referred for more appropriate care prior to interventional pain procedures. A history of allergy to contrast is not uncommon, and while not an absolute contraindication, it may lead to consideration of other options including catheter techniques. The procedure must be performed under fluoroscopy guidance with appropriate radiation protection equipment including lead aprons, thyroid shields, and leaded gloves. Contrast should be water-soluble or nonionized such as Omnipaque 240 or other myelogram-quality contrast. The field needs to be sterilized, after verifying that the patient is not allergic to iodine-containing solutions such as betadine. It is recognized that the Tuohy needle is most commonly used; however, there is an increasing number of complications from the tip design, where the sharp cutting edge of the needle may cut not only into the epidural space but partially into the subdural space. Similarly, in the upper cervical area if the needle tip ends up off midline, laceration of segmental arteries can be followed by a rapidly expanding arterial hematoma with pain, numbness, and evidence of cord compression. Midline interlaminar needle placement, especially without lateral fluoroscopic visualization, may result in intracord needle placement and injection. The needle selection should be a 2530-gauge needle for local anesthetic infiltration, an 18-gauge, B-bevel needle for opening up a hole through the skin, an 18-gauge, 3-1/2-inch R-X Coudé needle, and in some instances, the 130 Head and Neck 18-gauge reverse R-X Coudé needle. Additional equipment includes a loss-of-resistance, low-friction syringe, preservative-free injectable saline, fentanyl, 0.
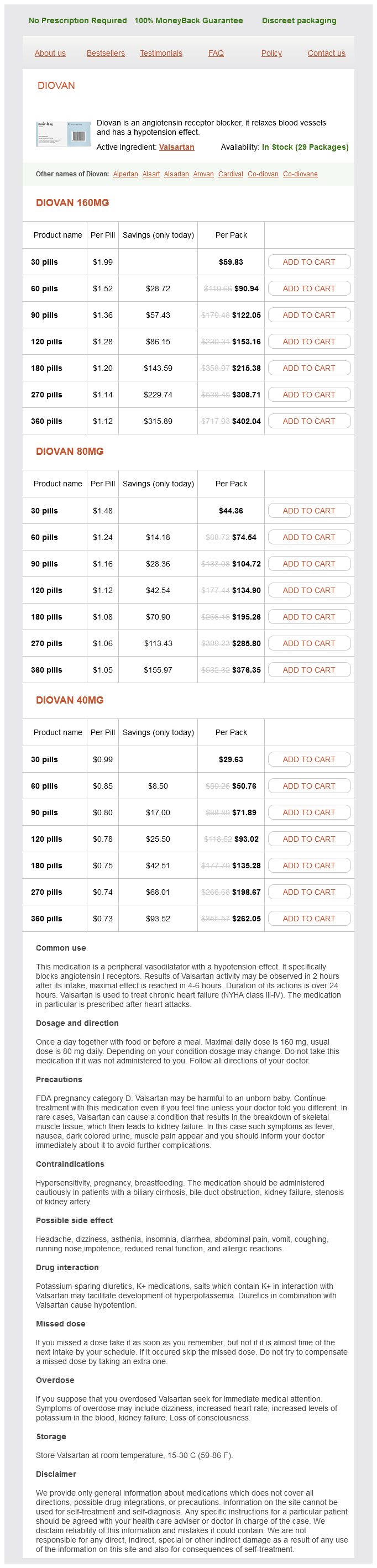
Diovan Dosage and Price
Diovan 160mg
- 30 pills - $59.83
- 60 pills - $90.94
- 90 pills - $122.05
- 120 pills - $153.16
- 180 pills - $215.38
- 270 pills - $308.71
- 360 pills - $402.04
Diovan 80mg
- 30 pills - $44.36
- 60 pills - $74.54
- 90 pills - $104.72
- 120 pills - $134.90
- 180 pills - $195.26
- 270 pills - $285.80
- 360 pills - $376.35
Diovan 40mg
- 30 pills - $29.63
- 60 pills - $50.76
- 90 pills - $71.89
- 120 pills - $93.02
- 180 pills - $135.28
- 270 pills - $198.67
- 360 pills - $262.05
Patients who could benefit from this therapy are those with poststroke pain arteria3d pack unity discount diovan 80 mg buy on line, trigeminal neuropathic pain, and anesthesia dolorosa. Other indications include deafferentation pain as postherpetic neuralgia, brachial plexus or sciatic nerve avulsion injury, phantom limb and stump pain, and selected cases of pain after spinal cord damage. As of this writing, a total of 44 publications exist with most of the data referring to central and facial pain than for other deafferentation syndromes. Operative Procedure Clotting disorders Ongoing infection Local infection Patient unable to fully understand treatment objectives Psychiatric disorders, major depression, drug abuse Sterile conditions are established in the neurosurgical operating room. The head is fixed in a three-point pin holder, after administering intravenous sedation and analgesia and local anesthesia of the areas to be incised. The neuronavigation system is initiated, and data are checked using anatomical landmarks like skin, nasion, and mastoid tip. After drawing the anatomical landmarks of the central sulcus and its relation thereto with pre- and post-central gyrus, the placement of a single burr hole is made on the skin. The burr hole is performed, and a quadripolar paddle lead (Resume, Medtronic) is placed epidurally with all four contacts covering the precentral gyrus followed by connection to the electrophysiological monitoring system. In addition, patients must be able to communicate during the lengthy screening process before implantation. Analgesic and sedative medication are recommended, as is prophylactic intravenous antibiotherapy. A neuropsychological evaluation must be Cranial Stimulation 577 Intraoperative Monitoring Somatosensory-evoked potentials of the media and/or tibial nerve are recorded in a bipolar mode using two electrodes of the quadripolar lead. The lead is placed and its extension cable is then tunneled subcutaneously and fixed in the frontotemporal region. The electrode is sutured to the outer, periosteal layer of the dura and the craniotomy bone flap is secured with plates. Postoperative Test Trial Testing of the electrode can begin immediately after the patient is fully recovered and should continue for 1 week or until the patient can confirm that stimulation reduces pain by at least 50%. Stimulation is generally performed with different electrode combinations and stimulation parameters. In the case of a positive test trial, the neurostimulator (Itrel 2 or 3, Model 7425, Medtronic Inc. After implantation of the pulse generator, a regimen of intermittent stimulation is usually programmed in order to avoid habituation. The technique is more effective in trigeminal neuropathic pain than in poststroke pain, with success rates from 50 to 80%. Morbidity includes intraoperative seizures or even postoperative seizures lasting less than 3 days,39 with no reports of long-lasting seizures. Kupers R, Vos B, Gybels J: Stimulation of the nucleus paraventricularis thalami suppresses scratching and biting behaviour of arthritic rats and exerts a powerful effect on tests for acute pain. Tsubokawa T, Yamamoto T, Katayama Y, et al: Thalamic relay nucleus stimulation for relief of intractable pain: clinical results and beta-endorphin immunoreactivity in the cerebrospinal fluid. Nandi D, Asís T, Carter H, et al: Thalamic field potentials in chronic central pain treated by periventricular gray stimulation-a series of eight cases. Tsubokawa T, Katayama Y, Yamamoto T, et al: Chronic motor cortex stimulation in patients with thalamic pain. Meyerson B: Motor cortex stimulation-effective for neuropathic pain but the mode of action remains illusive. Canavero S, Bonicalzi V: Therapeutic extradural cortical stimulation for central and neuropathic pain: a review. Carroll D, Joint C, Maartens N, et al: Motor cortex stimulation for chronic neuropathic pain: a preliminary study of 10 cases. Nuti C, Peyron R, Garcia-Larrea L: Motor cortex stimulation for refractory neuropathic pain: four year outcome and predictors of efficacy. Rasche D, Ruppolt M, Stippich C: Motor cortex stimulation for long-term relief of chronic neuropathic pain: a 10 year experience. Smith H, Joint C, Schlugman D, et al: Motor cortex stimulation for neuropathic pain. Complications related to surgery include stimulatorpocket infection or wound infection, epidural hematoma, subdural effusion, and dehiscence of the stimulator pocket. Hosobuchi Y: Combined electrical stimulation of the periaqueductal gray matter and sensory thalamus. Mazars G, Merienne L, Cioloca C: Traitement de certains types de douleurs par des stimulateurs thalamiques implantables. During monitoring, incidentally, these patients also had pain relief from stimulation of the third sacral nerve root. The indication for pelvic stimulation has been for bladder dysfunction and detrusor sphincter dyssynergia as in spinal cord injury where the innervation pathway has not been interrupted. The concept of retrograde electrode stimulation was introduced by Feler, Alo, and colleagues,2,3 and even early experiences indicated certain hazards. The use of the retrograde Tuohy-type needle results in an unacceptably high incidence of dural puncture. The problem has been reduced by the development of the reversed R-X Coudé needle due to the cutting end of the needle being away from the dura as the needle is passed in a retrograde manner from the L3-L4 and L4-L5 areas. Initially, the evaluation and the temporary electrode placement occurred in a blind manner where the needle was placed and stimulated without fluoroscopy, and the electrode was placed in the retroperitoneal space surrounding the S3 nerve root. The anchoring system is tested every time the patient sits down, and sliding from one sitting position to the other makes the relatively thin covering layers of the sacrum to slide and drag the electrode from the sacrum into a displaced position. The concept of retrograde stimulation was introduced primarily to allow the physician an option of covering more than one nerve root and to reduce the likelihood of electrode migration and displacement. More recently, it has been found that rectal incontinence has responded to sacral stimulation primarily the S4 rather than bladder stimulation, which is by the S3 stimulation.