General Information about Diamox
It also needs to be famous that Diamox should not be used in folks with a history of allergies to sulfonamide drugs or these with extreme liver or kidney illness. It can be not recommended for pregnant or breastfeeding ladies, as its safety in these populations has not been established.
Epilepsy is a disorder characterised by recurrent seizures, and Diamox is typically used as an adjuvant remedy for treating certain types of epilepsy. It works by inhibiting carbonic anhydrase in the mind, which helps to lower the excitability of nerves, thus decreasing the frequency of seizures. However, it should be noted that Diamox isn't effective for all sorts of epilepsy and may only be used in consultation with a doctor.
Craniocereberal hypertensia, also referred to as idiopathic intracranial hypertension, is a situation characterized by elevated strain contained in the cranium. This can cause severe complications, vision modifications, and even permanent vision loss if left untreated. Diamox is commonly prescribed in combination with other medications to scale back the strain within the cranium, providing relief to the signs of craniocereberal hypertensia.
When taken as directed, Diamox is mostly secure and well-tolerated. However, like all medicine, it could cause some unwanted effects, including nausea, loss of appetite, tingling sensation in the fingers and toes, and elevated urination. These side effects are usually delicate and resolve on their very own, but when they persist or turn into bothersome, it is important to seek the assistance of a health care provider.
Another widespread use of Diamox is in the therapy of glaucoma, a situation that causes elevated strain inside the attention, which may lead to imaginative and prescient loss. By inhibiting the production of fluid within the eye, Diamox helps to reduce the stress, thus defending the optic nerve and preserving vision.
Diamox, also referred to as Acetazolamide, is a weak diuretic used for treating numerous medical situations such as edematous syndrome, craniocereberal hypertensia, glaucoma, epilepsy, and mountain illness. It belongs to a class of medicine referred to as carbonic anhydrase inhibitors, and it really works by inhibiting the motion of carbonic anhydrase enzyme within the kidneys, leading to increased removing of sodium, potassium, and bicarbonate within the urine.
In conclusion, Diamox is a valuable medication used for the remedy of various medical circumstances, including edematous syndrome, craniocereberal hypertensia, glaucoma, epilepsy, and mountain illness. It works by inhibiting carbonic anhydrase, which ends up in increased elimination of sodium, potassium, and bicarbonate within the urine, offering aid to the signs of these situations. While it may trigger some side effects, Diamox is generally secure and efficient when taken as directed, and folks should seek the advice of their physician earlier than starting the therapy.
One of the primary makes use of of Diamox is to deal with edematous syndrome, which is a situation characterised by excessive fluid accumulation in the body tissues. This can happen because of numerous causes such as coronary heart failure, kidney disease, or liver disease. By inhibiting carbonic anhydrase, Diamox helps to reduce the surplus fluid within the physique, thus relieving the signs of edema.
In addition to the above medical circumstances, Diamox is also used for the prevention and therapy of mountain sickness. When at high altitudes, the physique might experience a decrease in the oxygen provide, leading to the symptoms of mountain sickness, corresponding to headache, nausea, and shortness of breath. Diamox works by stimulating respiration, increasing the amount of oxygen intake, and preventing the occurrence of mountain sickness.
None of the studies reported was blinded medications you can buy in mexico cheap 250mg diamox amex, and a randomization scheme was not used. The authors also have been criticized for excluding patients after randomization because of injuries considered too minor (no operative therapy) or too severe (Revised Trauma Score of 0). Exclusion of these patients may invalidate the statistical approach used and increase the difficulty of the clinician seeking guidance from this work. Finally, time spent in the trauma center by these hypotensive patients with injuries requiring operation was surprisingly long. Although the resuscitation groups described differed statistically in vital signs and hematologic parameters, it is unclear whether the differences observed had clinical significance. We await additional data on the military approach to resuscitation, which requires innovation and effectiveness in austere environments. Another clinical indicator for fluid resuscitation is decreasing mentation without evidence of head injury. In many settings, no fluids are administered in the presence of a strong radial pulse and normal mentation. Indicators for intervention are pulse deterioration or decreasing level of consciousness. When fluids are given, a number of smallvolume colloids with high tonicity or colloids in combination with saline solution are being investigated. Even early hospital resuscitation is designed to emphasize the use of blood products and minimize crystalloids and nonblood colloids in the setting of major injury. Clinical Pathway-Early Resuscitation In all of the preclinical and clinical work described, the mechanism of injury and survival remains unclear. Among considerations is the impact of fluid resuscitation on early clot formation in the setting of uncontrolled hemorrhage. Fluid resuscitation may contribute to dilution of clotting factors in the setting of exaggerated bleeding in uncontrolled hemorrhage. Coagulopathy proportional to volume of injured tissue and severity of shock may be seen even before resuscitation fluids are provided. This problem is best seen as injury with blood loss occurring in the absence of surgical or mechanical hemostasis or the "control" provided by regulated blood removal through a vascular cannula. It is unclear whether a vascular injury after a torso gunshot wound and a shattered spleen after an automobile crash are different in this regard. The message from all of the studies is that elevation of the blood pressure to normal or supranormal levels results in resumption of bleeding from the uncontrolled site, and rebleeding leads to recurrent shock and death of the experimental animal. Other work shows that animals subjected to shock could be successfully resuscitated at lower than "normal" mean arterial pressures if the bleeding site was controlled as part of the resuscitation program. Shock victims resuscitated with electrolyte solutions are subject to progressive hemodilution, and this may lead to death. The lessons that clinicians should learn from this body of data are as follows11,100,133: 1. Blood pressure levels are convenient but possibly misleading endpoints for shock resuscitation in that resuscitation to normal or supranormal pressures may be harmful if the effort delays 380 Pa rt 2 Critical Care Cardiovascular Disease operation to control bleeding or the pressure elevation causes rebleeding. Blood loss is increased in the setting of significant soft tissue insults combined with shock. Resuscitation of traumatic shock, similar to fluid management of a burned patient, requires repeated observation, judgment, and skill and cannot be accomplished by recipe or formula. Routine monitoring includes frequent vital signs, continuous electrocardiogram, and pulse oximetry with assessment of core body temperature. Arterial blood gas analysis is obtained in all patients presenting in traumatic shock. Patients with major torso trauma with evidence of shock (early systolic blood pressure <90 mm Hg and/or base deficit 6 mEq/L) and who require ongoing resuscitation should have a central venous catheter placed while they are in the emergency department. Differential diagnosis of cardiovascular insufficiency after blunt trauma includes tension pneumothorax, myocardial contusion or infarction, pericardial tamponade, and infrequently, air embolus. These investigators recommend hypotensive resuscitation to systolic blood pressure above 90 mm Hg and heart rate below 130 beats/ min with moderate volume loading until hemorrhage control is accomplished. They recommend this approach as standard care for patients with penetrating trauma and believe it is most likely safe as well for patients with blunt torso trauma who do not have significant coexistent brain injuries. Earlier empiric blood transfusion is indicated in patients, especially the elderly, who arrive in severe shock or have injuries associated with significant bleeding, such as vertical shear pelvic fractures or bilateral femur fractures. Institution protocols for massive transfusion should be established and used in these patients. Coagulopathy is among the complications of massive blood and fluid administration. Presumptive factor replacement is usually not indicated in the early phase of resuscitation, but it may be appropriate in patients with massive hemorrhage caused by significant intracavitary bleeding or an unstable pelvic fracture. Hemorrhage control is of paramount importance in initial management of patients with major torso trauma who arrive in shock. Simple clinical goals are provided which are modified based on observed patient response. Periodic urinary bladder pressure measurements should be obtained to monitor for the onset of abdominal compartment syndrome. Urinary bladder pressure of 25 mm Hg or higher indicates significant abdominal hypertension and the need to consider decompressive laparotomy. If they are not intubated and require ongoing volume loading, intubation should be considered because worsening pulmonary function is likely. If intubated and ventilator settings include positive end-expiratory pressure of 12 cm/H2O or higher, the effects of high mean airway pressure on cardiac function may become important. Laboratory variables, including hemoglobin, blood gas data, and coagulation parameters, should be determined every 4 hours and possibly more frequently until the patient is fully resuscitated and stable. There is no need to increase cardiac filling pressures to high levels in responsive patients, but the hemoglobin level should be maintained at 10 g/dL or higher during acute resuscitation where bleeding may still be ongoing.
A comprehensive review of spinal pain and the role of neural blockade in its treatment is provided by Rathmell in Chapter 44 symptoms ibs cheap diamox 250 mg amex. In the older person, degenerative central canal and lateral recess stenosis may be consequent to hypertrophy of the ligamentum flavum or zygapophyseal (facet) joints, vertebral body osteophytes or disc protrusion, or spondylolisthesis. The impact of degenerative changes may be compounded in a congenitally narrow canal or when associated with acquired conditions resulting from trauma, previous surgery, or medical comorbidities such as malignant neoplasia, Paget disease of bone, ankylosing spondylitis and vertebral compression fracture. Lateral recess or intraforaminal stenosis may result in radicular nerve root pain, due to compression of the exiting nerve root or the lower nerve root descending within the lateral recess. Degenerative spinal stenosis most commonly affects the L3L4 and L4L5 spinal segments. A review of foraminal stenosis indicated that the incidence of nerve root involvement was L5 (75%), L4 (15%), L3 (5%), and L2 (4%), relating to larger size of the L5 nerve root and its associated dorsal root ganglion relative to the exit foramen and increased frequency of disc degeneration and spondylosis at L4 and L5 (76). Foraminal stenosis may be static or dynamic, with lumbar flexion increasing (12%) and extension decreasing (15%) the size of the foramen. Hence, nerve root compression may be intermittent, depending on posture and activity. In one study, the incidence of foraminal nerve root compression was 21% in neutral, 15% in flexed, and 33% in extended positions (77). Exacerbation of leg pain during spine extension should therefore prompt consideration of foraminal stenosis. Imaging findings should always be correlated with clinical symptoms and examination. Jenis and An (76) suggest that plain radiographic dynamic flexion and extension studies may be misleading because of the oblique orientation of the lower lumbar intervertebral foramina. Myelography may not detect lateral pathology because of termination of the dural sheath, which prevents contrast medium from reaching the lateral nerve root sheath. Magnetic resonance changes suggestive of foraminal stenosis are reduction in foramen dimensions and loss of perineural fat in T1weighted images. Important conditions, including malignant neoplasia and infection, should be considered and excluded and the patient carefully evaluated for evidence of any neurologic deficit, in order to enable timely referral and treatment that may prevent permanent or progressive impairment. However, a prospective 10-year study of the outcomes of spinal decompressive surgery (78) by Amundsen et al. Conservative care was an alternative for patients with mild to moderate symptoms, resulting in 50% achieving a reduction in symptoms after 3 months; good results could still be obtained from surgery after failure of a trial of conservative care. Also, there was no difference in claudication at 4 years between surgical and conservatively treated groups, and more patients reported back pain at 4 years after operative intervention. There was an overall decrease in claudication symptoms from 90% at baseline to 20% after 10 years. As aging progresses, responses become less predictable, with wide variability in response to medications and interventions being the result of the overlay of purely age-based changes on those related to evolving medical comorbidities. Age-related changes in the impact of neuraxial block relate to altered function of cardiovascular, respiratory, and nervous systems, and also to increase in upper height of block. Following neuraxial block, hypotension and bradycardia are more frequent in the older patient, related to higher dermatomal levels of analgesia and sympathetic block after dose-equivalent spinal and epidural procedures; these cardiovascular changes pose greater risk to older individuals with reduced cardiac reserve (8188). Increased hypotension may be attributable to an increase in the upper level of analgesia with age, seen after epidural bupivacaine 0. With neuraxial block, the older patient is less able to compensate for hypovolemia or the redistribution of blood flow to the lower limbs and splanchnic circulation, due to decreased cardiac reserve and reduced sensitivity of the -adrenergic system and baroreceptor reflexes. Bradycardia may occur as a consequence of neuraxial cardiac sympathetic block at T1T4, age-related reduction in baroreceptor reflex mediated heart rate responses to hypotension or reflex slowing of heart rate in response to decreased venous return that relates to decreased atrial and pacemaker stretch and decreased ventricular mechanoreceptor reflex response. Judicious administration of intravenous fluids and vasopressors is required, taking care to avoid the fluid overload that may emerge as the neuraxial block regresses and the intravascular space contracts. Both local anesthetic dose and solution volume influence the upper epidural block height in the older patient, as in younger patients (see Chapter 11 on epidural blockade by Veering and Cousins). The age-related increase in upper block height after a fixed dose of local anesthetic may be the consequence of a number of factors (88). There may be decreased loss of epidural solution related to sclerosis and calcification of intervertebral foramina, or reduced epidural fat and decreased resistance to flow within the epidural space. In addition, greater flux of epidural solutions across the dura may be due to increased size of arachnoid villi and changes in the connective tissue matrix with age. Variability in age-related response with changes in solution volume may result in considerable interindividual variability in epidural block height in the older person. However, significant complications can arise even with small doses of drugs administered transforaminally (see Chapter 50). Recent reviews provide a more comprehensive overview of those changes in pharmacokinetics and pharmacodynamics in older patients that result in an increased sensitivity to both the therapeutic and adverse effects of many Neural Blockade Options in the Older Age Group Neural blockade and neuromodulatory techniques are potentially helpful in the management of pain associated with many of the most common conditions affecting the older age group. The subsections immediately following touch upon the value of these techniques in specific contexts such as low back pain, angina, peripheral vascular disease, and peripheral nerve Chapter 48: the Treatment of Pain in Older Patients 1209 injury. Comprehensive surveys of interventions related to musculoskeletal pain are described by Prager et al. Low Back Pain Low back pain has many causes, as discussed above and in Chapter 44. In the older age group, degenerative changes associated with osteoarthritis, spondylosis, and osteoporosis are common causes of back pain. Low back pain due to facet joint disease can be diagnosed by means of medial branch blocks and, if appropriate, radiofrequency lesions can be performed. This is a simple day case procedure that is well tolerated in the older age group. Further details on this and other spinal procedures are provided in Chapter 42 on percutaneous neurodestructive techniques by Niv and Gofeld, and Chapter 44 on spine pain by Rathmell. Back and leg pain associated with foraminal stenosis may be treated with epidural or transforaminal steroid and local anaesthetic injection.
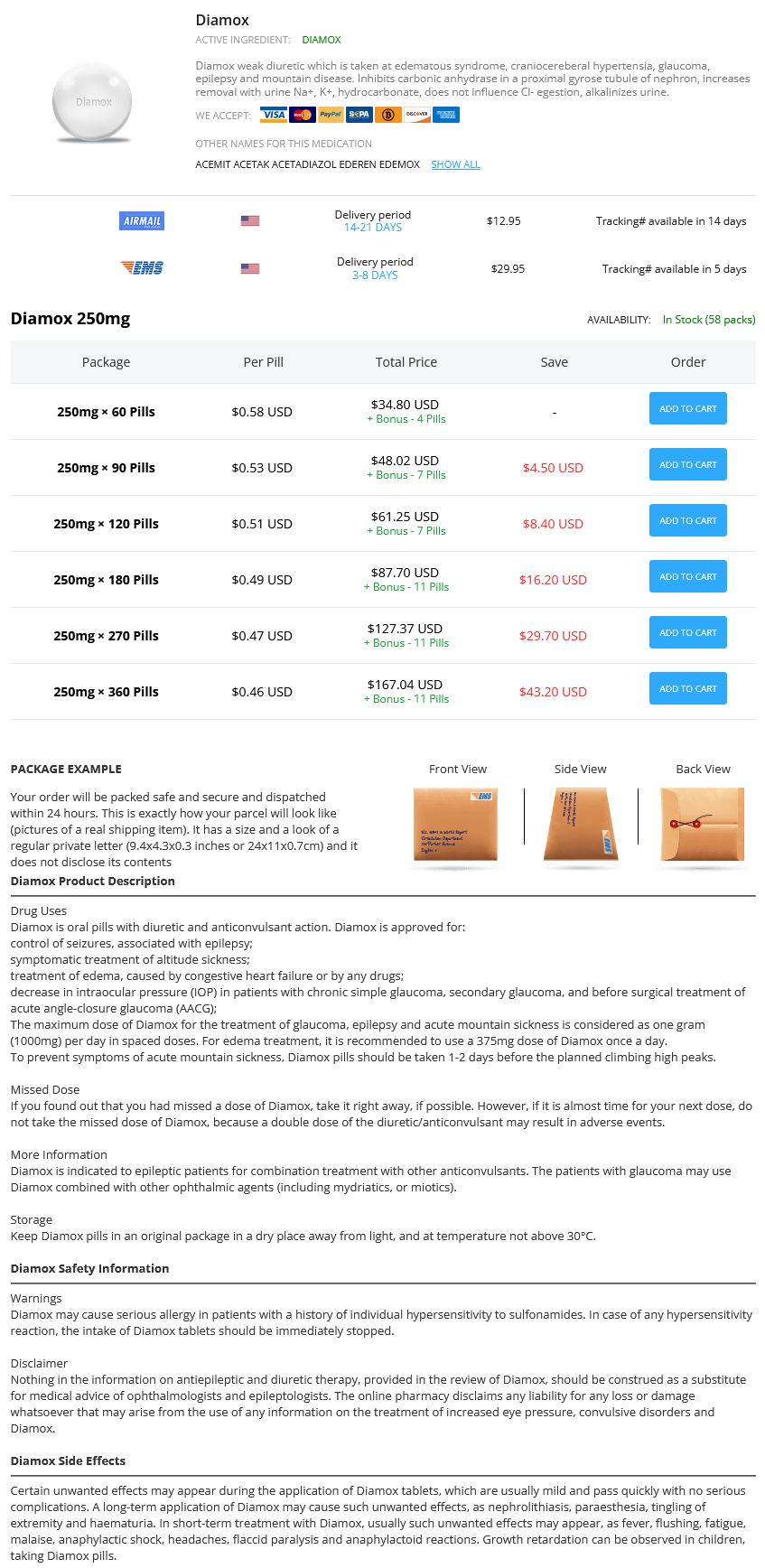
Diamox Dosage and Price
Diamox 250mg
- 60 pills - $34.80
- 90 pills - $48.02
- 120 pills - $61.25
- 180 pills - $87.70
- 270 pills - $127.37
- 360 pills - $167.04
Intermittent motion of the cardiac lead may also result in increased ventricular ectopy symptoms 9 weeks pregnant cheap diamox, with a premature ventricular contraction morphologic pattern that is similar to the morphologic pattern of the paced complex. Bleeding and Hematoma Hematoma is a common complication of pacemaker implantation, with an increased risk among patients receiving anticoagulation. Although not life-threatening, a large hematoma can be quite painful, result in significant blood loss, and increase the risk of infection. Placement of a tight pressure dressing over the site, immobilization of the ipsilateral arm with a sling, and temporary discontinuation of anticoagulation are often effective. When concomitant infection cannot be excluded, open wound exploration in a sterile operative setting should be considered. Needle aspiration of a hematoma should never be attempted at the bedside because this increases the risk of infection. Precautions should be taken to reduce the risk of bleeding preoperatively and postoperatively. As with any surgical procedure, the risk of bleeding associated with device implantation must be weighed against the risk of interruption of anticoagulation. In recent years, there has been a dramatic shift from official guidelines Pneumothorax Venous access may be obtained through subclavian or axillary puncture, as well as direct cephalic vein cut-down. Complications related to venous entry include bleeding, arterial injury caused by inadvertent arterial puncture, pneumothorax, hemothorax, thrombosis, air embolism, arteriovenous fistula, and brachial plexus injury. The risk of pneumothorax related to subclavian venous puncture is 1% to 2%125,135; this risk may be reduced by contrast venography before venipuncture. Pneumothorax typically presents early after the procedure, usually within 24 hours. Symptoms include chest pain, shortness of breath, or respiratory distress, which may be associated with hypotension or hypoxemia. A, A 12-lead electrocardiogram demonstrating sinus rhythm with synchronous ventricular pacing in a patient who had just undergone dual-chamber pacemaker placement. The paced morphologic pattern demonstrates a "left bundle branch block" appearance in lead V1 (red star) with a leftward axis, consistent with normal lead position. B, A 12-lead electrocardiogram in the same patient demonstrating a "right bundle branch block" morphologic pattern in lead V1 (red star) with a rightward axis, suggestive of lead perforation through the interventricular septum. C, Telemetry strip showing intermittent loss of ventricular capture shortly thereafter, caused by progressive migration of the lead tip. There are sinus P waves with ventricular capture (green stars) and failure to capture (red stars) with pauses truncated by ventricular escape complexes (blue stars). However, most operators perform pacemaker implantation if the international normalized ratio is in excess of 3. A growing body of literature suggests device insertions can also be performed safely in patients taking novel oral anticoagulants,147 but randomized data are not yet available. Hematologic evaluation is recommended and transfusions may be necessary when pacemaker therapy is urgently required. Inadvertent Lead Placement in the Left Ventricle Very rarely, a ventricular lead may be errantly placed within the left ventricle. Twelve-lead electrocardiography typically shows a right bundle branch block morphologic pattern in lead V1 during ventricular pacing, and lateral chest radiography demonstrates an abnormally posterior lead position. Left ventricular access introduces significant risk of arterial thromboembolism and should be corrected immediately. A decision between lifelong anticoagulation versus advanced extraction techniques is required for chronically implanted left ventricular leads. The lead tip extends to the lateral border of the cardiac silhouette, well beyond the typical border of the right ventricle (black arrow). Arrhythmias the most common arrhythmias occurring after pacemaker implantation are ventricular ectopic beats, particularly in the very early postoperative period. However, a change in lead position should be excluded by chest radiograph and bedside pacemaker analysis. Thrombosis Subclavian or axillary venous thrombosis may be detected early or late after implantation and can be either asymptomatic or associated with upper extremity swelling and pain. This is typically managed with elevation and anticoagulation with heparin and then warfarin. More severe presentations of thrombosis, including superior vena cava syndrome or venous thromboembolic complications, are very rare. The edges of the hematoma at the site of pacemaker implantation are marked to follow the size and exclude continued expansion. This may require drainage when large, tense, and painful, particularly if there is a need for early anticoagulation or if infection cannot be excluded. Patients who have undergone device insertion or revision should not receive unfractionated or lowmolecular-weight heparin for at least 6 hours after completion of the procedure, and low molecular-weight heparin should be avoided in patients with significant renal insufficiency. Thrombocytopenia and anemia are relative contraindications to device implantation, but a platelet count less than 50,000/µL and hemoglobin less than 7. Damage to the insulation may also occur at a site beneath the pulse generator owing to abrasion, or the damage may be the result of a suture being placed directly on the lead itself, in lieu of a suture sleeve. Signs of insulation breaks include undersensing and reduced pacing lead impedance. Lead fracture typically requires replacement, but a localized insulation breach can often be repaired operatively using a silicone repair kit. A, Abnormal contour of ventricular lead is noted on posteroanterior chest radiograph. B, Lateral view reveals that the lead initially courses very posteriorly, inconsistent with a right ventricular location.