General Information about Combivent
The main advantage of Combivent Aerosol is that it provides the comfort of utilizing two drugs in a single inhaler. This implies that sufferers now not need to juggle a quantity of inhalers or take a number of medicines at different instances of the day. This is especially helpful for aged patients or those with cognitive impairments who might have difficulty maintaining monitor of multiple medications.
Another benefit of Combivent Aerosol is its fast onset of motion. The medicine begins working within minutes, providing rapid relief for sufferers experiencing shortness of breath or other COPD signs. This can be significantly useful during acute exacerbations, that are sudden, extreme worsening of COPD symptoms.
In conclusion, Combivent Aerosol is an efficient choice for sufferers with COPD who require more than one bronchodilator. Its convenient administration, quick onset of motion, and synergistic impact make it a useful addition to the therapy regimen for COPD. However, it is essential to follow your doctor's instructions and report any unwanted side effects or concerns while using this medicine. With proper and regular use, Combivent Aerosol might help sufferers handle their COPD signs and improve their total high quality of life.
It is essential to notice that Combivent Aerosol isn't appropriate for all COPD sufferers. Patients with sure medical conditions, similar to coronary heart illness or high blood pressure, may have to use caution when using this medicine. As with any prescription medication, it is important to debate your medical historical past with your physician before beginning Combivent Aerosol.
Combivent Aerosol is a mix medication that contains two bronchodilators - ipratropium bromide and albuterol sulfate. Bronchodilators are drugs that assist to chill out and widen the airways, making it easier for patients to breathe. Individually, ipratropium bromide and albuterol sulfate are effective bronchodilators, but when combined, they provide even larger advantages for patients with COPD.
COPD is a progressive lung disease that makes it troublesome to breathe
Combivent Aerosol is usually prescribed for sufferers who usually are not adequately controlled with a single bronchodilator. For these sufferers, adding a second bronchodilator can greatly enhance their symptoms and quality of life. It is important to notice that Combivent Aerosol isn't meant to switch different COPD drugs, such as inhaled corticosteroids or oxygen remedy, but quite to enhance them.
Chronic obstructive pulmonary disease (COPD) is a progressive lung illness that impacts tens of millions of individuals worldwide. It is characterised by obstruction of airflow, making it troublesome for patients to breathe. This condition can have a big influence on a affected person's quality of life, limiting their capacity to carry out daily duties and even leading to life-threatening problems. As such, effective management of COPD is crucial for bettering the overall health and well-being of sufferers. One of the therapies commonly used for COPD is Combivent Aerosol.
Like all drugs, Combivent Aerosol might trigger some side effects, although most patients tolerate it nicely. Common unwanted effects embrace dry mouth, cough, throat irritation, and headache. These symptoms are normally gentle and momentary, and most patients don't expertise them after utilizing the medication for some time.
The effectiveness of Combivent Aerosol has been demonstrated in quite a few scientific studies. In one study, sufferers using Combivent Aerosol confirmed vital improvements in lung function and breathlessness compared to those utilizing both ipratropium or albuterol alone. This confirms the synergistic impact of the 2 drugs in treating COPD.
Echogenic polyps less than 5 mm in size can be presumed to represent cholesterol polyps and no further imaging follow up is necessary medications known to cause miscarriage discount combivent 100 mcg buy. Moving the patient during scanning confirms the mobile nature of sludge, as it will change position when the patient moves. Gallstones usually produce a posterior shadow, which may be difficult to demonstrate when the stones are small. Moving the patient to different positions while scanning or jiggling the gallbladder with the ultrasound probe will help to change the position of stones. Gallbladder Carcinoma Definition Gallbladder carcinoma is an aggressive malignancy that arises from the gallbladder mucosa. Demographic and Clinical Features Although gallbladder cancer is uncommon, it is the most common malignancy of the biliary tract. Gallstone size over 3 cm is thought to increase the risk of carcinoma by a factor of 10. Other risk factors include chronic cholecystitis, chronic biliary infections, a typhoid carrier state, primary sclerosing cholangitis, an anomalous pancreaticobiliary junction, choledochal cyst, and "porcelain" gallbladder. Gallbladder polyps greater than 1 cm are also associated with a high risk of malignancy. Gallbladder carcinoma is largely asymptomatic until the advanced stages of disease, when nonspecific symptoms such as abdominal pain, weight loss, fever, and jaundice may occur. Pathology Gallbladder carcinoma most commonly arises in the fundus or neck of the gallbladder. It arises from dysplastic gallbladder mucosa through a progression from dysplasia to carcinoma in situ to invasive carcinoma, which is thought to occur over a long period of time, about 15 years. Long-standing inflammation, usually in the presence of gallstones, is felt to be the underlying etiology. The most frequent histologic type is adenocarcinoma, accounting for over 98% of cases. Less frequent histologic types include squamous, adenosquamous, and small-cell carcinoma. Tumor dissemination occurs mainly through the lymphatic pathways and by direct invasion of the liver. The latter is thought to result from direct venous drainage of the gallbladder into segment 4 of the liver. The portion of the gallbladder that contacts the liver lacks a serosal covering and there is continuity of the connective tissue between the two organs. Peritoneal dissemination may also occur once the tumor has penetrated the gallbladder wall. Polyps larger than 10 mm-particularly if solitary, sessile, and symptomatic-found in association with gallstones or in patients over 50 years of age raise concern for a neoplastic origin of the polyp and thus pose an increased risk of malignancy. The hepatic invasion is shown (arrowheads) as well as nodes in the hepatoduodenal ligament. After contrast administration, tumor enhancement is observed, more pronounced on the arterial phase, with an irregular outer margin. Polypoid lesions are usually of intermediate signal intensity on T1-weighted images and moderately hyperintense on T2-weighted images. Management/Clinical Issues Surgery is considered to be the only curative treatment for gallbladder carcinoma. It is estimated to be approximately 10% at 5 years in cases with serosal involvement with or without lymph node metastasis. Extended and complete resection in highly selected patients with advanced disease may increase survival up to 31%. Differential Diagnosis Adenomyomatosis: May be difficult to distinguish from gallbladder cancer when there is pronounced gallbladder wall thickening. Gallbladder polyps: Large gallbladder polyps and those associated with focal gallbladder wall thickening or adenopathy should raise concern for malignancy in the polyp. Xanthogranulomatous cholecystitis: Often indistinguishable from gallbladder carcinoma preoperatively because it may have associated extension into the adjacent liver. Gallbladder metastases: Generally occur in the setting of a known primary cancer and widespread metastasis. Gallstones larger than 3 cm are thought to increase the risk for carcinoma 10-fold. May present as a subhepatic mass, frequently with trapped gallstones, as asymmetric and irregular gallbladder wall thickening, or as a polypoid lesion. Gallbladder carcinoma update: multimodality imaging evaluation, staging and treatment options. Gallbladder Metastases Key Points Uncommon malignancy despite being the most common malignancy of the biliary tract. Definition Gallbladder metastases stem from tumor growth in the gallbladder due to the transmission of neoplastic cells from a primary tumor located elsewhere in the body. Malignant melanoma is the most frequent cause of gallbladder metastasis, accounting for up to 60% of all cases. Other primary tumors that have a tendency to involve the gallbladder include renal cell carcinoma and hepatocellular carcinoma. When symptomatic, gallbladder metastases from melanoma are reported to cause acute cholecystitis, obstructive jaundice, external biliary fistula, and hemobilia.
Lipid can also overflow into arterial vascular smooth cells medicine in the civil war order combivent uk, leading to the acceleration of atherosclerosis. Using 14 C-palmitate in combination with the insulin clamp technique [39], the antilipolytic effect of insulin has been shown to be markedly impaired in lean type 2 diabetic subjects, as well as in obese nondiabetic subjects [208]. After fatty acids enter the cell, they can be converted to triglycerides, which are inert, or to toxic lipid metabolites such as fatty acyl CoAs, diacylglycerol, and ceramide [4]. Using magnetic resonance spectroscopy, the intramyocellular triglyceride content has been shown to be increased in type 2 diabetic subjects [338,340]. Fatty acyl CoAs, which are known to inhibit insulin signaling [341,342], are also significantly increased in muscle in diabetic subjects [338,343]. However, there also is evidence that the mitochondrial defect is acquired, at least in part [349Â351]. Treatment of diabetic patients with pioglitazone markedly improves insulin sensitivity in association with a reduction in intramyocellular lipid and fatty acyl CoA concentrations. The decrement in muscle fatty acyl CoA content is closely related to the improvement in insulin-stimulated muscle glucose disposal [340,343]. Reduced intramyocellular fatty acyl CoA content with acipimox, a potent inhibitor of lipolysis, caused a similar improvement in insulin-mediated glucose disposal [338,339]. Increased intramyocellular levels of diacylglycerol [330,352] and ceramides [353,354] have been demonstrated in type 2 diabetic and obese nondiabetic subjects and shown to be related to the insulin resistance and impaired insulin signaling in muscle. Alpha cell and glucagon It long has been known that the basal plasma glucagon concentration is elevated in type 2 diabetic individuals [184Â186, 357,358]. There also is evidence that the liver is hypersensitive to the stimulatory effect of glucagon in hepatic gluconeogenesis [185]. The kidney: increased glucose reabsorption the kidney filters 162 g ([glomerular filtration rate = 180 L day-1] Ч [fasting plasma glucose = 900 mg L-1]) of glucose every day. Thus, an adaptive response by the kidney to conserve glucose, which is essential to meet the energy demands of the body, especially the brain and other neural tissues which have an obligate need for glucose, becomes maladaptive in the diabetic patient. Instead of dumping glucose in the urine to correct the hyperglycemia, the kidney chooses to hold on to the glucose. Even worse, the ability of the diabetic kidney to reabsorb glucose is augmented by an absolute increase in the renal reabsorptive capacity for glucose. The current epidemic of diabetes is being driven by the epidemic of obesity [369]. Porte and colleagues [370Â373] were amongst the first to demonstrate that, in rodents, insulin was a powerful appetite suppressant. Obese individuals, both diabetic and nondiabetic, have moderate-to-severe insulin resistance with compensatory hyperinsulinemia. Nonetheless, food intake is increased in obese subjects despite the presence of hyperinsulinemia which should suppress the appetite. Therefore, one could postulate that the insulin resistance in peripheral tissues also extends to the brain. After glucose ingestion, two hypothalamic areas with consistent inhibition have been noted: the lower posterior hypothalamus, which contains the ventromedial nuclei, and the upper posterior hypothalamus, which contains the paraventricular nuclei. In both of these hypothalamic areas, which are key centers for appetite regulation, the magnitude of the inhibitory response following glucose ingestion was reduced in obese, insulin-resistant, normal glucose-tolerant subjects, and there was a delay in the time taken to reach the maximum inhibitory response, even though the plasma insulin response was markedly increased in the obese group. Nonetheless, these results suggest that the brain, like other organs (liver, muscle, and fat) in the body, are resistant to insulin. Westermark P, Wilander E: the influence of amyloid deposits on the islet volume in maturity onset diabetes mellitus. Vaxillaire M, Froguel P: Monogenic diabetes in the young, pharmacogenetics and relevance to multifactorial forms of type 2 diabetes. Role of alterations in systemic, hepatic, and muscle lactate and alanine metabolism. Evidence for reduced insulin-dependent muscle glucose transport or phosphorylation activity in non-insulin-dependent diabetes mellitus. Insulin action and binding in isolated hepatocytes, insulin receptor structure, and kinase activity. A lesson in metabolic regulation inspired by the glucokinase glucose sensor paradigm. Identification of a protein kinase cascade of major importance in insulin signal transduction. Philosophical Transactions of the Royal Society London Series B: Biological Sciences 1999;354:485Â495. Kelley D, Mokan M, Mandarino L: Intracellular defects in glucose metabolism in obese patients with noninsulin-dependent diabetes mellitus. Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Pathogenesis of type 2 diabetes mellitus 399 338 Bajaj M, Suraamornkul S, Romanelli A, et al. The risk variants are common in the population, have only a small effect on disease risk and together only explain a fraction of the heritability of the disease. The diabetic spectrum Diabetes is a group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both. The chronic hyperglycemia of diabetes is associated with long-term damage, dysfunction, and failure of different organs, especially the eyes, kidneys, nerves, heart, and blood vessels. These disease types could be divided further into subtypes possibly representing different disease mechanisms. The diabetes epidemic Worldwide prevalence figures estimate that there were 371 million diabetic patients in 2012 and more than 500 million are expected in 2030. In a situation of affluence most people tend to overconsume International Textbook of Diabetes Mellitus, Fourth Edition. One possible reason for this is that genetic selection has favored energy-preserving genotypes (so called thrifty genotypes); individuals living in an environment with unstable food supply could maximize their probability of survival by efficiently storing energy in times of surplus [2].
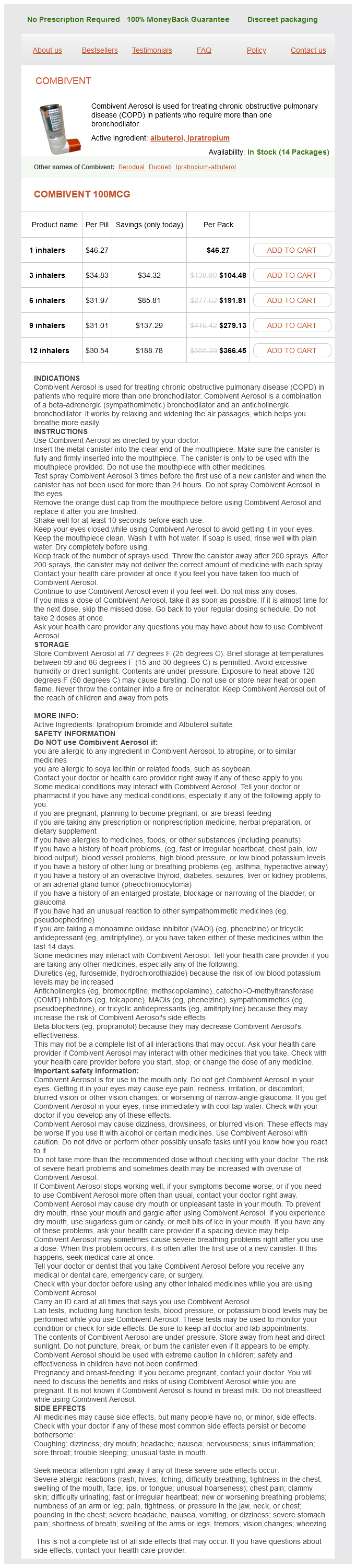
Combivent Dosage and Price
Combivent 100mcg
- 1 inhalers - $46.27
- 3 inhalers - $104.48
- 6 inhalers - $191.81
- 9 inhalers - $279.13
- 12 inhalers - $366.45
The factors and conditions associated with inhibition of glucagon release are listed in Table 10 symptoms 0f pregnancy cheap 100 mcg combivent with mastercard. It has been suggested that glucokinase may serve as a metabolic glucose sensor in pancreatic cells, and hence constitute a mechanism for direct regulation of glucagon release by extracellular glucose. Intra-islet insulin, glucagon, and somatostatin release have been shown to be interrelated [52]. Using isolated perifused human islets, it has been shown that glucose generates coincident insulin and somatostatin pulses and clear antisynchronous glucagon pulses [55]. The fact that these pulses occur in isolated islets demonstrates that their origin is the islets themselves and independent of external metabolic, hormonal, or neuronal signals. The nature of the intra-islet signal(s) coordinating the secretion of the various endocrine cells of the islets of Langerhans is still the subject of intense investigation [56Â61]. Some aspects of glucagon physiology and pathophysiology Glucagon as a counterregulatory hormone Numerous studies have shown that the liver is the main site at which moment-to-moment control of glucose homeostasis takes place and that in normal humans glucagon is the major glucose counterregulatory hormone. By antagonizing the suppressive effects of insulin on glucose production and by stimulating glucose production when appropriate, glucagon not only defends the organism against hypoglycemia, but also restores normoglycemia if hypoglycemia occurs. Biosynthesis, secretion, and action of glucagon 141 release in some diabetic patients markedly increases the risk of severe hypoglycemia in these subjects. Other hormones, such as epinephrine (acutely) and growth hormone and cortisol (more slowly), participate in the counterregulation of the effects of insulin, but careful clinical observations suggest that indeed glucagon is the first line of defense against hypoglycemia [62]. Glucagon in exercise Glucagon levels increase progressively during prolonged exercise [63], during which blood glucose remains relatively constant thanks to a fine balance between muscle glucose uptake and liver glucose production. Although a rise in plasma glucagon does not appear to be essential for increased glucose production during exercise, the presence of glucagon does appear to be necessary. It occurs mainly as a result of the -adrenergic stimulation associated with stress and undoubtedly contributes to the hyperglycemia, which is a classical finding in this condition. Glucagon in starvation Starvation is accompanied by a decline in circulating insulin and a moderate rise in plasma glucagon [65]. The main effects of glucagon during starvation are at the liver, where it contributes to the maintenance of continuous liver glucose output (initially by stimulating glycogenolysis, and later by promoting gluconeogenesis) and the induction of ketogenesis. Whether glucagon contributes to the stimulation of adipose tissue lipolysis during starvation is still disputed. Glucagon and adaptation to extrauterine life A significant rise in plasma glucagon occurs soon after birth in all species investigated so far, which suggests that glucagon has a crucial role in neonatal glucose homeostasis [66]. Furthermore, an important role of glucagon in thermogenic regulation has been suggested. Glucagon and diabetes Plasma levels of glucagon have been found to be increased in all experimental and clinical forms of diabetes mellitus. This disturbance undoubtedly contributes to the hyperglycemia of the disease and excessive ketogenesis of diabetic coma. Numerous studies have shown that failure of glucagon suppression contributes to postprandial hyperglycemia in type 1 [67] and type 2 [68,69] diabetes. Impaired glucagon suppression contributes with impaired insulin release to the excessive blood glucose levels in early type 1 diabetes [70], in subjects with impaired glucose tolerance [71,72], and in patients with ketosis-prone atypical diabetes [73,74]. Morphologic studies have established that the main abnormality in the islet cell population of diabetes is a decrease in the cells with a relative expansion of the -cell mass [75]. The proposal of Unger and Orci to consider diabetes as a "paracrinopathy" of the islets of Langerhans [3] is based on the concept that the very high concentrations of insulin normally reached inside the stimulated islet exerts, directly or by proxy, a major inhibitory effect on glucagon secretion from the neighburing cells. Conversely, a reduction in intra-islet insulin concentrations would permit glucagon release from the cells. Disruption of this mechanism is proposed as a key factor in the pathophysiology of diabetes [76]. This concept is supported by recent data on the micro-anatomy of the islets of Langerhans [74,77]. In type 1 diabetes, cells lack constant action of high insulin levels from juxtaposed cells. Replacement with exogenous insulin subcutaneously injected does not approach the paracrine levels of insulin, except with high doses that "overinsulinize" the peripheral insulin targets, thereby promoting glycemic volatility [3]. In type 2 diabetes, the -cell dysfunction may result from the failure of the juxtaposed cells to secrete the first phase of insulin or from the loss of the intra-islet pulsatile secretion of insulin. Observations made in experimental diabetes in minipigs [78] and recently confirmed in human type 2 diabetes [79] are in support of the second mechanism. Inhibition of glucagon secretion markedly improves experimental diabetes in rodents [80] and knockout of the glucagon receptor makes rodent models of insulin-dependent type 1 diabetes thrive without insulin [29]. The critical role of glucagon action in the liver in diabetes has been demonstrated by expressing glucagon receptors in livers of glucagon receptor-null (GcgR-/-) mice before and after cell destruction by high doses of streptozotocin [81]. Wild-type mice developed fatal diabetic ketoacidosis after streptozotocin, whereas GcgR-/- mice remained clinically normal without hyperglycemia, impaired glucose tolerance, or hepatic glycogen depletion. In this experimental setting, the metabolic manifestations of diabetes cannot occur without glucagon action, and once present, disappear promptly when glucagon action is abolished. These observations strongly suggest that targeting the cell and glucagon are innovative approaches in diabetes management. On the other hand, numerous glucagon antagonists, either peptidic or nonpeptidic, have been indentified and some have entered clinical trials. However, marked inhibition of glucagon signaling may result in -cell hyperplasia, increased mass of the pancreas, increased susceptibility to hepatosteatosis and hepatocellular injury, and an increased risk of hypoglycemia [82]. Further studies in normal and diabetic subjects should identify the 142 Chapter 10 extent to which reduction of glucagon signaling produces a compelling therapeutic benefit without incurring a risk of adverse events. The glucagonoma syndrome the glucagonoma syndrome is a rare disorder associating necrolytic migratory erythema, cheilosis, usually mild diabetes mellitus, anemia, weight loss, venous thrombosis, and, frequently, neuropsychiatric symptoms [83]. Proceedings of the Society for Experimental Biology and Medicine 1959;102: 621Â623.