General Information about Dapagliflozin
Clinical trials have shown dapagliflozin to be effective in reducing HbA1c ranges, a long-term measure of blood sugar control, and in enhancing different glycemic parameters corresponding to fasting and postprandial blood sugar levels. It has additionally been discovered to be helpful in decreasing weight and body mass index (BMI) in individuals with sort 2 diabetes. This is particularly important as a end result of obesity is a big threat issue for growing the situation and might make glucose administration tougher. Moreover, dapagliflozin has been shown to have a favorable safety profile, with minimal danger of hypoglycemia (low blood sugar levels) in comparison with other diabetes drugs.
Dapagliflozin belongs to a category of medications referred to as sodium-glucose cotransporter 2 (SGLT2) inhibitors. It works by blocking the absorption of glucose within the kidneys, leading to increased excretion of glucose in the urine. This mechanism of action is completely different from different diabetes drugs, which primarily work by rising insulin production or enhancing insulin sensitivity. By lowering the amount of glucose within the bloodstream, dapagliflozin helps to reduce blood sugar levels and improves glycemic control in individuals with kind 2 diabetes.
Forxiga is a prescription treatment and must be used underneath the steering of a healthcare skilled. It is out there in pill type and is normally taken as soon as a day, with or without meals. The recommended dosage might range based on individual needs, and it is important to comply with the physician's instructions fastidiously. The medicine should not be crushed or chewed, but swallowed whole with a glass of water.
Dapagliflozin, generally recognized by its brand name Forxiga, is a drugs used for the management of sort 2 diabetes. In recent years, the prevalence of sort 2 diabetes has been on the rise, making it a world health concern. As the variety of people living with this situation continues to extend, the need for efficient therapies turns into more obvious. Dapagliflozin has emerged as a promising medication within the fight towards type 2 diabetes and is gaining recognition among healthcare professionals and patients alike.
In addition to its glucose-lowering results, dapagliflozin has been found to have other potential benefits for folks with kind 2 diabetes. Research suggests that it might help to improve coronary heart and kidney well being by reducing the danger of cardiovascular events and delaying the development of diabetic kidney disease. These advantages are especially vital as a result of individuals with type 2 diabetes are at a higher risk of creating cardiovascular issues and kidney disease.
In conclusion, dapagliflozin, or Forxiga, is an efficient and protected option for the management of sort 2 diabetes. Its unique mechanism of motion and potential further advantages make it a useful addition to the prevailing arsenal of diabetes medicines. However, it is essential to do not forget that dapagliflozin just isn't a cure for kind 2 diabetes, and it ought to be used as part of a comprehensive therapy plan that contains a nutritious diet and common exercise. With proper use and monitoring, dapagliflozin might help individuals with type 2 diabetes obtain higher glycemic management and enhance their general health and well-being.
As with any medication, dapagliflozin may cause some unwanted facet effects. These embrace urinary tract infections, yeast infections, and increased frequency of urination. It is essential to debate any potential unwanted effects with a healthcare skilled and report any concerning symptoms promptly. Additionally, dapagliflozin could interact with different medicines, and it is crucial to inform a physician of all current drugs earlier than starting therapy.
Trientine is a less potent chelator than d-penicillamine cushings and diabetes in dogs 5 mg dapagliflozin mastercard, but the difference is not clinically important. Trientine produces little significant toxicity in patients with Wilson disease-apart from causing occasional gastritis and inducing iron deficiency, apparently by chelating dietary iron. Adverse effects of d-penicillamine resolve and do not recur during treatment with trientine. Trientine is highly effective, even in patients with advanced liver fibrosis or as initial treatment in children. The postulated mechanism of action is through the induction of metallothionein in enterocytes. The metallothionein has a greater affinity for copper than for zinc and preferentially binds copper from the intestinal contents. Once bound, the copper is not absorbed but is lost in the feces as enterocytes are shed during normal turnover. Zinc may interfere with lipid peroxidation and enhance the availability of glutathione. Problems with zinc therapy include gastritis, which is a common side effect, and uncertainty about dosing. Using a zinc salt other than zinc sulfate may minimize gastritis; most zinc salts are equally acceptable for the treatment of Wilson disease. Food interferes with the effectiveness of zinc, and some investigators recommend that no food be eaten for 1 hour before or after a dose of zinc is taken. An alternative approach is to be less rigorous about avoiding zinc at mealtimes and to titrate the dose according to the urinary copper excretion. Long-term studies suggest that zinc is more effective in neurologic Wilson disease than in hepatic Wilson disease. The adequacy of treatment is assessed by measurement of basal 24-hour urinary copper excretion, which should be high with either oral chelator (200 to 500 g/day or 3 to 8 mol/day) and low with zinc (30 to 75 g/day or 0. The patient must be asked specifically about general well-being and adherence to the drug regimen. With zinc treatment, adherence can be checked by measurement of 24-hour urinary zinc excretion (>2 mg/day) or serum zinc (>12. Elevated serum aminotransferase levels that were previously normal may signal nonadherence and evidence of ongoing hepatic damage. Patients diagnosed while still asymptomatic may be at greater than average risk for lapsing into nonadherence. For patients who present with decompensated chronic liver disease, combining zinc with a conventional chelator (preferably trientine) has become a popular treatment strategy even in the absence of extensive validation. This intensive short-term induction regimen is best suited to patients with severe hepatic or neurologic disease85 and remains semi-investigational. Ammonium tetrathiomolybdate was investigated as treatment of severe neurologic Wilson disease because, unlike d-penicillamine, it is not associated with early neurologic deterioration. A new formulation, bis-choline tetrathiomolybdate, has excellent stability and is pharmacologically equivalent to ammonium tetrathiomolybdate. More detailed information about the total-body disposition of copper and molybdate is needed. Studies in copper-loaded animals and in patients with Wilson disease indicate that copper enhances free radical production in tissues and may thereby cause liver damage. For pregnant patients with Wilson disease, treatment must be continued throughout pregnancy. Postpartum hepatic decompensation may occur if treatment is stopped completely during pregnancy. Although many pregnancies during treatment with d-penicillamine have been successful, the drug is officially classified as a teratogen. Occasional reports of severe collagen defects in the offspring of a patient treated with d-penicillamine may be caused in part by copper deficiency as a result of prolonged aggressive treatment, as well as the teratogenic effects of d-penicillamine. The safety of trientine during pregnancy is unknown, apart from favorable anecdotal reports. Judicious reduction of the dose of d-penicillamine or trientine by approximately 25% to 50% of the pre-pregnancy dose is advisable, especially if delivery by cesarean section is anticipated. An asymptomatic first-degree relative who is diagnosed on biochemical or genetic grounds and treated before any sign of clinical impairment generally has the best long-term outlook. Patients with early hepatic disease have a generally favorable prognosis provided treatment is consistent and well tolerated. The outcome is favorable, with 1-year survival rates of 80% to 90% and excellent survival beyond 1 year. Patients with Wilson disease who stop taking chelating treatment (or zinc) have a poor prognosis. Rapidly progressive hepatic decompensation has been observed and occurs on average within 3 years, and as early as 8 months, after treatment is stopped. The quality of life of patients with Wilson disease may be compromised by drug toxicity. Anecdotal observations suggest that damage to collagen may accrue over decades in patients who are maintained indefinitely on d-penicillamine, but the risk has not been assessed adequately. Deficiencies in trace metals may develop with the use of any chelator, but whether these deficiencies are clinically important is not yet clear. Abnormal iron metabolism, leading to hepatic iron overload and anemia, can be predicted if serum ceruloplasmin oxidase activity is zero. Patients should be encouraged to maintain a healthy lifestyle, including avoidance of alcohol and obesity. Targeted inactivation of copper transporter Atp7b in hepatocytes causes liver steatosis and obesity in mice. Analysis of a Wilson disease model demonstrates the link between copper and lipid metabolism.
The lesion was removed successfully but recurred twice over the next 10 years diabetes prevention management buy generic dapagliflozin 5 mg on-line, requiring additional surgical procedures and cryotherapy. Eventually, superficial corneal invasion developed and the patient was treated successfully with topical mitomycin C. Histopathology of conjunctival intraepithelial neoplasia showing almost full-thickness replacement of the epithelium by neoplastic squamous cells. From the normal conjunctival epithelium (to the right) to the tumor (to the left). Histopathology of conjunctival intraepithelial neoplasia showing abrupt transition between the normal epithelium and the thickened abnormal epithelium. Histopathology of conjunctival intraepithelial neoplasia showing abnormal epithelial cells with mitotic activity. Conjunctival intraepithelial neoplasia was documented histopathologically in each of these cases. Nodular vascular lesion arising from the superior limbus and secondarily invading the cornea in a 64-year-old man. This is an atypical location for squamous cell neoplasms; the majority arise in the interpalpebral area. Lesion with irregular, fleshy nodules in the peripheral cornea in a 61-year-old woman. Large, pedunculated lesion arising from limbal area and overhanging the cornea in an 85-year-old woman. Histopathologically, the lesion was confined to the epithelium and had not invaded the stroma despite marked elevation. It should be carefully mapped, depicted on a large drawing prior to surgical excision or other management. These cases were documented histopathologically to be conjunctival intraepithelial neoplasia. Diffuse conjunctival intraepithelial neoplasia with corneal invasion, simulating an inflammatory pannus in a 78-year-old man. Subtle involvement of the inferonasal quadrant of the cornea in a 69-year-old man. Involvement of nasal 70% of cornea with subtle conjunctival intraepithelial neoplasia in a 73-year-old man. Note the fine vertical line to the right separating the abnormal from the normal corneal epithelium. Corneal invasion of squamous cell carcinoma in a 60year-old African American woman. A rough summary of reported cases suggests that about 75% occur in men, 75% are diagnosed in older patients (60 years old), and more than 75% occur at the limbus. It occurs with greater frequency in patients with xeroderma pigmentosum, atopic eczema, and other conditions that predispose to epithelial malignancies (11). The dysfunction of T lymphocytes seen in these disorders may play a role in the malignant transformation of conjunctival epithelium (11). Mucoepidermoid carcinoma characteristically occurs in elderly individuals, usually over 70 years of age. However, it has been reported to originate in the caruncle and secondarily invade the orbit and paranasal sinuses (23). It is more aggressive than conventional squamous cell carcinoma, with a tendency toward intraocular and orbital invasion. The intraocular component has been known to produce a large intraocular mucinous cyst in the suprauveal space (29). It may have a more yellow, globular, cystic appearance than typical squamous cell carcinoma. In some cases, the mucinous component is not apparent in the original specimen, but can be more pronounced in the recurrence. Sometimes the mucinous cysts are not apparent in the epibulbar tumor, and only the intraocular component shows appreciable mucin production (27,28). Spindle cell carcinoma tends to be more locally invasive than standard squamous cell carcinoma and has a greater tendency to metastasize (34). One reported case metastasized to lung and bone; the patient expired 14 months after the original diagnosis (34). The treatment is similar to that of standard squamous cell carcinoma, but wider excision is advisable. An incisional biopsy to establish the diagnosis is not usually indicated unless the tumor is large and diffuse. In such instances, map biopsies, similar to that used for conjunctival involvement of sebaceous carcinoma, may be advisable. In addition, the depth of limbal invasion of squamous cell carcinoma can be estimated with high-frequency ultrasonography (ultrasound biomicroscopy). The tumor displays a wide array of clinical appearances and can be a circumscribed, gelatinous, sessile, papillomatous mass with varying amounts of leukoplakia. However, it can extend locally to cover the cornea and invade the orbit and globe. Intraocular invasion can cause uncontrollable glaucoma that may necessitate enucleation. Occasionally, squamous cell carcinoma can present as a diffuse, flat, poorly delineated neoplasm without distinct tumefaction (12). In such cases, it may be confused clinically with conjunctivitis, keratoconjunctivitis, scleritis, or pagetoid invasion of sebaceous carcinoma. Two less common, but aggressive variations of conjunctival squamous cell carcinoma, the mucoepidermoid and spindle cell forms, deserve special consideration. These account for fewer than 5% of cases of conjunctival squamous cell carcinoma (18).
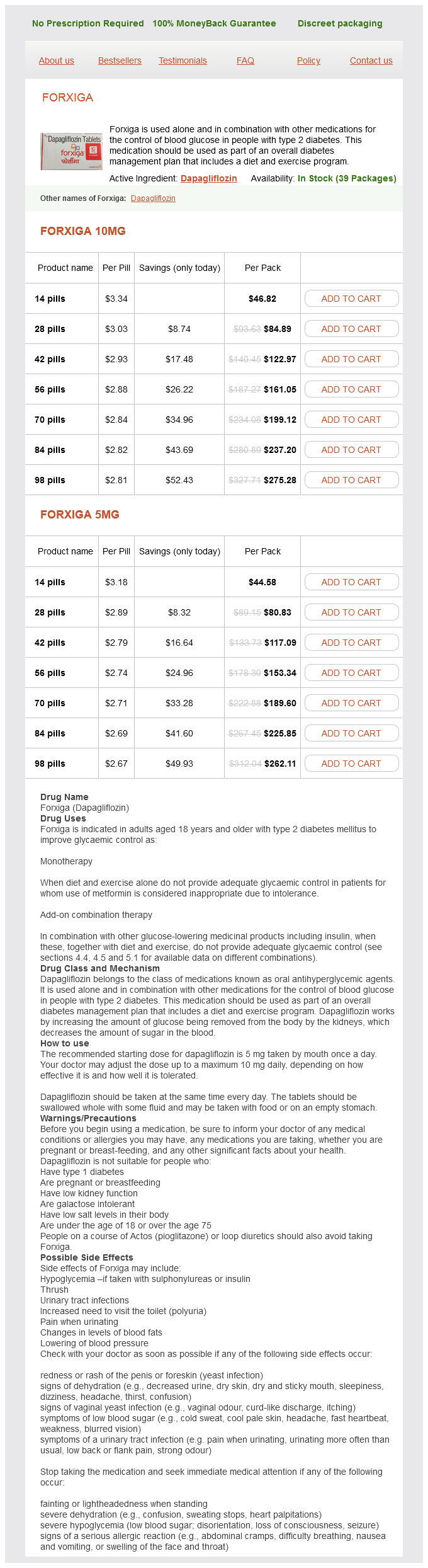
Dapagliflozin Dosage and Price
Forxiga 10mg
- 14 pills - $46.82
- 28 pills - $84.89
- 42 pills - $122.97
- 56 pills - $161.05
- 70 pills - $199.12
- 84 pills - $237.20
- 98 pills - $275.28
Forxiga 5mg
- 14 pills - $44.58
- 28 pills - $80.83
- 42 pills - $117.09
- 56 pills - $153.34
- 70 pills - $189.60
- 84 pills - $225.85
- 98 pills - $262.11
This tumor has no specific clinical features and may be impossible to differentiate clinically from other subcutaneous eyelid lesions diabetes symptoms journal buy dapagliflozin 5 mg free shipping. Pathology Histopathologically, the eyelid tumor has features identical to pleomorphic adenoma of the lacrimal gland. The glandular epithelial cells form islands or cords in a mucoid stroma, which often displays chondroid metaplasia. The epithelial cells form a double layer, with the inner layer being secretory and the outer layer myoepithelial in nature (2). Like pleomorphic adenoma of the lacrimal gland, areas of malignant transformation can be detected in the eyelid counterpart, although it is less common. Management the management of pleomorphic adenoma of the eyelid is complete surgical removal. Although eyelid lesions rarely undergo malignant change, benign mixed tumors in the extremities or back can metastasize locally and hematogenously (7). Histopathology of pleomorphic adenoma of eyelid, showing glandular, mesenchymal and chondroid elements. The three most often reported malignant eyelid tumors of sweat gland origin are mucinous sweat gland adenocarcinoma, eccrine sweat gland adenocarcinoma, and apocrine adenocarcinoma of the glands of Moll (13). Each type has overlapping clinical features, and the diagnosis is often not suspected clinically. Furthermore, they may be difficult to confirm histopathologically, because they may be similar to other primary malignancies and to metastatic adenocarcinoma to the eyelid. Mucinous sweat gland adenocarcinoma arises from the epidermal cells of eccrine sweat glands and is characterized by a high content of mucin (120). Eccrine sweat gland adenocarcinoma (also called "infiltrating signet ring carcinoma") is an unusual variant of adenocarcinoma of sweat gland origin that resembles mammary carcinoma histopathologically (5,2123). Apocrine adenocarcinoma can occur in areas of the skin where apocrine glands are most dense, such as the perianal region, axilla, and the external auditory canal (ceruminous glands). Pathology Mucinous sweat gland adenocarcinoma is characterized by lobules and cords of epithelial cells that float in pools of mucin, separated by thin fibrovascular septa (119). Less commonly, the mucin may be largely confined to the epithelial cells and not in the extracellular spaces. The epithelial cells can sometimes form ductules or acini, imparting an "adenocystic appearance. In some cells, a large vacuole displaces the nucleus, producing a characteristic signet ring appearance. These cells are said to be indistinguishable from those of the histiocytoid mammary carcinoma metastatic to the eyelid. In such cases, the diagnosis of a primary sweat gland neoplasm cannot be made until breast cancer has been excluded clinically. Apocrine adenocarcinoma is characterized by a glandular arrangement of large cells with abundant eosinophilic cytoplasm and evidence of decapitation secretion. They are identical to the apocrine adenocarcinoma that occurs in the axilla (2631). Clinical Features Each type of malignant sweat gland neoplasm begins as a small nodule that grows slowly and, if not controlled locally, has a capacity to recur locally and metastasize to region lymph nodes. Mucinous sweat gland adenocarcinoma develops in the head and neck region in 75% and in the periorbital area in 40% of cases. Patient ages have ranged from 8 to 84 years, but it is more common in older individuals, with a mean age at diagnosis of 63 years (5,14). Although most information is derived from case reports, Wright and Font (5) reported 21 cases and outlined the salient clinical and histopathologic features of mucinous sweat gland adenocarcinoma. It is more common in the lower eyelid and appears as a pink to blue, elevated nodule that may be solid or cystic. Eccrine sweat gland adenocarcinoma appears as a nodular, indurated subcutaneous mass that has an ill-defined, diffuse, infiltrating margin, and a blue to red color (2125). When it affects the periocular area, it is most common in the lower eyelid and extends toward the canthal region. Porocarcinoma is a variant of sweat gland carcinoma that arise from the eccrine secretory apparatus (17). In the eyelid area, apocrine adenocarcinoma develops from the apocrine glands of Moll near the base of the cilia. It is similar to other sweat gland and adnexal tumors, except that it is more likely to be located very near the eyelid margin corresponding to the glands of Moll. Management the best management of a malignant sweat gland neoplasm is wide surgical excision with frozen section or Mohs surgery to monitor the margins, similar to the management of basal cell carcinoma and other primary malignant eyelid tumors (15). However, incompletely excised lesions have a tendency toward local recurrence, regional lymph node metastasis and, rarely, systemic metastasis. A clinicopathologic study of 21 cases with histochemical and electron microscopic observations. Primary mucinous sweat gland carcinoma of the eyelid simulating metastatic carcinoma. Eccrine duct carcinoma of the eyelid mimicking meibomian carcinoma: clinicopathological study of a case. Signet ring carcinoma of the eccrine sweat gland in the eyelid, treated by radiotherapy alone. Histiocytoid variant of eccrine sweat gland carcinoma of the eyelid and orbit: report of five cases. Carcinoma of the apocrine glands at the base of eyelashes; a case report and discussion of histological diagnostic criteria. Apocrine adenocarcinoma of the eyelid with aggressive biological behavior: report of a case.