General Information about Diltiazem
In conclusion, Diltiazem is a generally prescribed medication for varied coronary heart and circulatory circumstances. Its capability to improve blood circulate and regulate the heart’s rhythm makes it an essential treatment in the management of hypertension, angina, and arrhythmias. As with any medicine, it may be very important comply with your doctor’s instructions and inform them of any potential unwanted facet effects. With the assistance of Diltiazem, individuals can lead a more healthy and more active way of life.
Another frequent use of Diltiazem is for treating angina, a condition where there is a reduction in blood circulate to the center because of narrowed arteries. This may cause chest pain or discomfort, and Diltiazem helps to alleviate these signs by enjoyable the blood vessels and enhancing blood move to the center. By doing this, Diltiazem not only helps to alleviate angina symptoms but also reduces the risk of coronary heart issues.
In addition to these advantages, Diltiazem is also used to treat sure types of arrhythmias, or irregular heartbeats. By regulating the heart’s rhythm, Diltiazem helps to enhance the heart’s efficiency and scale back the risk of great complications corresponding to coronary heart failure. It is also utilized in mixture with other drugs to handle situations such as atrial fibrillation, a standard heart rhythm dysfunction.
One of the primary features of Diltiazem is its capability to block the entry of calcium into the muscle cells of the guts and blood vessels. This ends in the relaxation of those muscular tissues, which in turn helps to widen the blood vessels and enhance blood flow. By doing so, Diltiazem helps to reduce the workload on the guts and alleviates symptoms of situations such as angina, hypertension, and arrhythmias.
Diltiazem is usually used to deal with hypertension or hypertension. As a calcium channel blocker, it works by preventing calcium from entering the muscle cells of the blood vessels, inflicting them to relax and permitting blood to move more simply. This reduces the pressure in opposition to the partitions of the arteries, serving to to decrease blood pressure. In addition, utilizing Diltiazem to deal with hypertension may reduce the risk of different problems similar to heart attack and stroke.
Diltiazem is a widely prescribed medication that belongs to the category of calcium channel blockers. It works by relaxing the muscular tissues of the heart and blood vessels, making it a popular selection for treating various coronary heart and circulatory situations.
When taken as prescribed, Diltiazem is usually well-tolerated with minimal unwanted effects. However, some common unwanted aspect effects could embrace dizziness, headache, upset stomach, and flushing. In uncommon instances, more severe side effects such as problem respiratory, chest pain, and swelling of the arms and feet might occur. It is necessary to tell your doctor when you expertise any side effects while taking Diltiazem.
It is also important to notice that Diltiazem may interact with different medications, so it's crucial to inform your doctor about any other drugs or supplements you might be presently taking. This consists of over-the-counter medications, natural treatments, and nutritional vitamins. In addition, Diltiazem must be used with warning in individuals with sure pre-existing conditions similar to liver or kidney illness, in addition to pregnant or breastfeeding girls.
Apart from these major uses, Diltiazem may also be prescribed for other circumstances such as migraines and Raynaud’s Disease. Migraines are believed to be attributable to the narrowing of sure blood vessels within the brain, and Diltiazem helps to widen these vessels, providing relief from migraines. Raynaud’s Disease, a rare condition that affects the blood vessels in the fingers and toes, can be treated with Diltiazem by improving blood circulate to those areas.
The accumulation of ammonia and glutamine leads to direct neuronal toxicity and brain edema medicine to stop runny nose purchase diltiazem 180 mg with mastercard. Deficiencies in urea cycle enzymes are individually rare, but as a group, they affect about 1:35,000 individuals. They are all transmitted as autosomal recessive traits, with the exception of ornithine transcarbamylase deficiency, which is X-linked and the most frequent urea cycle defect. Hepatocytes of females with ornithine transcarbamylase deficiency express either the normal or the mutant allele due to random X-inactivation and may be unable to remove excess ammonia if mutant cells are predominant. Infants with classic urea cycle defects present at 14 days of life with refusal to eat and lethargy progressing to coma and death. Milder enzyme deficiencies present with protein avoidance, recurrent vomiting, migraine, mood swings, chronic fatigue, irritability, and disorientation that can progress to coma. Females with ornithine transcarbamylase deficiency can present at time of childbirth due to the combination of involuntary fasting and stress that favors catabolism. Administration of systemic corticosteroids can precipitate hyperammonemia and can be fatal in previously asymptomatic individuals. These patients may be misdiagnosed as having gastrointestinal disorders, food allergies, behavioral problems, or nonspecific hepatitis. The diagnosis requires measurement of plasma ammonia, plasma amino acids, and urine orotic acid, useful for differentiating ornithine transcarbamylase deficiency from carbamyl phosphate synthase-1 and N-acetylglutamate synthase deficiency. Increased plasma glutamine is seen with all urea cycle defects since ammonia not removed by the urea cycle in periportal hepatocytes is conjugated to glutamate by glutamine synthase in perivenous hepatocytes. It requires many enzymes and mitochondrial transporters, any of which can be defective and may impair the function of the urea cycle. Ammonia escaping the urea cycle in periportal hepatocytes is conjugated with glutamate by glutamine synthase in perivenous hepatocytes to generate glutamine. Plasma citrulline is markedly increased in argininosuccinic acid synthase deficiency (citrullinemia type 1), with a milder elevation in argininosuccinic acid lyase deficiency in the presence of argininosuccinic acid (argininosuccinic aciduria). Arginine levels are usually normal to low in these conditions and become markedly elevated only in patients with arginase deficiency. In addition to urea cycle defects, hyperammonemia can also be caused by liver disease from any cause and several organic acidemias and fatty acid oxidation defects (the latter two excluded by the analysis of urine organic acids and plasma acylcarnitine profile). Several of these patients have been successfully rescued from hyperammonemia using the protocol described above for urea cycle defects. Arginine (200 mg/kg per day) becomes an essential amino acid (except in arginase deficiency) and should be provided intravenously to resume protein synthesis. If these measures fail to reduce ammonia, hemodialysis should be initiated promptly. Chronic therapy consists of a protein-restricted diet, phenylbutyrate, glycerol phenylbutyrate (a liquid drug better tolerated by most patients), arginine, or citrulline supplements, depending on the specific diagnosis. Oral carglumic acid can restore a functional urea cycle in patients with N-acetylglutamate synthase deficiency and can render other therapies unnecessary. Liver transplantation should be considered in patients with severe urea cycle defects that are difficult to control medically. Hyperammonemia due to a functional deficiency of glutamine synthase can occur in patients receiving chemotherapy for different malignancies or undergoing solid organ transplants. Classes of substrates include amino acids, sugars, cations, anions, vitamins, and water. The number of inherited disorders of membrane transport continues to increase with the identification of new transporters on the plasma membrane or intracellular organelles and the clarification of the molecular basis of diseases with previously unknown pathophysiology. The first transport disorders identified affected the gut or the kidney, but transport processes are now proving essential for the normal function of every organ. Mutations in transporter molecules cause disorders of the heart, muscle, brain, and endocrine and sensory organs (Table 414-1). It is characterized by impaired reabsorption and excessive urinary excretion of the dibasic amino acids lysine, arginine, ornithine, and cystine. Because cystine is poorly soluble, its excess excretion predisposes to the formation of renal, ureteral, and bladder stones. Homozygotes for both variants have high urinary excretion of cystine, lysine, arginine, and ornithine. Cystine stones account for 12% of all urinary tract calculi but are the most common cause of stones in children. Cystinuria homozygotes regularly excrete 24007200 mol (6001800 mg) of cystine daily. Stone formation usually manifests in the second or third decade but may occur in the first year of life. Symptoms and signs are those typical of urolithiasis: hematuria, flank pain, renal colic, obstructive uropathy, and infection (Chap. Cystinuria is suspected after observing typical hexagonal crystals in the sediment of acidified, concentrated, chilled urine, or after performing a urinary nitroprusside test. Quantitative urine amino acid analysis confirms the diagnosis of cystinuria by showing selective overexcretion of cystine, lysine, arginine, and ornithine. Quantitative measurements are important for differentiating heterozygotes from homozygotes and for following free cystine excretion during therapy. Management is aimed at preventing cystine crystal formation by increasing urinary volume and by maintaining an alkaline urine pH. The daily fluid ingestion necessary to maintain this dilution of excreted cystine should be spaced over 24 h, with one-third of the total volume ingested between bedtime and 3 a.
The improvement in acidosis and anion gap medicine bobblehead fallout 4 generic diltiazem 180 mg online, a result of bicarbonate regeneration and decline in ketone bodies, is reflected by a rise in the serum bicarbonate level and the arterial pH. Depending on the rise of serum chloride, the anion gap (but not bicarbonate) will normalize. A hyperchloremic acidosis (serum bicarbonate of 1518 mmol/L [1518 meq/L]) often follows successful treatment and gradually resolves as the kidneys regenerate bicarbonate and excrete chloride. During treatment with insulin and fluids, various factors contribute to the development of hypokalemia. These include insulin-mediated potassium transport into cells, resolution of the acidosis (which also promotes potassium entry into cells), and urinary loss of potassium salts of organic acids. Thus, potassium repletion should commence as soon as adequate urine output and a normal serum potassium are documented. If the initial serum potassium level is elevated, then potassium repletion should be delayed until the potassium falls into the normal range. To reduce the amount of chloride administered, potassium phosphate or acetate can be substituted for the chloride salt. In fact, theoretical arguments suggest that bicarbonate administration and rapid reversal of acidosis may impair cardiac function, reduce tissue oxygenation, and promote hypokalemia. The results of most clinical trials do not support the routine use of bicarbonate replacement, and one study in children found that bicarbonate use was associated with an increased risk of cerebral edema. The etiology of and optimal therapy for cerebral edema are not well established, but overreplacement of free water and rapid normalization of serum glucose should be avoided. During illness or when oral intake is compromised, patients should (1) frequently measure the capillary blood glucose; (2) measure urinary ketones when the serum glucose is >13. The physical examination reflects profound dehydration and hyperosmolality and reveals hypotension, tachycardia, and altered mental status. Sepsis, pneumonia, and other serious infections are frequent precipitants and should be sought. In addition, a debilitating condition (prior stroke or dementia) or social situation that compromises water intake usually contributes to the development of the disorder. Hyperglycemia induces an osmotic diuresis that leads to intravascular volume depletion, which is exacerbated by inadequate fluid replacement. It is also possible that the liver is less capable of ketone body synthesis or that the insulin/glucagon ratio does not favor ketogenesis. The measured serum sodium may be normal or slightly low despite the marked hyperglycemia. A small anion-gap metabolic acidosis may be present secondary to increased lactic acid. Fluid replacement should initially stabilize the hemodynamic status of the patient (13 L of 0. The calculated free water deficit (which averages 910 L) should be reversed over the next 12 days (infusion rates of 200300 mL/h of hypotonic solution). Potassium repletion is usually necessary and should be dictated by repeated measurements of the serum potassium. In patients taking diuretics, the potassium deficit can be quite large and may be accompanied by magnesium deficiency. If the serum glucose does not fall, increase the insulin infusion rate by twofold. The patient should be discharged from the hospital on insulin, although some patients can later switch to oral glucose-lowering agents. Virtually all medical and surgical subspecialties are involved in the care of hospitalized patients with diabetes. Hyperglycemia, whether in a patient with known diabetes or in someone without known diabetes, appears to be a predictor of poor outcome in hospitalized patients. General anesthesia, surgery, infection, or concurrent illness raises the levels of counterregulatory hormones (cortisol, growth hormone, catecholamines, and glucagon) and cytokines that may lead to transient insulin resistance and hyperglycemia. These factors increase insulin requirements by increasing glucose production and impairing glucose utilization and thus may worsen glycemic control. Electrolytes, renal function, and intravascular volume status should be assessed as well. The goals of diabetes management during hospitalization are near-normoglycemia, avoidance of hypoglycemia, and transition back to the outpatient diabetes treatment regimen. Upon hospital admission, frequent glycemic monitoring should begin, as should planning for diabetes management after discharge. Glycemic control appears to improve the clinical outcomes in a variety of settings, but optimal glycemic goals for the hospitalized patient are incompletely defined. In a number of cross-sectional studies of patients with diabetes, a greater degree of hyperglycemia was associated with worse cardiac, neurologic, and infectious outcomes. In some studies, patients who do not have preexisting diabetes but who develop modest blood glucose elevations during their hospitalization appear to benefit from achieving near-normoglycemia using insulin treatment. Currently, most data suggest that very strict blood glucose control in acutely ill patients likely worsens outcomes and increases the frequency of hypoglycemia. Inpatient diabetes management teams consisting of nurse practitioners and physicians are increasingly common. The physician caring for an individual with diabetes in the perioperative period, during times of infection or serious physical illness, or simply when the patient is fasting for a diagnostic procedure must monitor the plasma glucose vigilantly, adjust the diabetes treatment regimen, and provide glucose infusion as needed. Hypoglycemia is frequent in hospitalized patients, and many of these episodes are avoidable.
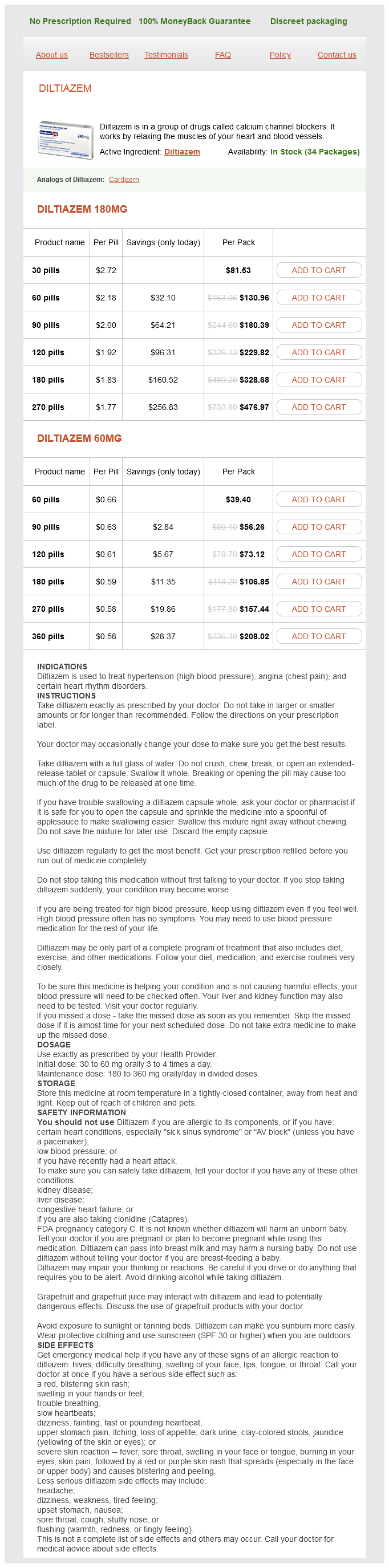
Diltiazem Dosage and Price
Diltiazem 180mg
- 30 pills - $81.53
- 60 pills - $130.96
- 90 pills - $180.39
- 120 pills - $229.82
- 180 pills - $328.68
- 270 pills - $476.97
Diltiazem 60mg
- 60 pills - $39.40
- 90 pills - $56.26
- 120 pills - $73.12
- 180 pills - $106.85
- 270 pills - $157.44
- 360 pills - $208.02
Even women who cannot walk benefit from swimming or water exercises symptoms to diagnosis buy diltiazem 60 mg low price, not so much for the effects on bone, which are quite minimal, but because of effects on muscle. For most patients we suggest participation in exercise regimes that the patient enjoys, in order to improve adherence. We also emphasize the importance of making exercise a social activity, again to improve adherence. Treatment thresholds depend on cost-effectiveness analyses but in the United States are >20% for 10-year major fracture probability and >3% 10-year hip fracture probability. It must be emphasized, however, that as with other diseases, risk assessment is an inexact science when applied to individual patients. Patients often accept risks that are higher than the physician might like out of concern for the (usually considerably lower) risks of adverse events of drugs. Antiresorptive Agents Estrogens A large body of clinical trial data indicates that various types of estrogens (conjugated equine estrogens, estradiol, estrone, esterified estrogens, ethinyl estradiol, and mestranol) reduce bone turnover, prevent bone loss, and induce small increases in bone mass of the spine, hip, and total body. The effects of estrogen are seen in women with natural or surgical menopause and in late postmenopausal women with or without established osteoporosis. For both oral and transdermal routes of administration, combined estrogen/progestin preparations are now available in many countries, obviating the problem of taking two tablets or using a patch and oral progestin. For transdermal estrogen, the commonly used dose supplies 50 g estradiol per day, but a lower dose may be appropriate for some individuals. Fracture Data Epidemiologic databases indicate that women who take estrogen replacement have a 50% reduction, on average, of osteoporosis related fractures, including hip fractures. The beneficial effect of estrogen is greatest among those who start replacement early and continue the treatment; the benefit declines after discontinuation to the extent that there is no residual protective effect against fracture by 10 years after discontinuation. A few smaller clinical trials have evaluated spine fracture occurrence as an outcome with estrogen therapy. They have consistently shown that estrogen treatment reduces the incidence of vertebral compression fracture. Other important relative risks included a 40% increase in stroke, a 100% increase in venous thromboembolic disease, and a 26% increase in risk of breast cancer. Subsequent analyses have confirmed the increased risk of stroke and in a substudy showed a twofold increase in dementia. Benefits other than the fracture reductions noted above included a 37% reduction in the risk of colon cancer. For example, out of 10,000 women treated with estrogen-progestin for 1 year, there will be 8 excess heart attacks, 8 excess breast cancers, 18 excess venous thromboembolic events, 5 fewer hip fractures, 44 fewer clinical fractures, and 6 fewer colorectal cancers. There was no effect of hormone treatment on the risk of uterine cancer or total mortality. The relative benefits and risks of unopposed estrogen in women who had hysterectomies vary somewhat. They still show benefits against fracture occurrence and increased risk of venous thrombosis and stroke, similar in magnitude to the risks for combined hormone therapy. The data suggest that at least some of the detrimental effects of combined therapy are related to the progestin component. In addition, there is the possibility, suggested by primate data that the risk accrues mainly to women who have some years of estrogen deficiency before initiating treatment. However, the majority of estrogen (and androgen) effects on bone resorption are mediated indirectly through paracrine factors produced by osteoblasts. Progestins In women with a uterus, daily progestin or cyclical progestins at least 12 days per month are prescribed in combination with estrogens to reduce the risk of uterine cancer. Medroxyprogesterone acetate and norethindrone acetate blunt the high-density lipoprotein response to estrogen, but micronized progesterone does not. Neither medroxyprogesterone acetate nor micronized progesterone appears to have an independent effect on bone; at lower doses of estrogen, norethindrone acetate may have an additive benefit. On breast tissue, progestins may account for the increase the risk of breast cancer with combination treatment. Bazedoxifene protects the uterus and breast from effects of estrogen and makes the use of progestin unnecessary. Tamoxifen reduces bone turnover and bone loss in postmenopausal women compared with placebo groups. These findings support the concept that tamoxifen acts as an estrogenic agent in bone. The breast cancer prevention trial indicated that tamoxifen administration over 45 years reduced the incidence of new invasive and noninvasive breast cancer by ~45% in women at increased risk of breast cancer. Tamoxifen increases the risk of uterine cancer in postmenopausal women, limiting its use for breast cancer prevention in women at low or moderate risk. Raloxifene (60 mg/d) has effects on bone turnover and bone mass that are very similar to those of tamoxifen, indicating that this agent is also estrogenic on the skeleton. Raloxifene reduces the occurrence of vertebral fracture by 3050%, depending on the population; however, there are no data confirming that raloxifene can reduce the risk of nonvertebral fractures >8 years of observation. In a further study raloxifene had no effect on heart disease in women with increased risk for this outcome. In contrast to tamoxifen, raloxifene is not associated with an increase in the risk of uterine cancer or benign uterine disease. Raloxifene increases the occurrence of hot flashes but reduces serum total and low-density lipoprotein cholesterol, lipoprotein(a), and fibrinogen. Raloxifene with positive effects on breast cancer and vertebral fractures has become a useful agent for the treatment of the younger asymptomatic postmenopausal woman.