General Information about Brahmi
Brahmi is a small, creeping herb with fleshy leaves and white or pale blue flowers. It has been used in conventional drugs as a brain tonic, promoting clarity, focus, and memory. In Ayurveda, it's categorized as a medhya rasayana, that means it's thought-about to be a rejuvenator of the mind. It is also known as the “Herb of Grace” as a end result of its capability to enhance mental clarity and cognitive operate.
Moreover, Brahmi has adaptogenic properties, which means it helps the body adapt to emphasize. It is usually used by students to improve concentration and retain data during exams. It can be beneficial for people with demanding jobs that require psychological agility and focus. By reducing stress and improving mental stamina, Brahmi can assist in learning and retaining info.
Brahmi also has a direct impression on the nervous system, serving to to manage the levels of a quantity of neurotransmitters, corresponding to dopamine and acetylcholine. These neurotransmitters are liable for a number of important functions, together with learning, reminiscence, and muscle movement. By balancing these ranges, Brahmi might help improve motor coordination and total mind operate.
Brahmi could be consumed in varied varieties, together with capsules, tablets, powders, and teas. Brahmi oil can be used in Ayurvedic massages to calm the mind and improve mind perform. It is relatively safe, with minimal unwanted facet effects, making it a popular herbal remedy for learning and reminiscence enhancement.
Brahmi, also recognized as Bacopa monnieri, is a strong herb broadly used in Ayurvedic drugs. It has been used for hundreds of years to boost memory, studying, and general cognitive function. This herb is native to India and has gained recognition all over the world for its quite a few health benefits, particularly for aiding learning and memory enchancment.
Another method Brahmi supports learning and reminiscence is through its capacity to minimize back irritation in the mind. Inflammation can cause damage to brain cells and disrupt the communication between them, leading to cognitive decline. Brahmi’s anti-inflammatory properties help to protect the brain, ensuring its correct functioning for optimum studying and reminiscence retention.
In addition to its results on learning and memory, Brahmi has additionally been proven to have mood-boosting properties. It is believed to reinforce the production of serotonin, often identified as the “happiness hormone,” resulting in a feeling of calmness and well-being. This makes it a valuable herb for these dealing with stress, nervousness, and despair.
In conclusion, Brahmi is a priceless herb with numerous well being benefits, together with its capability to enhance learning and reminiscence. Its neuroprotective, antioxidant, anti-inflammatory, and adaptogenic properties all contribute to its results on mind function, making it a potent aid for cognitive well being. Whether you are a scholar, a busy professional, or somebody trying to improve their mental performance, incorporating Brahmi into your every day routine could also be a useful addition. However, as with every complement, it's all the time greatest to seek the assistance of with a healthcare skilled earlier than incorporating it into your regimen.
One of the primary energetic compounds in Brahmi is bacosides, which have been discovered to have neuroprotective and antioxidant properties. These bacosides help to guard the brain against oxidative stress and promote the growth of latest nerve cells, probably explaining the herb’s cognitive advantages. Studies have proven that Brahmi can improve memory and learning talents, making it a wonderful help for college kids and people looking for to improve their cognitive abilities.
At this time treatment lung cancer order 60 caps brahmi with mastercard, the value of supratotal resection has not been confirmed in multi-institutional studies and is not widely accepted as routine clinical practice. Stereotactic computer-aided navigation systems represent the most widely used adjuvants to aid with surgical planning and resection. Although there are many branded varieties of this technology, the basic premise remains the same. They can also be coupled with functional imaging techniques, allowing surgeons to avoid eloquent areas or important white matter tracts during resection. The main drawback to navigation using preoperative imaging is that brain shift and distortion from tumor resection can render the system inaccurate as the surgery progresses. To address this issue, various intraoperative imaging techniques are being developed, a few of which are discussed here. It is administered orally prior to surgery and then visualized intraoperatively using an operating microscope capable of excitation with 405-nm wavelength blue light. Tumor cells fluoresce a violet-red color and can be distinguished from normal surrounding brain. Further studies have suggested that fluorescence correlates with anaplastic or high-grade foci, regardless of enhancement on preoperative imaging. The patient population was almost exclusively composed of those with high-grade, enhancing lesions. Because the assignments were randomized, the investigators were able to control for a variety of potential confounding factors including resectability, surgeon experience, and tumor size. This technique relies on the acoustic differences between tumor tissue and normal brain. Tumor tissue will appear as a hyperechoic mass on ultrasound, whereas normal brain is variably echoic and demonstrates a more typical gyral architecture. In addition, Doppler fiowmetry can be used to localize important blood vessels in real time. This study showed a survival benefit of 2 to 3 months from the addition of radiotherapy and a benefit of 4 to 5 months from combination radiotherapy and nitrosourea chemotherapy. Subsequent studies demonstrated that there was no difference in survival between whole brain radiation and partial brain radiation and that only a small number of patients had a recurrence outside a 2-cm margin after treatment. Survival after recurrence is highly dependent on patientspecific variables and ranges from 1 to 10 months. As expected, high~quality randomized data are not available currently, and practice patterns vary considerably across institutions. Consensus recommendations suggest that reoperation is indicated for patients who have recurrence in a noneloquent, operable area and have good performance status. The current data suggest a possible benefit in terms of survival, with the caveat that radiation~induced necrosis and other side effects need to be carefully managed. Bevacizumab (dis~ cussed later) has been studied extensively and can be used as salvage therapy in certain cases. This is important because the preservation of quality of life may take precedence over maximizing therapy in patients with the worst prognoses. Conversely, patients who are predicted to survive longest may warrant a more aggressive management paradigm. Each of these factors is assigned a point value, and the total of all the points for a given patient is then used to generate the median survival value based on a series of regression curves. Frontiers As previously mentioned, molecular characterization of tumors has fundamentally altered the concepts of tumor grade and how that relates to prognosis. More recent efforts are focused on using molecular data to generate prognostically meaningful classifications that are independent or work in parallel with more conventional methods. As we begin to understand more about the molecular biology of these tumors, these distinctions will become more important. Once tumor type-specific regimens have been developed, molecular classification schemes will ultimately come to inform not only prognosis but also treatment. Initial studies using hevacizumah for recurrent glioblastoma showed great promise, with = impressive regression of enhancement and edema noted on imaging. Both trials demonstrated no benefit to overall survival and had conflicting data on progression-free survival and quality-of-life measures. It is now primarily used in combination with other forms of chemotherapy for aggressive treatment of recurrent disease54 or as a single agent for the palliation of symptoms and decreasing corticosteroid dependence. All of these approaches are currendy highly experimental, but various clinical trials are enrolling patients to systematically test the efficacy of these approaches. The collective failure of so many different approaches to glioblastoma therapy has frustrated the field of neuro-oncology for decades. With more extensive molecular profiling, we are beginning to understand the underpinnings of treatment failure. Tumor heterogeneity-that is, the idea that cells within a tumor have drastically different genetic, epigenetic, and phenotypic characteristiC£-is emerging as a key factor underlying the failure of various therapeutic approaches. The origins of this idea came from studies that demonstrated the presence of privileged subpopulations of cells with tumorinitiating activity, 58·59 resistance to radiation, 60 angiogenic properties,61 ·62 and the ability to repopulate tumors following chemotherapy. Heterogeneity observed in primary patient tumor samples64 suggests that strategies aimed at targeting multiple pathways and cell types within a tumor are far more likely to be successful. Moreover, the plasticity of glioblastoma makes it a unique challenge, as our therapeutic efforts are trying to stay ahead of a tumor that is constandy changing and evolving. Mainstays of therapy include maximal surgical resection, followed by adjuvant radiation and chemotherapy. Once controversial, the role of maximal, safe resection is now fairly well established as a predictor of patient outcome. Various techniques to improve the extent of resection have been developed and are currendy making their way into routine clinical practice.
Atherosclerotic intracranial arterial stenosis: risk factors medicine yeast infection trusted brahmi 60 caps, diagnosis, and treatment. A direct aspiration first-pass technique vs stentriever thrombectomy in emergent large vessd intracranial occlusions. Conclusion Endovascular treatment has revolutionized the management of acute stroke and occlusive cerebrovascular disease. Heart Disease and Stroke StatistiOl-2016 Update: A Repon From the American Heart Association. Coronary and cerebrovascular atherosclerosis: two aspects of the same disease or two different pathologies Correlation of the extent and severity of atherosclerosis in the coronaty and cerebral aneries. National Institutes of Health stroke scale score and vessel occlusion in 2152 patients with acute ischemic stroke. National Institutes of Health Stroke Scale for prediction of proximal vessel occlusion in anterior circulation stroke. Simple clinical predictors of stroke outcome based on National Institutes of Health Stroke scale score during 1-h recombinant tissue-type plasminogen acrivator infusion. National Institutes of Health stroke scale item profiles as predictor of patient outcome: external validation on independent trial data. National Institutes of Health Stroke Scale Item Profiles as Predictor of Patient Outcome: External Validation on Safe Implementation of Thrombolysis in Stroke-Monitoring Study Data Stroke. Association of early National Institutes of Health Stroke Scale improvement with vessel recanalization and functional outcome after intravenous thrombolysis in ischemic stroke. Outcomes of intravenous thrombolysis in posterior versus anterior circulation stroke. Association of laterality and size of perfusion lesions on neurological deficit in acute supratentorial stroke. National Institutes of Health Stroke Scale score is an unreliable predictor of perfusion deficits in acute stroke. Magnetic resonance imaging versus computed tomography for detection of acute VllScular lesions in patients presenting with stroke symptoms. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Acute human stroke studied by whole btain echo planar diffWion-weighted magnetic resonance imaging. Validity and tdiability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. Computed tomographic angiography findings in 103 patients following vascular events in the posterior circulation: potential and clinical relevance. Role ofCf angiography in patient selection for thrombolytic therapy in acute hemispheric stroke. Systematic review of computed tomographic angiography for assessment of carotid artery disease. Perfusion-Cf assessment of infarct core and penumbra: receiver operating characteristic curve analysis in 130 patients suspected of acute hemispheric stroke. Existence of the diffusion-perfusion mismatch within 24 hours after onset of acute stroke: dependence on proximal arterial occlusion. Beyond mismatch: evolving paradigms in imaging the ischemic penumbra with multimodal magnetic resonance imaging. Cortdation between cerebral blood volume values and outcomes in endovascular therapy for acute ischemic stroke. Pre-intervention cerebral blood volume predicts outcomes in patients undergoing endovascular therapy for acute ischemic stroke. Association of Cf perfusion parameters with hemorrhagic transfonnation in acute ischemic stroke. Analysis of tissue plasminogen activator eligibility by sex in the Greater Cincinnati/ Northern Kentucky Stroke Study. Techniques for endovascular treatment of acute ischemic stroke: from intra-arterial fibrinolytics to stent-retrievers. The Penumbra system for mechanical thrombectomy in endovascular acute ischemic stroke therapy. The penumbra pivotal stroke trial: safety and effectiveness of a new generation of mechanical devices for dot removal in intracranial large vessel occlusive disease. Comparison of endovascular treatment approaches for acute ischemic stroke: cost effectiveness, technical success, and clinical outcomes. Management of acute ischemic stroke due to tandem occlusion: should endovascular recanalization of the extracranial or intracranial occlusive lesion be done first Stentor balloon: How to treat proximal internal carotid anery occlusion in the acute phase of ischemic stroke Acute ischemic stroke in the setting of cervical carotid occlusion: a proposed management strategy. Carotid stenting and intracranial thrombectomy for treatment of acute stroke due to tandem occlusions with aggressive antiplatdet therapy may be associated with a high incidence of intracranial hemorrhage. Stent-Rctriever Thrombectomy for Acute Anterior Ischemic Stroke with Tandem Occlusion: A Systematic Review and Meta-Analysis. Outcome after mechanical thrombectomy using a stent retriever under conscious sedation: comparison between tandem and single occlusion of the anterior circulation.
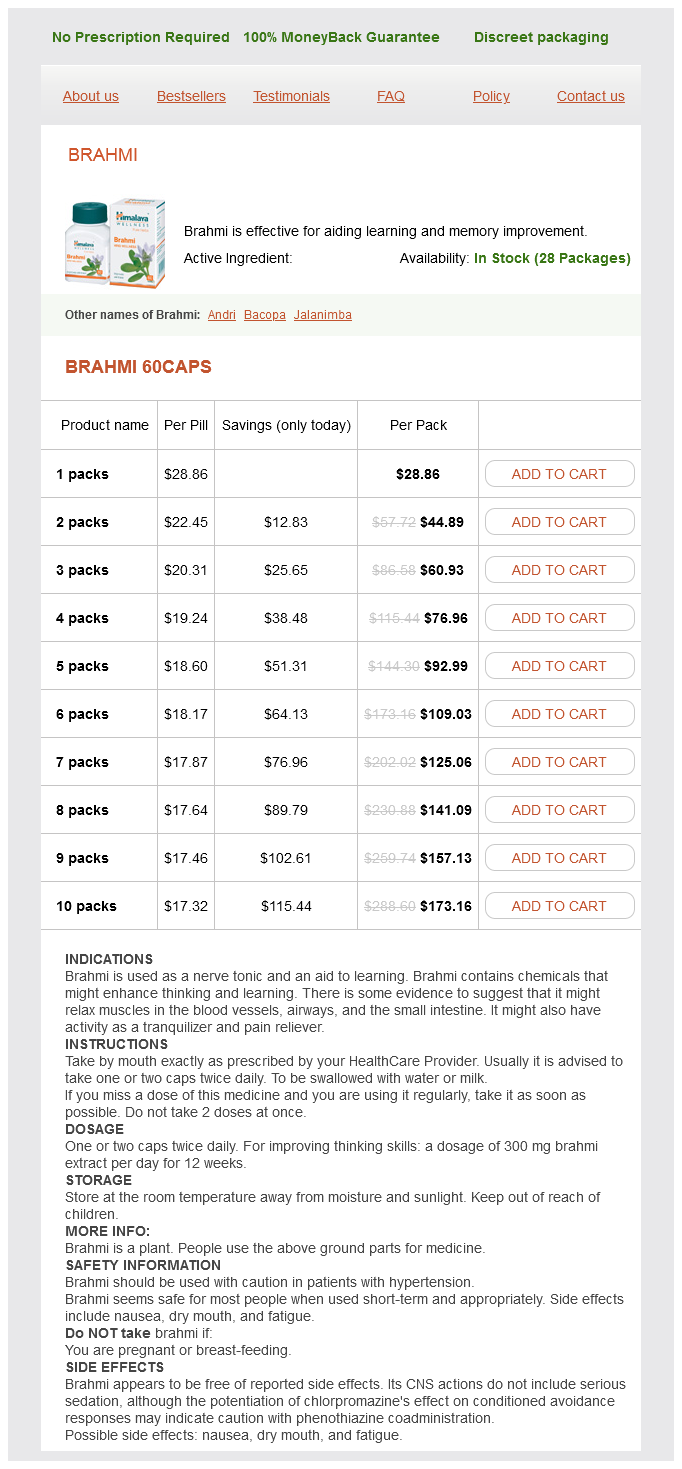
Brahmi Dosage and Price
Brahmi 60caps
- 1 packs - $28.86
- 2 packs - $44.89
- 3 packs - $60.93
- 4 packs - $76.96
- 5 packs - $92.99
- 6 packs - $109.03
- 7 packs - $125.06
- 8 packs - $141.09
- 9 packs - $157.13
- 10 packs - $173.16
Effect of mannitol and hyptenonic saline on cerebral oxygenation in patients with severe traumatic brain injury and refractory intracranial hypenension treatment that works discount brahmi 60 caps free shipping. Hyperosmolar agents in neurosurgical practice: the evolving role of hypertonic saline. A systematic review of randomized controlled trials comparing hypenonic sodium solutions and mannitol for traumatic brain injury: implications for emergency depanment management. Thromboembolism after trauma: an analysis of 1602 episodes from the American college of surgeons national trauma data bank. Three thousand seven hundred thirty-eight posttraumatic pulmonary emboli: a new look at an old disease. Prospective evaluation of the safety of enoxaparin prophylaxis for venous thromboembolism in patients with intracranial hemorrhagic injuries. Early venous thromboembolism prophylaxis with enoxaparin in patients with blunt traumatic brain injury. Tuning for deep vein thrombosis chemoprophylaxis in traumatic brain injury: an evidence-base review. External ventricular drain versus intraparenchymal intracranial pressure monitors in traumatic brain injury: a prospective observational study. Brain tissue oxygen monitoring in traumatic brain injury and major trauma: outcome analysis of a brain tissue oxygen-directed therapy. Brain tissue oxygendirected management and outcome in patients with severe traumatic brain injury. High-dose barbiturates control dcvatcd intracranial pressure in patients with severe head injury. The free radical pathology and the microcirculation in the major central nervous system trauma. Lactate and excitatory amino acids measured by microdialysis are decreased by pentobarbital coma in head-injured patients. Propofol in the treatment of moderate and severe head injury: a randomized, prospective double-blinded pilot trial. A randomized, double-blind study of phenytoin for the prevention of posttraumatic seizures. Levctiracctam versus phenytoin for seizure prophylaxis in severe traumatic brain injury. Prospective, randomized, single-blinded comparative trial of intravenous levetirace-tam versus phenytoin for seizure prophylaxis. The outcome from severe head injury with early diagnosis and intensive management. Predicting the need for operation in the patient with an occult traumatic intracranial hematoma. Continuous monitoring of jugular venous oxygen saturation in head-injured patients. The effect of intracen:bral hematoma location on the risk of brain-stem compression and on clinical outcome. Decompressive craniectomy for the treatment of refractory high intracranial pressure in traumatic brain injury. Craniotomy versus craniectomy for acute uaumatic subdural hematoma in the united states: A national retrospective cohon analysis. Structured intcrview5 for the Glasgow outcome scale and the extended Glasgow outcome scale: guiddines for their use. Disproponionatdy severe memory deficit in rdation to normal intdlectual functioning after closed head injury. A survey ofthe brain injury special interest group of the American academy of physical medicine and rehabilitation. Association of traumatic brain injury with subsequent neurological and psychiattic disease: a meta-analysis. Knowledge of the aforementioned neurophysiological principles is important in understanding the mechanism of action and application oftherapeutic interventions in a neuro-critical care setting. Initial assessment of the critically ill neurosurgical patient requires a systemic, methodical and reproducible approach to identify, resuscitate and treat life-threatening insults in the most important sequence in which they occur. A variety of techniques allow the multi-modal monitoring of critically ill neurosurgical patients allowing individualisation of treatment; trends and variability over a time course provide more useful information than isolated measurements. Complications that are general to all neurosurgical patients, and those that are specific to the each neurosurgical pathology should be investigated for an identified in a deteriorating critically ill neurosurgical patient. The diagnosis of brain death is important in critically care settings and familiarity with institutional, regional and national guidance is essential. The nervous system is vulnerable not only to effects from the initial insult it suffers from a pathologic process (primary brain or spinal cord injury) but also to systemic factors, which exacerbate this primary injury (ie, secondary brain or spinal cord injury). This spectrum includes patients admitted in extremis following their initial injury for preoperative optimization and stabilization, patients in the immediate postoperative phase following elective surgery, and any previously stable patient in a ward setting that suffers a neurologic deterioration. The reader is advised to refer to the variety of excellent monographs and texts on the subject where necessary. The regulatory changes in flow-metabolism coupling have a short latency (~ 1 sec) and are mediated by regional metabolic and neurogenic factors. This leads to an increased washout of these factors with an associated reduction in flow. Absorption is via arachnoid granulations and villi into dural venous sinuses and is dependent on venous pressure.