General Information about Cardura
It is necessary to tell your doctor about some other drugs you take earlier than beginning Cardura. It may interact with different drugs and trigger potentially harmful side effects. It must also be used with caution in sufferers with liver or kidney disease, in addition to in these with low blood pressure.
Cardura comes within the form of oral tablets and is usually taken once a day with or without food. The dose may be adjusted by a healthcare provider based on the person's response to the treatment. It is necessary to take Cardura at the identical time every day to take care of a steady stage of the drug within the body. It might take a quantity of weeks for the treatment to indicate its full effects, so it's important to not stop taking it without consulting a doctor.
BPH, on the opposite hand, is a non-cancerous enlargement of the prostate gland that may trigger troublesome urinary signs in males. As men age, the prostate naturally grows in measurement, which may trigger pressure on the bladder and urethra, leading to problem in urination and other symptoms corresponding to frequent urination, weak urine stream, and the sensation of incomplete bladder emptying. BPH primarily affects males over the age of fifty and might significantly affect their high quality of life. Cardura works by relaxing the muscle tissue within the prostate and the bladder, making it simpler for males to urinate.
The major operate of Cardura is to relax and widen the blood vessels, which in flip lowers blood strain and allows blood to flow extra easily by way of the body. This lowers the chance of coronary heart assaults, strokes, and other cardiovascular problems. In addition, Cardura also works to improve urinary signs in men with BPH by enjoyable the muscle tissue within the prostate and bladder, making it simpler to urinate.
Cardura, also identified by its generic name doxazosin, is a medicine that's commonly used for two major purposes: treating high blood pressure and managing symptoms of benign prostatic hyperplasia (BPH). This powerful drug belongs to a class of medicines known as alpha blockers, and has been proven to be an efficient treatment choice for patients affected by these circumstances.
Like any medicine, Cardura could trigger some unwanted effects, although not everyone experiences them. Common unwanted effects embrace dizziness, lightheadedness, nausea, and headaches. These usually subside because the body adjusts to the treatment. In some circumstances, severe unwanted effects such as fainting, problem respiration, and chest pain might happen, and quick medical consideration should be sought if these occur.
In conclusion, Cardura is a highly effective treatment for managing high blood pressure and urinary signs in males with BPH. It has been used for a few years and has confirmed to be safe and well-tolerated by most patients. However, it could be very important follow the really helpful dosage and to tell your physician of any side effects or interactions with different drugs. With correct use and monitoring, Cardura might help improve the standard of life for those living with hypertension or BPH.
High blood pressure, also referred to as hypertension, is a typical situation that impacts millions of people worldwide. It is sometimes called a silent killer because it normally has no warning signs or signs till serious issues come up. If left uncontrolled, high blood pressure can result in serious well being points similar to heart disease, stroke, and kidney failure. Cardura helps to lower and preserve a wholesome blood pressure level, thereby decreasing the chance of these harmful conditions.
The Pleural Cavity 389 At sea level arrhythmia definition cardura 2 mg purchase amex, the atmospheric pressure exerted by the mixture of all the gases is 760 mm Hg. Each gas exerts a proportionate part of the total atmospheric pressure, depending on its concentration in the mixture of gases. Therefore, the pressure exerted by oxygen is 20 percent of the total pressure exerted by all the gases (0. The part of the total atmospheric pressure exerted by a gas is called the partial pressure of the gas. Gases diffuse between blood, tissues, and pulmonary alveoli because of differences in their partial pressures. This blood is pumped through the pulmonary capillaries, where it comes into contact with the air in the pulmonary alveoli. Therefore, oxygen diffuses from alveolar air into pulmonary capillaries, and carbon dioxide diffuses from pulmonary capillaries into the alveoli. Exchange of gases between alveolar air and pulmonary capillaries is accomplished by diffusion across the alveolar membrane. Efficient gas exchange requires (1) a large capillary surface area in contact with alveolar air, (2) unimpeded diffusion of gases across the alveolar membrane, (3) normal pulmonary blood flow, and (4) normal pulmonary alveoli. The Pleural Cavity the lungs are covered by a thin membrane called the pleura, which also extends over the internal surface of the chest wall. Because the lungs fill the thoracic cavity, the two pleural surfaces are in contact. In disease, however, the pleural surfaces may become roughened because of inflammation and may become adherent. Inflammatory exudate may accumulate in the pleural cavity and separate the two pleural surfaces. Pleura the mesothelial covering of the lung (visceral pleura) and chest wall (parietal pleura). The lungs are held in an expanded position within the pleural cavity because the pressure within the pleural cavity (intrapleural pressure) is less than the pressure of the air within the lungs (intrapulmonary pressure). The lungs become filled with air at atmospheric pressure and expand to fill the enlarged thoracic cavity, stretching the elastic tissue within the lungs. The tendency of the stretched lung to pull away from the chest wall and return to its original contracted state creates a slight vacuum within the pleural cavity. Because the intrapleural pressure is slightly less than atmospheric pressure, it is often called "negative pressure. Pulmonary ventilation is usually tested by measuring the volume of air that can be moved into and out of the lung under standard conditions. Specialized tests can measure the total volume of air in the lungs and the volume of air remaining in the lungs after a maximum expiration. Oxygen concentration is reduced, and arterial oxygen saturation is decreased correspondingly. Arterial blood for analysis is Vital capacity the maximum volume of air that can be forcefully expelled after a maximum inspiration. Pneumothorax 391 usually collected by inserting a small needle into the radial artery in the wrist and withdrawing a small amount of blood. One can also determine how effectively the lungs are oxygenating the blood (arterial oxygen saturation) using a device called a pulse oximeter. A fingertip is inserted into the device, which measures photoelectrically the changes in light absorption of the hemoglobin in the fingertip capillaries at various wavelengths during systole and diastole. Then the data are used to automatically calculate the oxygen saturation of the arterial blood, and the device promptly displays the result. Pneumothorax Because the intrapleural pressure is below that of the atmosphere, air flows into the pleural space if the lung or chest wall is punctured. When this occurs, the negative pressure that holds the lung in the expanded position is lost, and the lung collapses because the elastic tissue within the lung contracts. This condition, which is called a pneumothorax (pneumo = air), may follow any type of lung injury or pulmonary disease that allows air to escape from the lungs into the pleural space. Most cases occur in young healthy people, usually as a result of rupture of a small, air-filled, subpleural bleb at the apex of the lung. The sudden escape of air into the pleural cavity that is associated with any type of pneumothorax usually causes chest pain and often some shortness of breath. The breath sounds, which normally can be heard with a stethoscope when the air moves in and out of the lung during respiration, are diminished on the affected side. The development of a positive (higher than atmospheric) pressure in the pleural cavity, called tension pneumothorax, may accompany any type of pneumothorax. The trachea and mediastinal structures are shifted away from the side of pneumothorax and encroach on the opposite pleural cavity. Depression of diaphragm Atelectasis 393 overdistended with air under pressure, and the affected lung collapses completely. A tension pneumothorax can be fatal if it is not recognized and treated promptly by evacuating the trapped air to relieve the pressure. A pneumothorax is usually treated by inserting a tube into the pleural cavity through an incision in the chest wall. The tube prevents accumulation of air in the pleural cavity and aids reexpansion of the lung.
Many diagnostic procedures are noninvasive (requiring no physical invasion of the body heart attack while pregnant cheap cardura 2 mg line, its openings, or cavities). A common example of such noninvasive diagnostic testing is the use of imaging technology (x-rays or ultrasound, for example). Such procedures may be relatively minor and have little discomfort associated with them. Common examples are drawing blood, obtaining a Pap smear (to collect a sample of cervical cells), or sampling fluid and cells from a surface accessible lesion with a very fine needle (fine needle aspiration). Somewhat more invasive are a variety of endoscopic procedures in which a tube (generally flexible) is passed into a body opening such as the esophagus or anus (as is done in the case of colonoscopy). Laparoscopic procedures involving the introduction of devices into body cavities or obtaining samples of internal organs (liver, kidney, and lungs, for example) by the use of sampling devices guided by imaging technology are yet more invasive, but much safer and potentially less costly than a surgical procedure. Whatever the case, when the clinician has reached a diagnosis, he or she can then offer a prognosis, an opinion concerning the eventual outcome of the disease. The foundation for the process of obtaining a diagnosis is the history and a physical examination. Noninvasive testing Diagnostic procedure requiring no physical invasion of the body. As is the case in any interaction between individuals, this requires the physician to establish a relationship with the patient that facilitates the accurate verbal transmission of information. The patient must feel enabled to present his or her history both fully and accurately. The physician must be able to elicit such information and accurately interpret it without prejudgment or bias (either scientific or social). Acquiring such interviewing skill is an early and essential part of the training of a medical student. To facilitate obtaining and recording an accurate, organized, patient history, a standard approach is generally used on an initial encounter, although it may be modified on subsequent visits. This approach consists of several parts: Chief complaint: this introduction to the history seeks to establish why the patient has sought medical attention. It may be followed up by a brief survey of any additional problems currently being experienced by the patient. This part of the history establishes the "when, where, and how" of the chief complaint, that is, the source of the symptoms experienced. Family history is important in diagnosing many common chronic diseases such as diabetes and heart disease. Questions are asked about potentially addictive behaviors such the use of alcohol, tobacco products, and recreational drugs. The review of systems: this is often considered to be the center of the patientphysician encounter and consists of a body systemoriented, head to toe-review of all presenting symptoms in an organized manner. The review may disclose additional symptoms not initially reported by the patient that are important to the diagnosis. A physician investigating the presenting symptom of back pain may elicit the additional symptom of pain on urination during the review, which suggests potential urinary tract disease. The experienced physician often will undertake this review as part of the physical examination. The practitioner places particular emphasis on the part of the body affected by the illness, such as the ears, throat, chest, and lungs in the case of a potential respiratory infection. For example, respiratory symptoms may be associated with a range of etiologies affecting multiple body systems. Any abnormalities detected on the physical examination are correlated with the clinical history. At this point, the practitioner begins to construct a hypothesis regarding diseases or conditions that best fit with the clinical findings. Often, more than one diagnosis must be considered, and such consideration is likely to be altered by the results of laboratory and other diagnostic tests. For example, respiratory symptoms might, based on patient history, suggest a seasonal allergy. A suggestion of renal problems in the patient could point to a serious, multisystem disease involving blood vessels (a vascular disease). Additional laboratory tests and potentially invasive procedures to sample patient tissue would be needed to support such a diagnosis. In difficult cases, the clinician may also obtain the opinion of a medical consultant (a physician with special training and experience in the type of medical problem presented by the patient). For a respiratory disease, a pathologist experienced in tissuebased diagnosis or a radiologist expert in the analysis of x-ray and other visualization data produced by physical methods might be consulted. The wise physician always maintains a probabilistic approach in constructing the diagnosis. In testing the diagnostic hypothesis, the clinician uses a variety of tests and procedures and considers the usefulness of possible results of the tests in the clinical reasoning process. Radiologist Physician expert in the use and analysis of imaging techniques and results. One major medical center lists more than 1,300 laboratory tests that are available to its staff. Medical procedures carry a degree of risk, ranging from trivial to potentially serious. Diagnostic tests and procedures also vary in the amount of information they provide in relation to a potential diagnosis. For example, colonoscopy provides no information in the case of respiratory symptoms, but it may lead to a definitive diagnosis in the case of possible bleeding from the rectum. Colonoscopy costs thousands of dollars at a major medical center, whereas determination of fecal blood.
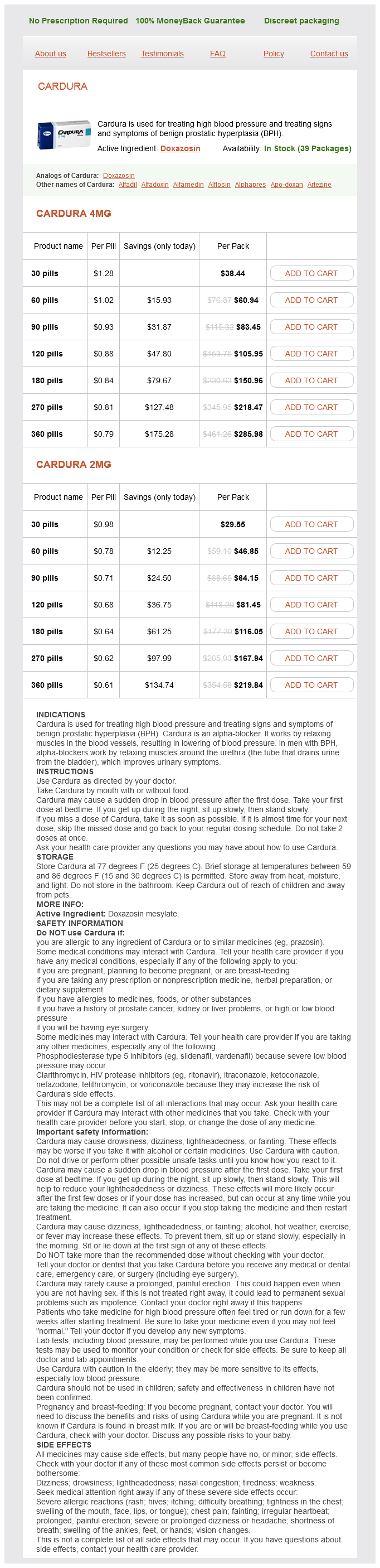
Cardura Dosage and Price
Cardura 4mg
- 30 pills - $38.44
- 60 pills - $60.94
- 90 pills - $83.45
- 120 pills - $105.95
- 180 pills - $150.96
- 270 pills - $218.47
- 360 pills - $285.98
Cardura 2mg
- 30 pills - $29.55
- 60 pills - $46.85
- 90 pills - $64.15
- 120 pills - $81.45
- 180 pills - $116.05
- 270 pills - $167.94
- 360 pills - $219.84
Conversion to sirolimus and mycophenolate can attenuate the progression of bronchiolitis obliterans syndrome and improves renal function after lung transplantation heart attack jeff x ben cardura 2 mg order without prescription. Lung transplantation: the role of azithromycin in the management of patients with bronchiolitis obliterans syndrome. Pulmonary retransplantation: predictors of graft function and survival in 230 patients. Index Notes Tables, figures and boxes are indicated by an italic t, f, or b following the page number. Define the common terms used to describe disease including, but not limited to , lesions, symptomatic and asymptomatic disease, etiology, and pathogenesis. Describe the various types of diagnostic tests and procedures that can help the practitioner make a diagnosis. Disease, in its broadest sense, is any compromise to the normal function of the body and the systems of which it is composed. However, it is best to consider health and illness as two extremes of a continuum. At one extreme is severe, disabling, or life-threatening illness with corresponding effects on our physical and emotional well-being. At the other extreme is ideal, perfectly good health, a state of physical and mental well-being wished for but rarely attained. Between these two extremes are many gradations of health and disease, ranging from mild or short-term illness that limits activities to some extent to moderate good health that falls short of the ideal state. The midpoint in this continuum, one in which one is neither ill nor in ideal good health, is where most of us are likely to fall. Disease is no longer occasional but becomes chronic as we suffer from degenerative conditions, which are part of the inevitable process of aging. Pathologist Person who studies the structural and functional changes in the body caused by disease. Symptoms such as fever, muscle aches, and pain are part of the process of inflammation, an early defensive reaction by the body to insult (discussed in the presentation on inflammation). Pathologists study the etiology (cause) and pathogenesis (progression or "natural history") of disease by evaluating lesions at the level of organs, the tissues that comprise the organs, the cells that form the tissues, and the molecules of which the cells are composed. The pathologist may observe the diseased tissue with the naked eye (gross examination) or with the aid of a microscope (histologic examination). Histologic examination may be supplemented by the use of special methods of identifying normal or abnormal tissue components using biochemical or immunological techniques (see the discussion of immunology). It is increasingly common for pathologists to study the molecules of which the tissue is composed using the techniques of molecular biology. In addition, pathologists working in the area of laboratory medicine study the composition of our body fluids (blood and urine, for example) to look for markers of disease. Classifications of Disease Pathologists interested in etiology classify diseases into several large categories. Although these categories are broad, this helps in understanding how a disease is likely to progress and how it will affect the patient. Although the above scheme is useful, many diseases fit in multiple categories or fit poorly in any. Principles of Diagnosis the first physician to see the patient and to diagnose the disease is the clinician (the generalist physician, or specialist in a particular area of medicine or surgery) who is expert in detecting and evaluating the objective manifestations of disease, the signs or physical findings. However, a disease may cause the affected individual no discomfort or disability (an asymptomatic disease). Because disease is most often asymptomatic in its early stages, it may progress to the point where it causes subjective symptoms, abnormal physical findings, and is more difficult, impossible, or costly to treat. Therefore, early detection of disease, even before it is brought to the attention of the clinician, is of great importance to the public and is a major concern of the specialist in public health who might design screening systems for early diagnosis. In a period of increased concern about the economic aspects of health care, cost must also be considered. Choosing a Diagnostic Test A diagnostic test can be defined in terms of a set of characteristics that help the clinician judge the usefulness of the procedure in diagnosing a specific disease. A perfect test would always be positive in a patient who has the disease in question and always negative in one who does not. Sensitivity refers to the percentage of patients classified as positive by a test who do have the disease. A test with a high sensitivity will miss few people with the disease (have a low rate of false negatives). Specificity refers to the percentage of patients without the disease who are classified as negative by the test. The clinician attempts to choose a test with as high a sensitivity and specificity as possible for the diagnosis in question. Unfortunately, highly sensitive tests tend to have lower specificity (misdiagnosing people as having a disease they do not have; i. However, a false positive result, assuming a patient has a disease he or she does not, may also lead to anxiety, discomfort, and unneeded therapy. For example, a patient in a clinic who is suspected of having a disease (based on prior clinical information) is much less likely to yield a false negative result than an individual chosen at random off the street. A physician who is considering an invasive, painful, or costly mode of therapy might choose to use a test with high specificity to exclude a false positive result. However, the case is different when choosing screening assays to be applied to a population in which the diagnostic target is a relatively uncommon but potentially serious (possibly fatal) illness where early diagnosis might effect a cure.