General Information about Bupron SR
Bupron SR is a member of the aminoketone class of antidepressants. Unlike different antidepressants that primarily work on the neurotransmitters serotonin and norepinephrine, it acts on the mind chemical dopamine. Dopamine is thought to play a major function in regulating mood and motivation, making Bupron SR a useful tool in treating depression.
Bupron SR is not suitable for everyone and should not be utilized by individuals with a history of an consuming dysfunction or seizures, or those that have taken a monoamine oxidase inhibitor (MAOI) inside the past 14 days. It is important to tell your physician about any medical situations and drugs you're taking before beginning Bupron SR.
Another main advantage of Bupron SR is its effectiveness in aiding smoking cessation. Smoking is a well-known threat factor for several health conditions, together with coronary heart disease and lung cancer. However, quitting smoking is a challenging task, and many people struggle to do so on their own. Bupron SR works by reducing the urge to smoke and minimizing withdrawal symptoms, making it easier for people to give up smoking and enhance their total health.
The dual action of Bupron SR makes it a robust therapy possibility for these suffering from both despair and nicotine addiction. By concentrating on both conditions, it not only improves mood but additionally promotes better overall health and high quality of life.
Bupron SR, additionally known by its generic name bupropion, is a prescription medicine used to deal with depression and assist in smoking cessation. Its unique mechanism of action sets it apart from other antidepressants, making it a preferred alternative among physicians and sufferers alike.
The beneficial dosage for Bupron SR varies relying on the condition being treated. For depression, the same old starting dose is a hundred and fifty mg once every day, and it might be increased to a most of 300 mg per day. For smoking cessation, the beneficial dose is a hundred and fifty mg as soon as every day for three days, followed by 150 mg twice day by day for seven to 12 weeks. It is necessary to comply with your doctor's instructions and never exceed the recommended dose.
In conclusion, Bupron SR is a valuable medicine for the therapy of melancholy and smoking cessation. Its distinctive mechanism of action and twin advantages make it an attractive option for people struggling with each situations. If you or a beloved one is experiencing symptoms of despair or struggling to stop smoking, speak to a healthcare skilled to see if Bupron SR may be an acceptable therapy option.
Like any treatment, Bupron SR does have some potential side effects, including dry mouth, headache, nausea, and insomnia. However, these unwanted facet effects are often mild and tend to improve with continued use. In rare instances, Bupron SR may also cause seizures, so you will want to talk about any historical past of seizures along with your doctor earlier than taking this medication.
Depression is a standard mental well being disorder that impacts tens of millions of individuals worldwide. It is characterised by persistent feelings of unhappiness, loss of interest in activities, and modifications in appetite and sleep patterns. While there are numerous therapy choices available, many patients battle to find reduction from their signs. This is the place Bupron SR comes in.
Anticholinergic effects of some of these medications anxiety triggers order on line bupron sr, as well as anticholinergic medications used to remedy extrapyramidal side effects, may further contribute to cognitive problems in schizophrenia. The advent of newer second-generation antipsychotic medications, beginning with clozapine in the 1990s, further improved treatment of schizophrenia, and for the first time targeted negative symptoms as well as being equally effective for positive symptoms. Unwelcome side effects may occur with these agents, such as sedation, hypotension, seizures, weight gain, and hyperglycemia and other features of metabolic syndrome (85). Therefore, regular monitoring of vital signs and laboratory metabolic indicators is indicated. Patients vary considerably in their metabolism of antipsychotic medications; therefore, individualization of dosage is indicated. Because there are no biomarkers or pharmacological tests to guide the choice of antipsychotic agent, the selection of medication is typically based on the side-effect profile (85). Most antipsychotic effects occur within the first week, with marginal improvements thereafter (85). After 4 to 6 weeks without adequate treatment response, it is recommended to switch to another antipsychotic agent with a different receptor-binding profile. Treatment is generally continued for at least 1 year for first episodes and at least 5 years for patients with multiple episodes of illness (85). Clozapine is particularly effective for refractory illness and for suicidal ideation, with a 50%60% response in patients who are refractive to all other antipsychotics (85). A specific safety concern for treatment with clozapine is agranulocytosis, which is uncommon (<1% of patients treated and increases with dosage level) but can be medically catastrophic, and even fatal in 1 of 10,000 treated patients. Optimally safe prescription of this antipsychotic drug therefore requires close monitoring of white blood cell counts (85) in addition to the standard laboratory monitoring of metabolic status recommended for other antipsychotic agents. Antipsychotic polypharmacy, defined as the use of two or more antipsychotic agents simultaneously, is generally discouraged. There is no evidence, outside of specific justifications for this practice in unusual circumstances, to suggest that more than one antipsychotic agent is more effective than a single antipsychotic, yet this practice often occurs. Antipsychotic polypharmacy is also further associated with potential for excessive dosing, adverse drugdrug interactions, and dosing complexity that further compromises patient adherence to medication schedules (85). High-dose antipsychotic treatment above standard recommended dosing levels has not been demonstrated to increase effectiveness in general. This problem is greater for schizophrenia, however, than for most other chronic diseases, observed in 75% of patients with schizophrenia over a 2-year period after discharge from psychiatric hospitalization (85). Treatment nonadherence can result from intolerable side effects, lack of insight into illness that frequently accompanies schizophrenia, continued psychotic symptoms, and poor therapeutic alliance (85). Longacting depot formulations of some antipsychotic medications have helped the problem of unsatisfactory treatment adherence (85). This requires a multidisciplinary approach by a coordinated team of healthcare professionals and agencies delivering an assortment of vocational and educational services and rehabilitation in the community care setting (110). Ideally, care for patients with schizophrenia also provides support to families, who often end up being responsible for major aspects of the day-to-day care for their loved ones with schizophrenia. The first 2 or 3 years after the first onset of illness in schizophrenia are thought to be a period in which the illness is most modifiable and interventions may be most effective at reducing progression of the illness and its negative consequences (38, 39, 66, 100). In particular, greater duration of untreated psychosis has been found to be strongly predictive of clinical outcomes of schizophrenia, especially negative symptoms, quality of life, and functional capacity (3). These findings have prompted the development of specialist early intervention services providing intensive services for patients in their first psychotic episode and for the first 2 or 3 years (38, 39, 66, 100). These services have been demonstrated to have beneficial effects on outcome in the first few years (75), but their long-term effect remains uncertain (130). Duration of untreated psychosis in community treatment settings in the United States. Hippocampal volume is reduced in schizophrenia and schizoaffective disorder but not in psychotic bipolar I disorder demonstrated by both manual tracing and automated parcellation (FreeSurfer). Hallucinations in bipolar disorder: characteristics and comparison to unipolar depression and schizophrenia. The neuropathology of schizophrenia: a selective review of past studies and emerging themes in brain structure and cytoarchitecture. Differences in cognitive impairment between schizophrenia and bipolar disorder: considering the role of heterogeneity. Cognitive dysfunction in bipolar disorder and schizophrenia: a systematic review of meta-analyses. The role of dopamine in schizophrenia from a neurobiological and evolutionary perspective: old fashioned, but still in vogue. Heritability estimates for psychotic disorders: the Maudsley twin psychosis series. From linkage studies to epigenetics: what we know and what we need to know in the neurobiology of schizophrenia. Differences between early-phase primary psychotic disorders with concurrent substance use and substance-induced psychoses. When acute-stage psychosis and substance use co-occur: differentiating substance-induced and primary psychotic disorders. Treatment for outpatients with comorbid schizophrenia and substance use disorders: a review. Negative symptoms: history of the concept and their position in diagnosis of schizophrenia. Psychoses in the offspring of schizophrenic monozygotic twins and their normal co-twins. Impact of cognitive and social cognitive impairment on functional outcomes in patients with schizophrenia. Offspring of parents with schizophrenia: a systematic review of developmental features across childhood. Do all schizophrenia patients need antipsychotic treatment continuously throughout their lifetime
Many patients with dementia may present with depressive symptoms (74) or somatic complaints such as headache depression symptoms quiz discount bupron sr express, abdominal pain, and constipation. Others are brought to physicians by relatives because of temper outbursts, socially embarrassing behavior, or suspiciousness. Patients with depression may complain of poor memory, and some studies have revealed impairment of short-term memory in many such patients. Some have argued that the term "pseudodementia" can be misleading because depression may also include significant cognitive impairment as part of the clinical picture, especially in older patients. It has therefore been suggested that a more appropriate name for this condition might be "cognitive impairment of depression. Clearly the relationship between depression and cognitive impairment may sometimes be puzzling. It is important to recognize that some patients with depression, especially older ones, may present with enough cognitive difficulty to raise differential diagnostic problems. In such cases, physicians should be cautious about making a firm diagnosis and be prepared to change their diagnosis as the clinical picture unfolds. Sometimes, especially earlier in the illness, the patient may volunteer, "I keep losing things. Inability to follow directions and confusion about what others intend may lead to irritability and anger: "Nobody tries to explain things to me. The most important point about dementia is that in some cases the underlying illness is treatable (59). These cases should be recognized as early as possible because recovery may be related to the duration of the dementia. Recurrent hypoglycemia arising from insulin treatment of diabetes, pancreatic islet-cell tumors, or the too-rapid alimentary absorption of glucose in patients who have undergone subtotal gastric resection may also lead to severe dementia (10, 11, 25). Chronic alcohol abuse has been associated with a memory impairment (77, 79, 96) that is distinct from the Wernicke-Korsakoff syndrome and, if recognized early, often can be reversed by abstention from further drinking; however, debate continues about the validity of an alcoholinduced dementia separate from Wernicke encephalopathy or hepatic encephalopathy (113). Dementia caused by aluminum intoxication from the water used in such great quantities during chronic renal dialysis is now avoided through modern water purification techniques in use since 1980 (2, 92). Most cases of dementia are the result of intrinsic brain disease or arteriosclerotic changes in the blood vessels supplying the brain. The term "vascular dementia" is preferred over the older term "arteriosclerotic dementia," reflecting the recognition that the dementia results from loss of brain tissue. Finally, dementia may arise from more than one etiology and sometimes from multiple etiologies, making it difficult for clinicians to address the source of the problem (Box 13. Often it is impossible to determine the most crucial factor in a patient with simultaneous heart failure, infection, fever, and dehydration who is also receiving a variety of medications. Sometimes, when patients have been very sick and have had a prolonged delirium, many days pass after medical abnormalities are controlled before the mental picture clears. Frontotemporal dementias (including Pick disease) Dementia with Lewy bodies Parkinson disease with dementia Huntington disease Central nervous system disease 1. Brain injury (concussion/damage) Neoplasms Vascular disease Normal pressure hydrocephalus Viral/bacterial infections Subdural hematoma Chronic seizures Systemic disease 1. Nutritional deficits (niacin, B-12) Hepatic disease Renal disease Wilson disease Endocrine (hypothyroidism, hypoparathyroidism) Multiple sclerosis Chronic metabolic dysregulation (hypocalcemia, hypoglycemia) Autoimmune disease Immune system disease Cardiovascular disease Medication(s)/substance(s) 1. Alcohol dementia Adapted from diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision. Wernicke-Korsakoff syndrome develops after many years of heavy alcohol use and poor nutrition. Patients usually present in a marked delirious state without other classic signs of delirium tremens (autonomic instability and tremulousness). As the confusion clears, significant anterograde and retrograde amnesia become prominent. The deficit can be permanent (71), although in one series of patients, 20% did resolve (98). The early manifestations may be subtle, and only in retrospect does their significance become evident. Fatigability, moodiness, distractibility, depression, irritability, and carelessness may be present long before memory difficulty, intellectual deterioration, and disorientation can be clearly and easily detected. Depending on the underlying brain disease, the dementia may either stabilize for long periods or progress to total incapacity and death (17, 78, 97, 118). Certain vulnerabilities to this alteration, including age, illness, brain disease, or medication(s), may all play a part in this disorder. In their seminal work on delirium, published in 1959, Engel and Romano (41) reviewed signs of delirium and described "overall slowing of posterior background rhythm" (p. They reported the electrical changes as reversible and associated with the level of the disturbance. Wernicke-Korsakoff syndrome is widely accepted to be produced also by an extrinsic factor, namely thiamine deficiency. Because other causes of thiamine deficiency produce the same type of disorder, genetic factors have not generally been considered to actively contribute to the illness. However, a more recent review (104) has suggested some possible genetic contribution in thiamine-inadequate diets. The generally agreed-upon pathological lesions are located bilaterally in the temporal lobes and involve the associated hippocampus and mammillary body (57, 67). Over time, the anatomical findings (senile plaques, neurofibrillary tangles, and granulovacuolar degenerative changes) of the two groups of patients have been found to be similar (97, 118), as are the clinical presentations. Space limitation does not permit detailed review of these evolving efforts (literally thousands of references) proffered to assist the field. Fortunately, there is now widespread agreement that the central pathological changes in brain tissue are increased levels of amyloid- (A) peptide found extracellularly in neuritic plaques and microtubule assembly protein found in the cell and described as a neurofibrillary tangle composed of hyperphosphorylated tau (p-tau) (90). As these downstream neuropathological changes are being further defined, the upstream genetics, initiation, evolution, risk factors, and potential treatments are coming more into focus.
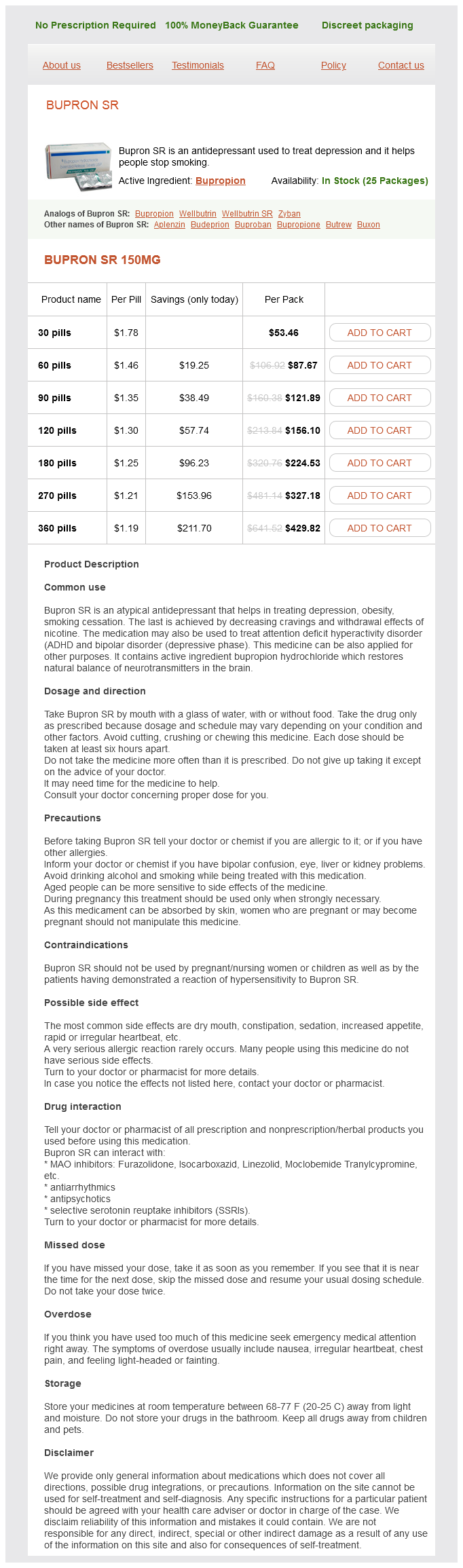
Bupron SR Dosage and Price
Bupron SR 150mg
- 30 pills - $53.46
- 60 pills - $87.67
- 90 pills - $121.89
- 120 pills - $156.10
- 180 pills - $224.53
- 270 pills - $327.18
- 360 pills - $429.82
Similar and dissimilar manifestations of obsessive-compulsive neurosis in monozygotic twins depression symptoms and cures bupron sr 150 mg buy amex. Obsessive-compulsive disorder: a double-blind trial of clomipramine and clorgyline. Managing the patient with treatmentresistant obsessive compulsive disorder: current strategies. Behavioral versus pharmacological treatments of obsessive compulsive disorder: a meta-analysis. Guideline Watch (March 2013): Practice Guideline for the Treatment of Patients with Obsessive Compulsive Disorder. Practice guideline for the treatment of patients with obsessive-compulsive disorder. Recent advances in Gilles de la Tourette syndrome: implications of clinical practice and future research. Gender differences in social and interpersonal features and personality disorders among Japanese patients with obsessive-compulsive disorder. Complex segregation analysis provides compelling evidence for a major gene underlying obsessive-compulsive disorder and for heterogeneity by sex. Return of symptoms after discontinuation of clomipramine in patients with obsessive-compulsive disorder. N-acetylcysteine augmentation therapy for moderate-to-severe obsessive-compulsive disorder: randomized, double-blind, placebo-controlled trial. A review of the efficacy of selective serotonin reuptake inhibitors in obsessive-compulsive disorder. Riluzole augmentation in treatmentrefractory obsessive-compulsive disorder: a pilot randomized placebo-controlled trial. Randomized controlled crossover trial of ketamine in obsessive-compulsive disorder: proof-of-concept. Behavioral therapy and serotonin reuptake inhibitor pharmacotherapy in the treatment of obsessive-compulsive disorder: a systematic review and meta-analysis of headto-head randomized controlled trials. Psychological treatment of obsessive-compulsive disorder in children and adolescents: a meta-analysis. Royal College of Psychiatrists of the National Collaborating Centre for Mental Health. Obsessive-compulsive disorder: core interventions in the treatment of obsessive-compulsive disorder and body dysmorphic disorder. Ein Beitrag zur Frage der Zwangskrankheit, insbesondere ihrer heriditären Beziehungen. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. A preliminary randomized double-blind clinical trial on the efficacy of celecoxib as an adjunct in the treatment of obsessive-compulsive disorder. Shortterm diagnostic stability of schizotypal, borderline, avoidant, and obsessivecompulsive personality disorders. Genomewide linkage scan for obsessive-compulsive disorder: evidence for susceptibility loci on chromosomes 3q, 7p, 1q, 15q, and 6q. Escitalopram in obsessive-compulsive disorder: a randomized, placebo-controlled, paroxetinereferenced, fixed-dose, 24-week study. A study of some clinical aspects of the relationship between obsessional neurosis and psychotic reaction types. Transcranial magnetic stimulation for obsessive-compulsive disorder: an updated systematic review and meta-analysis. Anorexia nervosa is characterized by peculiar attitudes toward eating and weight that lead to obsessive refusal to eat, profound weight loss, and, when the disorder occurs in girls, persistent amenorrhea. Bulimia refers to a behavior of gorging of food, typically followed by induced vomiting or purging. Bulimia is seen in many patients with anorexia nervosa, but it is the predominant clinical feature in bulimia nervosa (39). One of its early chapters, "Nervous Phthisis," contains case histories of the illness we recognize today as anorexia nervosa. Mary Axe, in the Year 1684 and the Eighteenth Year of her Age, in the Month of July fell into a total suppression of her Monthly Courses from a multitude of Cares and Passions of her Mind, but without any Symptoms of the Green-Sickness following upon it. The Spring following, by the Prescription of some Empirik, she took a Vomit, and after that I know not what Steel Medicine, but without any Advantage. I do not remember that I did ever in all my Practice see one, that was conversant with the Living so much wasted with the greatest degree of Consumption (like a Skeleton only clad with Skin) yet there was no Fever, but on the contrary a coldness of the whole Body; no Cough, or difficulty of Breathing nor an appearance of any other Distemper of the Lungs, or of any other Entrail; No Looseness, or any other sign of a Colliquation, or Preternatural expence of the Nutritious Juices. Only her Appetite was diminished, and her Digestion uneasy, with Fainting Fits, which did frequently return upon her. Which symptoms I did endeavor to relieve by the outward application of Aromatick Bags made to the Region of the Stomack, and by Stomach-Plaisters, as also by the internal use of bitter Medicines, Chalybeates, and Juleps made of Cephalick and Antihysterick Waters, sufficiently impregnated with Spirit of Salt Armoniack, and Tincture of Castor, and other things of that Nature. Another vivid and accurate description was presented in 1908 by Dejerine and Gauckler (18), as cited by Cowles (p. The abdominal wall sinks in below the floating ribs and forms a hollow like a basin. One would say it was the picture of an immured nun, such as the old masters have portrayed. Sometimes they seem to be sustained by some unknown miracle of energy; their voices are strong and their steps firm. On the other hand they often seem almost at the point of death and ready to draw their last breath. These patients are what are known as mental anorexics, who, without having any physical lesions, but by the association of various troubles, all having a psychic origin, have lost a quarter, a third, and sometimes a half of their weight.