General Information about Deltasone
Deltasone is a medicine that falls underneath the class of corticosteroids, that are hormones produced by the adrenal glands. It is usually prescribed to reduce inflammation and alleviate signs in numerous circumstances corresponding to ulcerative colitis and bronchial asthma.
In ulcerative colitis, Deltasone is prescribed to reduce inflammation and relieve symptoms similar to belly pain, diarrhea, and rectal bleeding. It works by concentrating on the immune system and decreasing the production of chemical compounds that cause inflammation within the colon.
For bronchial asthma sufferers, Deltasone helps to scale back airway irritation and enhance respiration. It does so by reducing the manufacturing of mucus and swelling in the airways, making it simpler for air to flow in and out of the lungs.
Deltasone is out there in various types, together with tablets, liquid, and injectable kind. The dosage and length of remedy depend upon the precise situation being handled, the severity, and the patient's response to the medicine.
It is essential to notice that Deltasone should not be stopped abruptly, as it might possibly cause withdrawal symptoms such as fatigue, joint ache, and fever. The dosage should be progressively reduced beneath the supervision of a medical professional to keep away from these symptoms.
Like some other treatment, Deltasone is related to some potential unwanted effects. The most typical unwanted side effects include increased appetite, weight gain, temper modifications, difficulty sleeping, and an increased risk of infections. These side effects usually subside once the medication is discontinued or the dosage is lowered.
Before starting Deltasone therapy, it's essential to debate the potential risks and advantages with a healthcare supplier, especially if the patient has a historical past of allergic reactions or different medical circumstances.
In conclusion, Deltasone is a broadly used treatment for managing varied conditions that contain irritation. It is a potent anti-inflammatory drug that helps to cut back signs and enhance the quality of life for sufferers. However, it is important to use this treatment beneath the steerage of a medical professional and to concentrate to the potential unwanted aspect effects. With proper use, Deltasone may be an efficient and important therapy option for those affected by inflammatory conditions.
In some circumstances, Deltasone can also trigger extra severe unwanted aspect effects, including high blood pressure, diabetes, osteoporosis, and cataracts. It is essential to tell the physician of any pre-existing medical situations earlier than starting Deltasone therapy.
Deltasone is primarily used to treat conditions that involve irritation, including allergic reactions, bronchial asthma, rheumatoid arthritis, and sure skin problems. It is also helpful in managing circumstances such as ulcerative colitis, which is a type of inflammatory bowel illness, and multiple sclerosis, which is an autoimmune disorder.
One of the primary features of Deltasone is to suppress the immune system's response to inflammation, which is the body's natural response to injury or infection. By doing so, it helps to scale back redness, swelling, ache, and different symptoms associated with inflammation.
They are rich in a mixture of phospholipids allergy shots effective for cat allergies purchase discount deltasone, neutral lipids, and proteins that is secreted by exocytosis to form an alveolar-lining, surface-active agent called surfactant. After lung injury, they proliferate and restore both types of alveolar cells within the alveolus. Surfactant decreases the alveolar surface tension and actively participates in the clearance of foreign materials. Rings of smooth muscle are present in the knob-like interalveolar septa (see the next paragraph). Alveolar sacs usually occur at the termination of an alveolar duct but may occur anywhere along its length. Alveoli are surrounded and separated from one another by an exceedingly thin connective tissue layer that contains blood capillaries. The tissue between adjacent alveolar air spaces is called the alveolar septum or septal wall. Surfactant synthesis in the fetus occurs after the 35th week of gestation and is modulated by a variety of hormones, including cortisol, insulin, prolactin, and thyroxine. Without adequate secretion of surfactant, the alveoli would collapse on each successive exhalation. In addition, administration of cortisol to mothers with threatened premature delivery decreases neonatal mortality. Surfactant proteins help organize the surfactant layer and modulate alveolar immune responses. The alveolar surface forms a vulnerable biologic interface that is subject to many destabilizing surface forces and to continuous exposure to inhaled particles, pathogens, and toxins. The alveolar epithelium is composed of several specialized cells and their products, some of which play defensive and protective roles: In addition to phospholipids, hydrophobic proteins are necessary for the structure and function of surfactant. They are extremely thin squamous cells; they line most (95%) of the surface of the alveoli. This electron micrograph shows two alveolar spaces separated by an alveolar septum containing capillaries, some of which contain red blood cells. Photomicrograph of an alveolus for comparison with the alveolar wall as seen in an electron micrograph. Connective tissue cells and fibers that may be present between the two basal laminae widen the airblood barrier. It is thought that most gas exchange occurs across the thin portion of the barrier. The thick portion is thought to be a site in which tissue fluid can accumulate and even cross into the alveolus. Lymphatic vessels in the connective tissue of the terminal bronchioles drain fluid that accumulates in the thick portion of the septum. Alveolar macrophages remove inhaled particulate matter from the air spaces and red blood cells from the septum. Alveolar macrophages are unusual in that they func- the alveolar septum is the site of the airblood barrier. The airblood barrier refers to the cells and cell products across which gases must diffuse between the alveolar and capillary compartments. The thinnest airblood barrier consists of a thin layer of surfactant, a type I epithelial tion both in the connective tissue of the septum and in the air space of the alveolus. Alveolar macrophages are derived from blood monocytes and belong to the mononuclear phagocyte system (see page 181). Some engorged macrophages pass up the bronchial tree in the mucus and are disposed of by swallowing or expectoration when they reach the pharynx. Thus, at autopsy, the lungs of urban dwellers and smokers usually show many alveolar and septal macrophages filled with carbon particles, anthracotic pigment, and birefringent needle-like particles of silica. Alveolar macrophages also phagocytose infectious organisms such as Mycobacterium tuberculosis, which can be recognized in the cells in appropriately stained specimens. These bacilli are not digested by macrophages; however, other infections or conditions that damage alveolar macrophages can cause release of the bacteria and recurrent tuberculosis. In addition, recent evidence suggests that apoptosis of septal macrophages contributes to the development of emphysema. Collateral air circulation through alveolar pores allows air to pass between alveoli. Scanning electron microscopic studies of alveolar structure show openings in the interalveolar septa that allow circulation of air from one alveolus to another. These alveolar pores (of Kohn) can be of great significance in some pathologic conditions in which obstructive lung disease blocks the normal pathway of air to the alveoli. The alveoli distal to the blockage may continue to be aerated, via the pores, from an adjacent lobule or acinus. With the aid of surfactant protein, surfactant is distributed on the surface of epithelial cells lining the alveolus as a thin film that reduces the surface tension. The thin portion forms the airblood barrier and is responsible for most of the gas exchange that occurs in the lung. The thick portion of the interalveolar septum plays an important role in fluid distribution and its dynamics. Note the macrophage in the thick portion that extends its processes into the lumen of the alveolus. This high-magnification micrograph shows the thin portion of the air blood barrier where it consists of type I alveolar cells, capillary endothelium, and the fused basal lamina shared by both cells. In the thick portion, the type I alveolar cell (arrows) rests on a basal lamina, and on the opposite side is connective tissue in which collagen fibrils and elastic fibers are evident. One set of lymphatic vessels drains the parenchyma of the lung and follows the air passages to the hilum.
The diagnosis of the underlying cause of the collapse may not be immediately obvious allergy medicine insomnia deltasone 20 mg buy amex. As has been emphasised in this section, resuscitation must begin even if the diagnosis is unclear. The differential diagnosis is not extensive, but in this clinical situation rational thought often deserts us. Prompt introduction of appropriate resuscitation may make the difference between the woman living or dying and give the time necessary to make the correct diagnosis. Progressively the woman complains of feeling short of breath or finding it difficult to breathe and becomes more anxious and dyspnoeic before proceeding rapidly to respiratory arrest. The close correlation between the administration of local anaesthetic and the progressive respiratory distress in the absence of circulatory disturbance confirms the diagnosis. A more truly toxic effect occurs with intravascular injection of a local anaesthetic agent, again typically with the insertion or topping up of an epidural block. Pregnant women appear to be more susceptible because of increased vascularity in the vessels around the epidural space and the increased pressures in the subarachnoid and epidural spaces that occur with contractions. Signs and symptoms usually occur within minutes of the injection of local anaesthetic. Respiratory paralysis follows, and cardiac arrest may occur as a result of anoxia and/or myocardial depression. However, collapse in the puerperium is more common, principally due to postpartum haemorrhage. The symptoms and signs of hypovolaemia (shock) may develop rapidly with progressive loss of consciousness as the blood pressure falls. It should be remembered that in severe haemorrhage there may be multiple factors contributing to the blood loss. For example, blood loss from perineal trauma may add to the bleeding from an atonic uterus, which can be aggravated by a developing coagulopathy due to consumption of clotting factors. Blood samples for full blood count, group and screen, coagulation screen, and renal and liver function tests should be taken right after inserting large bore cannulas. Once again it is important to emphasise that resuscitation must be proceeding hand in hand with diagnosis. A flow chart for the diagnosis of the woman collapsing in the puerperium is shown in. The causes of collapse are listed in Box 1 and will be covered in this sequence in this chapter. If significant bleeding continues despite the application of pressure, the cervix must be examined for lacerations. In a collapsed woman this should be done under anaesthesia together with exploration of the uterine cavity. Uterine cause If vaginal and cervical traumas are excluded by examination, then either retained placenta or products of conception or a poorly retracted lower segment are the likely causes of the bleeding. Gentle exploration of the uterine cavity digitally or using a large, blunt curette will allow the removal of any remaining tissue. Great care must be taken in these circumstances because of the ease with which the uterus can be perforated. If no tissue is detected it is likely that the lower segment is not retracting, and this is usually seen when the placenta has been implanted in the lower segment. Delayed collapse (more than 24 h after delivery and less than 6 weeks postpartum) Haemorrhage Eclampsia Infection/sepsis Pulmonary embolus Myocardial infarction Coagulopathy In most cases of postpartum haemorrhage sufficient to cause maternal collapse, coagulopathy will contribute to the blood loss. This is most often a consumptive coagulopathy due to depletion of clotting factors with excessive blood loss. Alternatively, it may be associated with sepsis or one of the coagulopathic conditions peculiar to pregnancy (pre-eclampsia, abruption, amniotic fluid embolism, intrauterine fetal death). Repeated blood testing will be necessary to monitor blood and blood product replacement during resuscitation. Input from a haematologist is required to expedite the testing, interpreting the results, and procuring replacement factors. In general, coagulopathy due to consumption is more readily corrected (once bleeding is arrested) than that due to a coagulopathic condition of pregnancy. The causes of postpartum haemorrhage can be classified as the four Ts: Tone or lack of it (uterine atony) Trauma (vaginal, cervical, uterine) Tissue (retained products of conception or blood clot) Thrombin or lack of it (coagulopathy) Blood loss Atonic uterus Uterine atony is more likely and should be anticipated if the labour has been prolonged, augmented, or the delivery assisted by forceps or vacuum. Bleeding will continue while the uterus remains atonic, and this must be corrected with oxytocics and abdominal or bimanual massage of the uterus. The contraction of the uterus must be palpated frequently to assess the effects of the measures taken. If the uterus fails to respond, rupture of the uterus, although rare, should be considered. Severe pre-eclampsia Coagulopathy is a feature of severe pre-eclampsia and is usually preceded by a progressive fall in the platelet count. It is not usually of sufficient severity alone to cause collapse, but it may be a contributing factor, as described previously. Genital tract trauma If the uterine fundus is well contracted when palpated, bleeding must be coming from the lower segment of the uterus, the cervix, or the vagina. Palpate fundus of the uterus: Consistency Soft Firm Absent Diagnosis Atonic uterus, rarely rupture Genital tract trauma Uterine inversion 3.
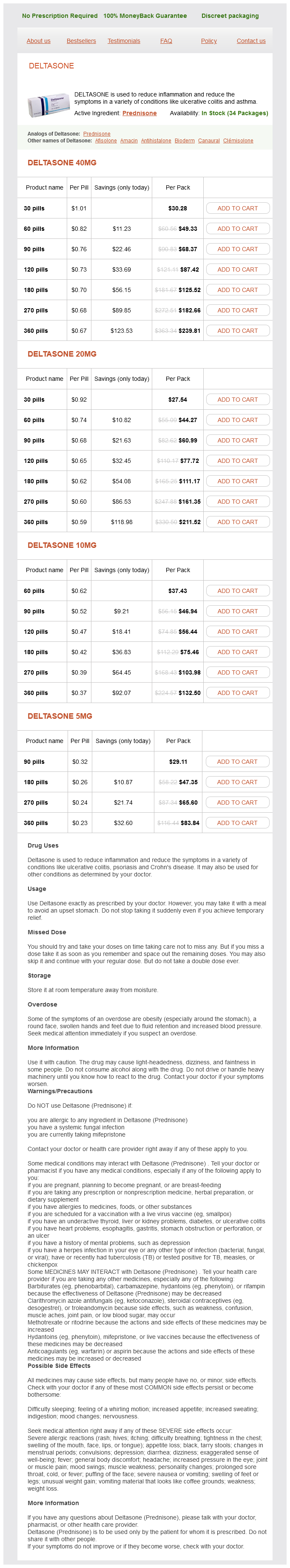
Deltasone Dosage and Price
Deltasone 40mg
- 30 pills - $30.28
- 60 pills - $49.33
- 90 pills - $68.37
- 120 pills - $87.42
- 180 pills - $125.52
- 270 pills - $182.66
- 360 pills - $239.81
Deltasone 20mg
- 30 pills - $27.54
- 60 pills - $44.27
- 90 pills - $60.99
- 120 pills - $77.72
- 180 pills - $111.17
- 270 pills - $161.35
- 360 pills - $211.52
Deltasone 10mg
- 60 pills - $37.43
- 90 pills - $46.94
- 120 pills - $56.44
- 180 pills - $75.46
- 270 pills - $103.98
- 360 pills - $132.50
Deltasone 5mg
- 90 pills - $29.11
- 180 pills - $47.35
- 270 pills - $65.60
- 360 pills - $83.84
The discontinuity of the endothelium is evident in two ways: · · Large fenestrae allergy medicine mold spores 10 mg deltasone purchase with amex, without diaphragms, are present within the endothelial cells. One hepatic sinusoid (top) displays a stellate sinusoidal macrophage (Kupffer cell). The remainder of the sinusoid as well as the other sinusoid is lined by thin endothelial cell cytoplasm. Surrounding each sinusoid is the perisinusoidal space (space of Disse), which contains numerous hepatocyte microvilli. Also present in the perisinusoidal space is a hepatic stellate cell (Ito cell) with a large lipid droplet and several smaller droplets. In congestive heart failure, the heart is unable to provide sufficient oxygenated blood to meet the metabolic requirements of many tissues and organs, including the liver, which is readily affected by hypoperfusion and hypoxia (low blood oxygen content). The hepatocytes in this zone are the last to receive blood as it passes along the sinusoids; as a result, these cells receive a blood supply already depleted in oxygen. Examination of a liver biopsy specimen from an individual with congestive heart failure shows a distinct pattern of liver necrosis. Hepatocytes in zone 3, which is located around the central vein, undergo ischemic necrosis. Typically, no noticeable changes are seen in zones 1 and 2, representing the periphery of a classic lobule. The multiple round vacuoles indicate lipid accumulation, and the atrophic changes are the result of dying hepatocytes undergoing autophagocytosis. Centrilobular necrosis as a result of hypoxia is referred to as cardiac cirrhosis; however, unlike true cirrhosis, nodular regeneration of hepatocytes is minimal. This photomicrograph shows a routine H&E liver biopsy specimen from an individual with congestive heart failure. Pathologic changes (referred to as ischemic necrosis) are most severe in hepatocytes in zone 3. Note the presence of multiple round vacuoles, which indicates extensive lipid accumulation. No noticeable changes are seen in the periphery of the lobule, which is zone 1 and much of zone 2. Processes of Kupffer cells often seem to span the sinusoidal lumen and may even partially occlude it. The presence of red cell fragments and iron in the form of ferritin in the cytoplasm of Kupffer cells suggests that they may be involved in the final breakdown of some damaged or senile red blood cells that reach the liver from the spleen. Some of the ferritin iron may be converted to hemosiderin granules and stored in the cells. This function is greatly increased after splenectomy when it is then essential for red blood cell disposal. Perisinusoidal Space (Space of Disse) the perisinusoidal space is the site of exchange of materials between blood and liver cells. The microvilli increase the surface area available for exchange of materials between hepatocytes and plasma by as much as six times. Because of the large gaps in the endothelial layer and the absence of a continuous basal lamina, no significant barrier exists between the blood plasma in the sinusoid and the hepatocyte plasma membrane. Proteins and lipoproteins synthesized by the hepatocyte are transferred into the blood in the perisinusoidal space; this pathway is for liver secretions other than bile. In the fetal liver, the space between blood vessels and hepatocytes contains islands of blood-forming cells. In cases of chronic anemia in the adult, blood-forming cells may again appear in the perisinusoidal space. The hepatic stellate cells (Ito cells) store vitamin A; however, in pathologic conditions, they differentiate into myofibroblasts and synthesize collagen. The perisinusoidal space (space of Disse) lies between the basal surfaces of hepatocytes and the basal surfaces of endothelial cells and Kupffer cells that line the sinusoids. Small, irregular microvilli project into this space from the basal surface of the hepatocytes. The other cell type found in the perisinusoidal space is the hepatic stellate cell (commonly called an Ito cell). An increased amount of perisinusoidal fibrous stroma is an early sign of liver response to toxic substances. The cytoplasm of hepatic stellate cells contains contractile elements, such as desmin and smooth muscle -actin filaments. During cell contraction, they increase the vascular resistance within the sinusoids by constricting the vascular channels, leading to portal hypertension. In addition, hepatic stellate cells play a role in remodeling the extracellular matrix during recovery from liver injury. From this collecting site, the fluid then enters lymphatic capillaries that travel with the other components of the portal triad. The lymph moves in progressively larger vessels, in the same direction as the bile. About 80% of the hepatic lymph follows this pathway and drains into the thoracic duct, forming the major portion of the thoracic duct lymph. The perisinusoidal space (D) is located between the hepatocytes (H) and the sinusoid. Such gaps allow easy passage of small substances between the sinusoid and the perisinusoidal space. It is then transported from the liver to the retina, where its stereoisomer 11-cis-retinal binds to the protein opsin to form rhodopsin, the visual pigment of rods and cones of the retina. In certain pathologic conditions, such as chronic inflammation or liver cirrhosis, hepatic stellate cells lose their lipid and vitamin A storage capability and differentiate into cells with characteristics of myofibroblasts.