General Information about Benemid
Benemid is out there in both pill and injectable type. The recommended dose is usually 250 mg twice a day, though this may range relying on the severity of the condition and response to therapy. It is important to notice that whereas Benemid can help decrease uric acid ranges, it does not provide instant reduction from gout signs. Therefore, different medications might need to be prescribed for acute relief throughout gout attacks.
In conclusion, Benemid is a priceless medication for the remedy of gout and different situations caused by high ranges of uric acid within the body. It offers an alternate option for those who cannot take different medications for gout and has been proven to be effective in lowering uric acid ranges. However, as with any treatment, you will want to use Benemid as prescribed and underneath the steerage of a healthcare professional.
Like any medication, Benemid just isn't without its unwanted effects. The most common side effects embrace abdomen upset, headache, dizziness, and pores and skin rash. In uncommon circumstances, it could additionally cause more critical side effects like kidney stones, low platelet count, and blood disorders. As with any medication, you will need to consult with a doctor before beginning Benemid and report any unwanted aspect effects skilled.
Benemid, also called probenecid, is an anti-gout agent that has been used for over 60 years to treat symptomatic hyperuricemia, a condition in which there's extra uric acid in the physique. It works by blocking the reabsorption of uric acid within the kidneys, allowing the excess uric acid to be excreted by way of urine. This results in a decrease in the general levels of uric acid within the physique and reduces the chance of gout assaults.
In addition to treating gout, Benemid has additionally been found to be efficient in the therapy of different circumstances such as sure kinds of kidney stones and a rare genetic dysfunction known as familial juvenile hyperuricemic nephropathy. It has also been used off-label for the remedy of certain infections and to increase the plasma ranges of certain antibiotics.
Gout is a common form of arthritis that entails sudden, severe assaults of ache, redness, swelling, and tenderness in the joints. It is attributable to high ranges of uric acid within the body, which might crystallize and form deposits in the joints, resulting in painful flare-ups. Though there are numerous therapies available for gout, one medicine particularly stands out for its capacity to prevent the formation of uric acid - Benemid.
Benemid is primarily utilized in sufferers who can't take other drugs such as allopurinol or febuxostat, which are commonly prescribed for gout, due to both unwanted effects or allergic reactions. It is also used in combination with these drugs for patients who don't respond properly to them. In addition, Benemid is used as a prophylactic remedy to prevent recurrent gout assaults.
Higher pressure within the tumor and permeable tumor vessels initiates hydrostatic flow away from the tumor margin and into the extracellular space surrounding it until it reaches (convects to) the ventricles and subarachnoid spaces pain treatment clinic order cheap benemid. There are dynamic limits to resorption: local capillaries absorb extracellular fluid slowly (estimated at 0. Although ineffective for cytotoxic edema and only modestly but transiently efficacious in the short-term treatment of interstitial edema, glucocorticoids can improve the neurological symptoms and signs caused by vasogenic edema, especially in patients with brain tumors, in whom the clinical features often result from the mass contributed by the peritumoral edema. The blood-brain barrier: an overview: structure, regulation, and clinical implications. Mechanism of dexamethasone suppression of brain tumor-associated vascular permeability in rats. Aquaporin-4 deletion in mice reduces brain edema after acute water intoxication and ischemic stroke. A reassessment of vascular endothelial growth factor in central nervous system pathology. Tumor cells secrete a vascular permeability factor that promotes accumulation of ascites fluid. Tight junctions of the blood-brain barrier: development, composition, and regulation. Diuretics, such as the loop diuretic furosemide, act by inducing systemic dehydration, which may reverse osmotic flow. Furthermore, prolonged use of osmotic agents can lead to the accumulation of solute (mannitol, glycerol) within the tissues, which can then serve as a "reverse sink" and produce a circumstance in which the edema is refractory to further osmotic therapy. Agents such as mannitol or hypertonic saline may also have other actions, such as vasoconstriction, enhanced cerebral blood flow, and altered rheology, among others, that can alter the content or effect of edema. Many free radical scavengers and neuroprotective agents that have shown promise in the laboratory or in animal models have generally failed in human trials. Whether new agents that modulate the activity of aquaporins, corticotropin-releasing hormone, sulfonylurea receptor 1, or other pathways will prove effective awaits new human trials. The exquisite sensitivity of the central nervous system to physical and chemical injury has led to an ingenious series of protective and homeostatic systems that shroud, nurture, nourish, and maintain maximal function. These highly developed protective systems can become detrimental, however, under certain pathologic conditions. In particular, encasement of brain tissue in a rigid structure (the skull) places an important constraint on the refined interplay between cerebral homeostatic processes, namely, volume regulation. These ideas later became recognized as the Monro-Kellie doctrine, which is formalized physiologically later. Quincke3 first described lumbar puncture for the relief of "brain pressure" in 1911. Cardiac and respiratory activity creates pulsatile components by cyclic changes in cerebral blood volume. Left ventricular contraction contributes the cardiac component, which has a frequency similar to the peripheral arterial pulse. Early studies suggested that the choroid plexus and pial arteries were responsible,6 although more recent analysis has implicated the high-compliance venous blood vessels. During inspiration, there is a fall in arterial blood pressure and an increase in pressure gradient from cerebral veins to central venous capacitance vessels. This gradient drives cerebral venous return, which is therefore increased on inspiration, with a concomitant drop in cerebral blood volume. Monro,1 in his seminal work on the brain and nervous system, wrote: For, as the substance of the brain, like that of other solids of our body, is nearly incompressible, the quantity of blood within the head must be the same, or very nearly the same at all times, whether in health or disease, in life or after death, those cases only excepted in which water or other matter is effused, or secreted from the blood vessels; for in these a quantity of blood, equal in bulk to the effused matter, will be pressed out of the cranium. Some years later, at a meeting of the Medico-Chirurgical Society of Edinburgh, George Kellie2 presented a report in which he advanced this idea and stated: If these premises be true, it does not then appear very conceivable how any portion of the circulating fluid can ever be withdrawn from within the cranium, without its place being simultaneously Deceased. Pressures are usually reported in units of either millimeters of water (mm H2O) or millimeters of mercury (mm Hg). This convention arose because a fluid column will exert a pressure at its base proportional to the height of the column (h), the density of the fluid (), and the gravitational constant (g). Because, for a given fluid, g and are constant, pressures can be compared by relation to the height of a given fluid. As with any column of fluid, the skull and spinal canal experience hydrostatic pressure caused by the weight of their contents. The contribution of hydrostatic pressure depends on the weight of fluid and tissue above the point of measurement, divided by the cross-sectional area at that level. The filling pressure of the system is determined by the volume of the intracranial contents and the elastance of the enclosing structures. Elastance is a system parameter that is defined by the pressure change per unit of volume change,13 namely, the corresponding pressure change for any given volume increase in craniospinal contents. The relationship is not necessarily linear across all volumes and not necessarily constant under all physiologic conditions. In other words, as volume is added to the system, there are two principal routes for compensation, either expansion or loss of volume. These concepts are expounded on subsequently in the discussion of nonsteady-state dynamics. Atmospheric pressure, hydrostatic pressure, and filling pressure all contribute to the concept of steady-state dynamics. Thebaseline pressure level is affected by rhythmic components caused by cardiorespiratory activity. The tidal wave and the dicrotic wave are separated by the dicrotic notch, which corresponds to the dicrotic notch in the arterial pulse waveform.
They found that deterioration was less likely after right subthalamotomy (5% decline in cognitive test scores) than left subthalamotomy (25% decline) heel pain treatment exercises purchase benemid american express. These patients also showed a significant improvement in apathy and depression test scores (Hamilton Depression Rating Scale) after surgery. Hyperactive behaviors, such as lack of inhibition and hypomania, occurred in five patients. This new behavior or mood change was severe 1 month after the procedure but gradually diminished by 1 year after surgery. However, bilateral lesions should be carefully considered in patients who exhibit speech problems preoperatively. Indeed, other avenues and approaches now dominate the scientific and clinical thinking with regard to neurodegeneration. Whether these more fashionable treatments will prove right or wrong is yet to be seen. In the meantime, we continue to search for a way to change the natural history of the disease. Ipsilateral side and axial signs worsen, however, during the postsurgical assessment period. Tremor, rigidity, and bradykinesia are alleviated, and these benefits are Full references can be found on Expert Consult @ Alterman Torsion dystonia is a neurological disorder characterized by twisting, repetitive movements that result in abnormal, often painful postures. Dystonia is not one disease; rather, it is a neurological manifestation of many pathologic conditions, most of which are poorly characterized. Prevalence estimates for primary dystonia in the general population range from 2 to 50 cases per million for early-onset dystonia and from 30 to 7320 cases per million for late-onset dystonia. Because of space constraints, discussion of alternative therapeutic targets for stimulation is limited. Consequently, this is a heterogeneous patient population with varied pathophysiologies and responses to treatment. Additional medications for dystonia include baclofen, benzodiazepines, and tetrabenazine. A minority of patients with symptomatic generalized dystonia will benefit from specific therapy targeted at the underlying disorder. At least 13 different mutations are now associated with dystonia, with each mutation occurring at a unique gene locus. Historically, surgical interventions for dystonia have targeted both the peripheral and central nervous systems. Failure to perform any of these three steps properly may lead to suboptimal results. Therefore, it is important to have all surgical candidates evaluated by a movement disorders neurologist before proceeding. The neurologist will ensure that the diagnosis of dystonia is correct and that all reasonable medical therapies have been tried. If painful muscular spasms or abnormal postures make awake surgery arduous, conscious sedation with propofol or dexmedetomidine can be used. Antibiotics are administered intravenously during application of the head frame so that serum levels are therapeutic during the implantation procedure. The thickness of the axial slices (3 mm) required to generate these high-resolution images increases our initial targeting error along the z-axis. Moreover, contrast enhancement demonstrates the cortical veins so that they may be avoided when selecting an entry point. These advanced software packages provide at least five distinct advantages: (1) the target coordinates are calculated automatically, thereby eliminating human math errors; (2) a variety of image sets. The calculated target point should be visualized on both axial and coronal images and should lie 2 to 3 mm superior and lateral to the optic tract. Our preferred trajectory rises at a 60- to 65-degree angle anterior and superior to the intercommissural plane and 0 to 10 degrees lateral to the vertical axis. C-arm fluoroscopy is used to confirm that the lead has traveled to the desired point relative to the frame. Testing is performed in bipolar mode with the following parameters: pulse width, 90 µsec; frequency, 130 Hz; and amplitude, 0 to 4 V. Stimulation amplitudes greater than 4 V are not used because we have never required amplitudes this great for therapy. Therefore, a lack of improvement in response to intraoperative stimulation should not be viewed as an indicator of poor lead placement. Sustained time- and voltage-locked contractions of the contralateral hemibody or face, or both, indicate that stimulation is activating the fibers of the internal capsule, in which case the lead is placed too medially or posteriorly, or both. Induction of phosphenes in the contralateral visual field suggests that stimulation is activating the optic tract and the lead is too deep. Fluoroscopy is used to confirm that the lead was not displaced from its desired position during fixation. The remaining length of the lead is encircled around the bur hole cap and left in the subgaleal space. The incision is irrigated with antibiotic-containing saline and closed anatomically. Patients are observed overnight in the neurosurgical intensive care unit and discharged the following day. The connection between the lead and the extension cable is placed under the galea, just lateral to the cranial incision, to limit exposure of the lead to potential fracture through movement. In very young patients with thin skin, one may place the pulse generator or generators at the abdomen. There is no consensus regarding the optimal settings for treating dystonia because few systematic evaluations of varying stimulus parameters have been conducted. Instead, therapy is currently guided by published case series, which report positive responses with wide pulses (210 to 400 µsec) and high frequencies (130 Hz).
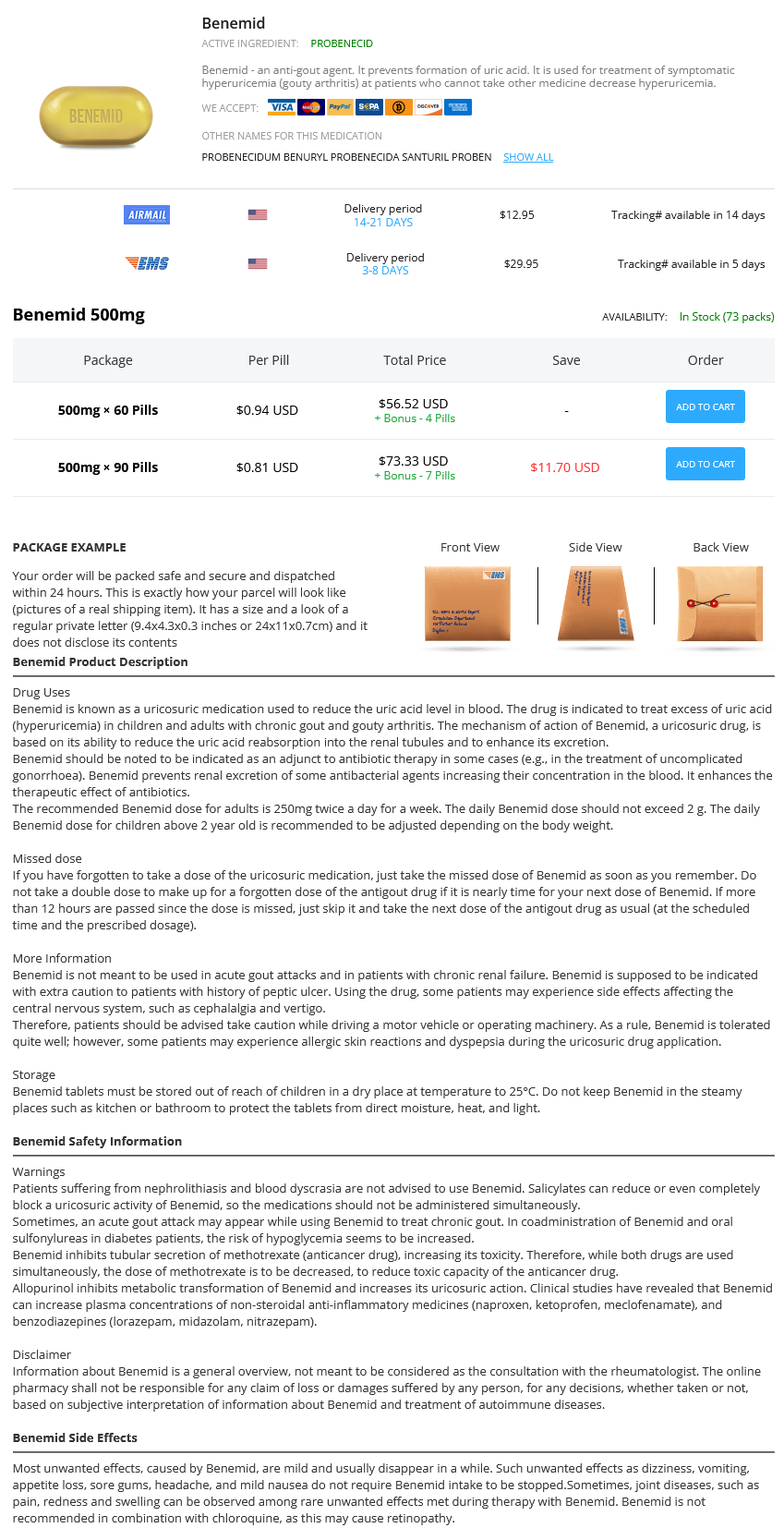
Benemid Dosage and Price
Benemid 500mg
- 60 pills - $56.52
- 90 pills - $73.33
This avoids a scenario in which the divided stump retracts into the perimesencephalic cistern and causes subarachnoid hemorrhage joint pain treatment for dogs cheap benemid 500 mg buy on-line. After the hippocampal sulcus is divided, the hippocampus and any remaining parahippocampus can be gently peeled off the underlying pia and removed to be sent to pathology for study. The mesial resection is then assessed and any remaining accessible posterior hippocampus removed. The posterior cut across the tail of the hippocampus ideally should allow for 3 to 4 cm of hippocampus to be removed. When the resection is complete, hemostasis is achieved by time, irrigation, and the judicious use of hemostatic materials. Bipolar coagulation of bleeding points in the mesial temporal or sylvian fissure region is best avoided to prevent injury to underlying structures. Similar bleeding points in the residual amygdala tissue are also best treated with application of hemostatic agents, irrigation, and time. The cavity is then filled in with saline and the dura closed in watertight fashion. The craniotomy flap is attached with titanium fixation and the muscle sewn together and reapproximated to the residual cuff. The skin is then closed in anatomic layers over a subgaleal drain to reduce postoperative swelling. Long-term seizure-free outcomes after temporal lobectomy, especially when performed for mesial temporal sclerosis, are often stated to be the best of all surgical procedures for medically resistant epilepsy. A number of long-term studies following patients for 5 to 10 years after surgery describe an initial seizure-free rate reaching 80%, which then noticeably declines over time to a 5-year seizure-free rate of about 50%. Hemiparesis may also result from manipulation or retraction injury of the ipsilateral cerebral peduncle. This type of postoperative deficit generally improves with time and is best avoided by limiting retraction during surgery on the roof of the temporal horn. Other neurological complications encountered include horizontal and vertical diplopias resulting from irritation to the third and fourth cranial nerves, respectively. These usually resolve over a few months and may need to be treated with ocular patching therapy. Fourth cranial nerve dysfunction is likely the less frequent cause of diplopia, although because it is difficult to diagnose, it may be underrecognized. The patient typically complains of double vision, especially when descending stairs or looking down. The nerve is vulnerable during temporal lobectomy because it travels under the medial edge of the tentorium, and injury is best avoided by limiting pressure or coagulation in this region. These are generally characterized by perseveration, naming difficulties, paraphasias, and word substitutions. Fortunately, these are usually transient and peak 24 to 48 hours after surgery before resolution. Although the exact cause is unknown, this language disturbance can be quite severe when it occurs. Potential mechanisms include retraction and ischemic infarction of comprehensive language cortex and resection of anterior and basal temporal lobe language sites that ultimately are not essential language sites. Strategies to avoid injury to the posterior temporal neocortex during surgery include minimizing retraction during removal of the posterior hippocampus and protecting the arterial and venous structures serving this area. Outcome analysis is extremely important in this group of patients because questions regarding return to employment, driving, and cessation of medication hinge on the success of surgery. Concrete information regarding potential risks and benefits of anticonvulsant withdrawal are necessary to allow these patients to reintegrate into society safely without medications. The National Library of Medicine has indexed more than 4400 articles that focus on epilepsy surgery, and 75% of these were published after 1990. In general, the neurosurgical risks that need to be discussed with the patient include the general risks of craniotomy and the more specific risks of manipulating the temporal lobe. General complications include infection (wound, craniotomy, meningitis, urine), hemorrhage (wound, epidural, subdural, intracerebral), red blood cell transfusion related to acute blood loss anemia, deep venous thrombosis, anesthetic complications, and death. The incidence of mortality after temporal lobectomy is approaching zero as experience and technology improves. Common postoperative conditions (not complications) include headache, wound swelling, jaw discomfort, retro-orbital pain, and cosmetic deformity. These conditions largely resolve over 2 to 3 months, although preoperative headaches and temporomandibular joint dysfunction can predispose the patient to a longer recovery period after surgery. Visual field loss after temporal lobectomy is related to injury of the geniculocalcarine fibers as they make their way from the lateral geniculate body to the occipital cortex. Its variable course and lack of anatomic distinction at surgery make it a difficult structure to protect. The incidence of superior quadrantanopsia reported on retrospective studies is variable, but likely a realistic estimate is 35% to 50% after standard temporal lobectomy. The optic tract can also be injured in the prethalamic region by dissections that stray too far superiorly at the level of the amygdala and anterior hippocampus. Finally, a contralateral hemianopsia may accompany a hemiparesis when damage to the anterior choroidal artery occurs in its cisternal segment. This artery is an important structure to protect during removal of the mesial structures. Many patients have significant neuropsychological deficits before surgery thought to be related to damage to the mesial temporal lobe structures involved in memory as well as the effects of anticonvulsant therapy on normal cortical tissue.