General Information about Cefpodoxime
Vantin is often used to deal with infections within the respiratory tract, corresponding to bronchitis and pneumonia. It may also be prescribed for infections of the skin, urinary tract, and ear. The medicine is taken orally in the form of tablets or suspension, making it handy for these who don't choose injections.
Cefpodoxime works by inhibiting the expansion of micro organism, preventing them from producing cell partitions and finally leading to their destruction. This makes it an efficient treatment for numerous bacterial infections.
Another benefit of Vantin is its favorable security profile. While like all medication, it might cause delicate unwanted aspect effects corresponding to nausea, diarrhea, and headache, it is generally well-tolerated by most sufferers. However, as with any medicine, it may be very important observe the prescribed dosage and course of remedy to prevent any potential opposed results.
Cefpodoxime, commonly marketed as Vantin, is an antibiotic medicine used to treat quite lots of bacterial infections. It is assessed as a third generation cephalosporin, which implies it is more superior than earlier generations and can combat a wider vary of micro organism.
Before taking Vantin, sufferers should inform their healthcare supplier of any existing medical circumstances or allergic reactions. It can be important to reveal any other drugs or supplements being taken to make sure there are not any potential drug interactions.
It can be important to complete the full course of remedy, even when signs improve, to ensure the an infection is fully eradicated. Stopping the medicine prematurely can result in the return of the an infection or its persistence.
Vantin can be thought of protected to use in kids, making it an acceptable option for pediatric sufferers with bacterial infections. However, it should not be used in infants less than two months of age.
One of the main benefits of Vantin is its capacity to fight both gram-positive and gram-negative micro organism. This is necessary because some bacteria have turn into proof against earlier generations of antibiotics, making them ineffective. Cefpodoxime has been shown to be effective towards many of these antibiotic-resistant bacteria, making it a valuable treatment choice for healthcare providers.
In conclusion, Vantin, or cefpodoxime, is a extremely efficient antibiotic used to treat a variety of bacterial infections. Its broad spectrum of activity, favorable safety profile, and suitability to be used in kids make it a priceless therapy choice. However, its use ought to always be beneath the guidance of a healthcare provider and following the prescribed dosage and duration of therapy is essential for its effectiveness.
As with any antibiotic, it is important to use Vantin solely when prescribed by a health care provider. Misuse or overuse of antibiotics can contribute to the event of antibiotic-resistant micro organism, which can pose a risk to public well being.
The individual mutations at position 48 or 90 infection yellow pus purchase cheap cefpodoxime on-line, and mutations at both of these sites, results in successively less processing of Gag and GagPol polyproteins in vitro. The mutation at position 48 occurs at the hinge of the beta ribbon strands near the active site of the protease, potentially sterically hindering entry of the inhibitor to the active site (Eberle et al. Mutations conferring resistance have been shown to arise in 45% of patients treated with saquinavir (1800 mg/day) alone or in combination with zidovudine for 812 months. The most common mutation observed was LeuMet at codon 90 (L90M), with mutations at codon 48 rarely observed (Jacobsen et al. For example, L90M does not reduce the susceptibility of subtype G to saquinavir (Santos et al. Mutations that are selected for by saquinavir provide crossresistance to many of the first-generation protease inhibitors (Winters et al. Cross-resistance between saquinavir and nelfinavir has also been observed (Jacobsen et al. A point mutation Leu90Met/Ile (as well as mutations at positions 36, 71, and 84) was observed, without detection of the Gly48Val mutation (Ives et al. The use of ritonavir-boosted saquinavir results in very low rates of protease inhibitor resistance in treatment-naive patients. Saquinavir boosted with low-dose ritonavir compares favorably with other boosted protease inhibitors (de Mendoza et al. Predictors of a response to ritonavirboosted saquinavir and lopinavir in a double-protease regimen include the absence of mutations at codons 82 and 154 of the protease gene (von Hentig et al. Calculation of a virtual inhibitory quotient using data on resistance mutations can assist in predicting which patients will respond to ritonavir-boosted saquinavir (Mallolas et al. Lamivudine, saquinavir, and these two drugs in combination with zidovudine have demonstrable additive or synergistic interactions. Additive to synergistic activity has been demonstrated for the combination of interferon-alpha and saquinavir (Johnson et al. The combination of lopinavir and saquinavir has been shown to be synergistic at a variety of ratios tested without cellular toxicity. Increased intracellular concentrations of saquinavir due to lopinavir inhibition of P-glycoprotein is a possible mechanism (Molla et al. Synergy has also been demonstrated between atazanavir and saquinavir using virus strains with varying degrees of resistance (Dam et al. This might explain the inhibitory effects of protease inhibitors on lymphocyte apoptosis (Rizza and Badley, 2008). Adults Saquinavir mesylate must be combined with low-dose ritonavir to achieve boosting of serum levels. The recommended dose is 1000 mg saquinavir film-coated tablets plus 100 mg ritonavir, each administered twice daily with food. Other dosage regimens boosted with ritonavir have also been evaluated (Roche, product information), and two large (but not comparative) studies suggested that once-daily ritonavirboosted saquinavir (100 mg and 15002000 mg, respectively) was safe, well tolerated, and resulted in sustained saquinavir exposure while reducing ritonavir exposure (Bickel et al. Newborn infants and children the film-coated tablets of saquinavir offer a reduction in pill burden and have similar tolerability compared with hard gel capsules (Bittner et al. The active site is formed at the dimer interface, with one aspartyl residue from each subunit contributing to 4c. The manufacturer recommends that saquinavir should not be given to breastfeeding women. For patients receiving the 600 mg three times daily dose, steady-state plasma concentrations were five times the target concentration in 11 of 12 patients, remaining above this value for the entire dosing interval in 10/12 patients. For those patients receiving 200 mg three times daily, saquinavir was detectable in plasma for the duration of the dose interval in the majority of patients but not in those receiving 25 mg three times daily (Kitchen et al. The drug has nonlinear pharmacokinetics when given in doses of 75, 200, and 600 mg administered three times daily (Noble and Faulds, 1996). There was evidence of drug accumulation (two- to threefold) over a period of 4 weeks (Kitchen et al. The hard gel capsule and film-coated tablet formulations have been demonstrated to be bioequivalent in healthy volunteers (Bittner et al. A significant reduction in interpatient variability was observed with the film-coated tablets when compared with hard gel capsule, when administered twice daily with ritonavir and nucleoside reverse transcriptase inhibitors. Slight reductions in saquinavir plasma exposure were noted when saquinavir was administered with other antiretroviral drugs-20% when given twice daily with ritonavir and nucleoside reverse transcriptase inhibitors and 12% for a once-daily regimen with ritonavir and atazanavir. This may be partially explained by the small reduction in dosage size of 1600 mg for hard gel capsule versus 1500 mg for film-coated tablets (Winston et al. The mean oral bioavailability of a 600-mg dose of saquinavir when taken following food is very low, in the range of 4% (18-fold greater than in the fasted state) (Noble and Faulds, 1996). This is partly because only 30% is absorbed and also due to considerable first-pass metabolism of the drug (Williams et al. A rat model has suggested that the low oral bioavailability of saquinavir is due to intestinal rather than hepatic first-pass metabolism (Lledo-Garcia et al. The absorption of saquinavir is rapid when it is administered after fasting (time to maximum concentration [tmax] 2. Clinically significant pharmacokinetic and pharmacodynamics data regarding saquinavir. Pharmacokinetics and pharmacodynamics 4023 absorption is also markedly increased when taken after food. Nonlinear pharmacokinetics was apparent for both single and multiple doses of saquinavir, possibly because of saturable first-pass metabolism (Muirhead et al. The increased absorption of saquinavir following food is possibly due to the increased ratio of nonionized drug to ionized drug as a result of the increase in gastric pH (Barry et al. There was a 53% lower clearance (Cl/F) in females after adjusting for weight (Fletcher et al. Ritonavir peak and trough levels were significantly lower during gestation than during the postpartum period.
Severe hepatotoxicity without hypersensitivity may occur after the first 12 weeks of therapy (68% in one series) (Clarke et al antibiotic effect on birth control cheap 100 mg cefpodoxime. Others have shown no increased risk of clinically significant liver disease in patients treated with long-term nevirapine (at least 3 years) (Van Welzen et al. This is in contrast to a smaller Spanish study that reported an independent association of nevirapine with fibrosis progression (Macias et al. Risk factors for nevirapine hepatotoxicity include hepatitis B and/or C coinfection (Ena et al. There have been several deaths from fulminant hepatitis and liver failure secondary to nevirapine (Cattelan et al. Nevirapine-based therapy has also been associated with faster progression of liver fibrosis in patients with chronic hepatitis C (Macias et al. The risk of rashassociated hepatotoxicity is threefold higher in women than in men, and the risk ratio of these reactions is 9. Several studies have shown no association between hepatotoxicity and nevirapine concentrations (Dong et al. In a resource-limited setting (South Africa), hepatotoxicity from nevirapine was not a serious problem (Chu et al. The beneficial changes in lipid profile have been shown to be significantly greater than with efavirenz (van Leth et al. Atazanavir ritonavir treatment was associated with a greater increase in triglyceride levels (35. The prevalence of dyslipidemia after 3 years of treatment was 73% in one cohort (Liu et al. Replacement of the protease inhibitor component of the antiretroviral regimen in patients with lipodystrophy syndrome and/or dyslipidemia and virologic suppression resulted in marked improvements in the atherogenic lipid profiles of patients randomized to nevirapine. This strategy has also been shown to improve the body shape changes associated with lipodystrophy by causing reductions in abdominal visceral fat (Carr et al. However, the addition of lipid-lowering therapy was more effective in lowering elevated cholesterol and triglyceride levels in patients on a protease inhibitor regimen than a 3878 Nevirapine switch to nevirapine (4045% reduction compared with 2528%) (Calza et al. There is no significant association between the recent or cumulative use of nevirapine and development of myocardial infarction (Worm et al. Neuropsychiatry side effects Central nervous system complications of nevirapine therapy occur less frequently than with efavirenz and include headache and somnolence. Vivid dreams (similar to those described as an adverse effect of efavirenz) have been uncommonly described in patients after initiating nevirapine (Morlese et al. Other reported neuropsychiatric effects include clouding of consciousness and cognitive impairment, visual hallucinations, persecutory delusions, attempted suicide, and depression (Foster et al. A switch from efavirenz to nevirapine is associated with a reduction in neuropsychiatric side effects with complete resolution of depression, anxiety, and fatigue, with or without sleep disturbances, in 75% of patients (Ward and Curtin, 2006). Other adverse effects A case of acute renal failure has been reported as occurring secondary to nevirapine therapy. The patient presented with a hypersensitivity reaction of fever, rash, and eosinophilia but also developed acute renal failure, which was attributed to interstitial nephritis, and all symptoms resolved on discontinuation of nevirapine (Franceschini et al. A single case of diffuse interstitial pulmonary infiltrates has been reported 23 weeks after commencing nevirapine. In the first 2 weeks of nevirapine therapy, the patient had a mild fever and dry cough, which progressed with development of rash and dyspnea soon after dose escalation of nevirapine to 400 mg daily. Complete resolution of symptoms and chest radiograph abnormalities occurred with cessation of nevirapine (Sankatsing and Schouten, 2007). A case of severe ocular complication associated with Stevens-Johnson syndrome/ toxic epidermolysis syndrome in a 25-year-old man who commenced stavudine, lamivudine, and nevirapine 2 weeks before the rash developing. He complained of visual loss, and 6 weeks after onset of Stevens-Johnson syndrome, he had a rapidly progressive conjunctivalization of the cornea, resulting in blindness (Schulze Schwering et al. The incidence of rash in one study of 235 pregnant women of predominantly black African and black Caribbean origin was 7. Asymptomatic serum liver function test abnormalities were seen in 1020% of pregnant women in Italy (Manfredi and Calza, 2007). A Thai study suggested that pregnant women had a significantly higher rate of hepatotoxicity than nonpregnant women (Phanuphak et al. No case occurred in the 30% of women who started on antiretroviral treatment in the first trimester or in the 44% who began treatment in the second trimester. All cases occurred in the third trimester (3 of 5 women), but numbers are small (Joy et al. There are reports of pregnant women who died from fulminant hepatitis secondary to nevirapine (Lyons et al. It is quite safe to continue treatment in women who are stable on nevirapine therapy before becoming pregnant (Thorne and Newell, 2005). Fetal toxicity There was no evidence of teratogenicity in studies performed in rats and rabbits treated with doses of 50 mg/kg/day and 300 mg/kg/day nevirapine. No effects on fetal development were seen in rats with systemic exposures equivalent to the recommended human dose or rabbits with systemic exposure about 50% higher than the recommended human dose. No reports of adverse effects on the fetus have been observed from several studies (Bae et al. Risks in pregnancy Nevirapine appears to be reasonably well tolerated in pregnancy, with a generally low rate of adverse events, particularly 7. Clinical uses of the drug 3879 studies in animals failed to demonstrate a risk to the fetus; adequate well-controlled studies involving pregnant women have not been conducted). Clinical trials demonstrating efficacy of nevirapine, in combination with other antiretroviral drugs, are outlined in this section and summarized in Table 235. There is no difference in virologic or immunologic responses in antiretroviralnaive patients starting on therapy with nevirapine 400 mg once daily or 200 mg twice daily (van Leth et al. For this reason, it is recommended that nevirapine be used in a twicedaily dosing regimen in patients who are antiretroviral naive.
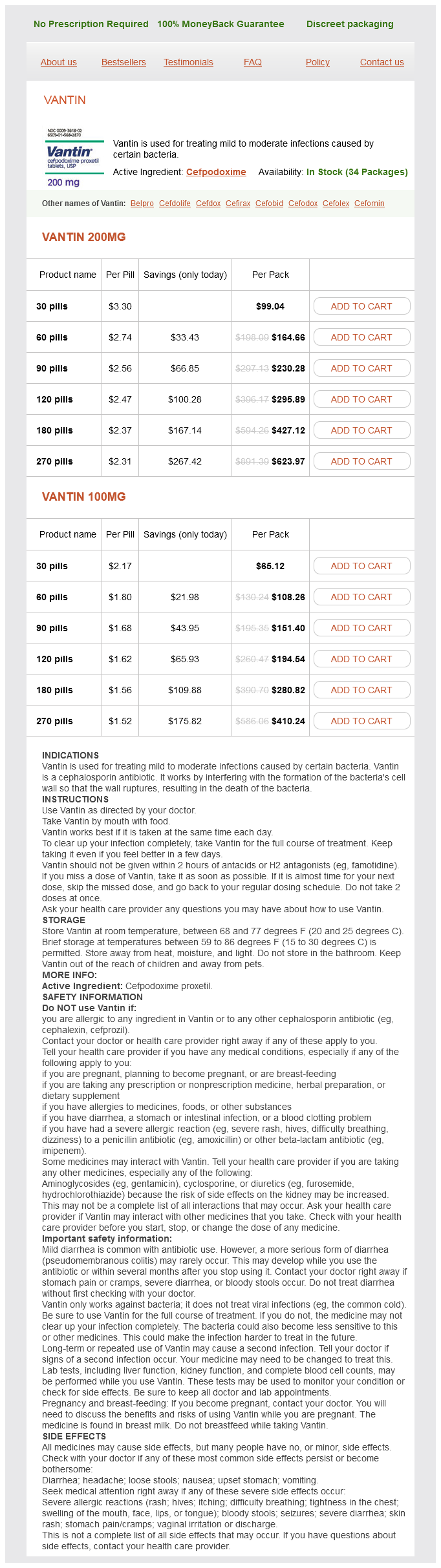
Cefpodoxime Dosage and Price
Vantin 200mg
- 30 pills - $99.04
- 60 pills - $164.66
- 90 pills - $230.28
- 120 pills - $295.89
- 180 pills - $427.12
- 270 pills - $623.97
Vantin 100mg
- 30 pills - $65.12
- 60 pills - $108.26
- 90 pills - $151.40
- 120 pills - $194.54
- 180 pills - $280.82
- 270 pills - $410.24
Bioequivalence of a dolutegravir antibiotics you can give dogs cheap cefpodoxime 100 mg visa, abacavir, and lamivudine fixed-dose combination tablet and the effect of food. Population pharmacokinetics and pharmacodynamic modeling of abacavir (1592U89) from a dose-ranging, double-blind, randomized monotherapy trial with human immunodeficiency virus-infected subjects. Molecular mechanisms of resistance to human immunodeficiency virus type 1 with reverse transcriptase mutations K65R and K65R + M184V and their effects on enzyme function and viral replication capacity. Changes in proteinuria and albuminuria with initiation of antiretroviral therapy: data from a randomized trial comparing tenofovir disoproxil fumarate/emtricitabine versus abacavir/lamivudine. Pharmacokinetics and bioavailability of carbovir, a carbocyclic nucleoside active against human immunodeficiency virus, in rats. Abacavir/lamivudine/zidovudine as a combined formulation tablet: bioequivalence compared with each component administered concurrently and the effect of food on absorption. The chemical name of emtricitabine is (2R,5S)-5-fluoro-1-[2-(hydroxymethyl)-1,3-oxathialon-5-yl]cytosine. The chemical structure of emtricitabine differs from that of lamivudine in that it has a fluorine atom in the 5 position of the pyrimidine ring, as opposed to lamivudine, which has a hydrogen atom. Emtricitabine differs from other cytidine analogs because of the fluorine in the 5 position (Seshachalam et al. Emtricitabine is available as capsule for oral administration containing 200 mg of drug and as an oral solution at a concentration of 10 mg/ml. In vitro resistance testing indicates that isolates resistant to lamivudine are virtually always resistant to emtricitabine and vice versa, due to the structural similarities of the two compounds (Frampton and Perry, 2005). However, despite the similar mutations mediating resistance to lamivudine and emtricitabine, these mutations emerge at a slower rate and less frequently, and patients are, on average, half as likely to develop resistance when treated with emtricitabine compared with lamivudine-based combinations (Maserati et al. This compares to a rate of 9% of resistance to entecavir at 2 years (Coffin and Lee, 2009), and 18% resistance to lamivudine at 1 year (Marcellin et al. Although emtricitabine is not approved for the treatment of hepatitis B infection in most countries, clinicians who are using it for this purpose typically prescribe a dose of 200 mg daily. In vitro synergy and antagonism Emtricitabine had synergistic activity in vitro with stavudine, tenofovir, efavirenz, rilpivirine, zidovudine, the integrase inhibitors elvitegravir and raltegravir, and the protease inhibitors darunavir and atazanavir, along with additive in vitro activity in combination with zalcitabine and didanosine (Bridges et al. For patients aged 3 months to 17 years, the recommended therapeutic dose of emtricitabine solution is 6 mg/kg up to a maximum of 240 mg (24 ml) given once daily. For children weighing more than 33 kg who can swallow an intact capsule, a 200 mg capsule should be given once daily. Emtricitabine is not approved for treatment of hepatitis B infection in children, and because there are few if any reports of it being used, dosing recommendations are not provided here. Pregnant and lactating mothers Emtricitabine levels decrease in the third trimester of pregnancy. In general these plasma levels do not fall below the threshold thought necessary for clinical efficacy and so no dose adjustment is recommended. Emtricitabine is secreted in human breast milk at a concentrations equivalent to 2% of the recommended daily dose for neonates who are solely breastfed. Dose and dosing interval adjustment in adult patients with renal impairment receiving emtricitabine. Appropriate dose for a given creatinine clearance Formulation Capsule (200 mg) Oral solution (10 mg/ml) 50 ml/minute 200 mg every 24 hours 240 mg every 24 hours (24 ml) 3049 ml/minute 200 mg every 48 hours 120 mg every 24 hours (12 ml) 1529 ml/minute 200 mg every 72 hours 80 mg every 24 hours (8 ml) < 15 ml/minute or on hemodialysisa 200 mg every 96 hours 60 mg every 24 hours (6 ml) a Assumes a 3-hour hemodialysis session three times per week; If dosing on day of hemodialysis, give dose after dialysis. Dosing recommendation for patients with impaired renal function are summarized in Table 231. Emtricitabine, like many other nucleoside analogs, may in rare cases cause hepatic injury, so liver function tests should be monitored during therapy. However, like other nucleoside analogs, the intracellular half-life is significantly longer than the plasma t½, on average 39 hours, which is also longer than the intracellular t½ of lamivudine triphosphate, 10. Consequently, emtricitabine is eminently suitable for once-daily dosing because the half-life of antiviral activity of nucleoside analogs in vivo is primarily a function of their intracellular halflife (Piliero, 2004). As with other nucleoside analog drugs, the binding of emtricitabine to human plasma proteins in vitro is low (< 4%) and independent of concentration over the range of 0. At peak plasma concentrations, the mean plasmablood drug concentration ratio was ~ 1. Drug distribution Time to peak plasma concentrations of emtricitabine (tmax) occurs 12 hours after an oral dose, indicating rapid absorption. These investigators found that the mean plasma concentrationtime profiles at each dose level were similar across all age groups studied. The plasma emtricitabine concentrations for patients given the oral solution were measured from 30 minutes post dose, and reached a Cmax of 0. The authors stated that the capsule formation showed marginally higher plasma exposure compared with the oral solution. The pharmacokinetics of emtricitabine have not been fully evaluated in the elderly, but its use has been shown to be generally safe and effective in this population (Blanco et al. Pharmacokinetics and pharmacodynamics 3805 Emtricitabine is widely distributed throughout the body to both intracellular and extracellular fluid spaces and unlike tenofovir is present in high concentrations in saliva (mean ratio of saliva/plasma concentrations ~ 86. Emtricitabine is also detected in high concentrations in rectal (rectal tissue/plasma concentration ratio 4. The central nervous system penetration of emtricitabine has been incompletely studied. In 30 patients receiving emtricitabine, tenofovir and a ritonavir boosted protease inhibitor, the mean emtricitabine cerebrospinal fluid/plasma concentration ratio was 0.