General Information about Baycip
Baycip has additionally been found to be effective in treating infections in oncology patients. These patients are often more prone to infections as a result of their weakened immune techniques, making it essential to discover a powerful and dependable therapy. Baycip has been confirmed to be effective in treating infections in oncology sufferers, giving them an opportunity to recuperate and continue their treatment with out the added issues of an an infection.
The active ingredient in Baycip is ciprofloxacin, a broad-spectrum antibiotic that's efficient towards both gram-positive and gram-negative bacteria. It works by inhibiting the growth and reproduction of bacteria, effectively stopping the unfold of infection. This makes it a key medicine for treating critical infections that may probably be life-threatening if left untreated.
One of the distinct advantages of Baycip is its rapid absorption into the urinary tract. This makes it a superb choice for treating urinary tract infections, as it may possibly quickly reach the affected area and begin working its bactericidal results. By focusing on the micro organism liable for the infection, Baycip works to get rid of the purpose for the an infection, rather than simply treating the signs.
Speaking of unwanted effects, Baycip is mostly well-tolerated by patients. However, like all medicine, it could trigger some adverse reactions in some individuals. These can embrace nausea, diarrhea, headaches, and dizziness. It is necessary to tell your doctor should you expertise any of those symptoms or any other uncommon unwanted effects while taking Baycip.
The really helpful dosage and period of treatment with Baycip could differ relying on the condition being treated, the severity of the infection, and the patient's general well being. It is necessary to follow the directions of a healthcare skilled when taking this medicine to make sure its effectiveness and avoid any potential side effects.
Baycip is a powerful and efficient drug that has been used to deal with a broad range of infections since its discovery. The medicine has gained recognition amongst healthcare professionals as a end result of its capacity to effectively fight urinary tract infections together with different critical circumstances. Baycip is understood for its fast absorption into the physique, as nicely as its long-term effuse and bactericidal results on a selected micro organism, Pseudomonas aeruginosa. This makes it an ideal alternative for treating numerous infections in oncology sufferers.
In addition to its effectiveness towards urinary tract infections, Baycip can also be prescribed for a selection of different situations. These embody respiratory infections, pores and skin and soft tissue infections, bone and joint infections, and digestive tract infections attributable to micro organism similar to salmonella, shigella, and campylobacters. This broad spectrum of coverage makes it a flexible drug that can be used in varied medical settings.
In conclusion, Baycip is a extremely efficient and versatile drug that is extensively used within the remedy of various infections. Its quick absorption, long-term efficacy, and bactericidal effects make it a go-to treatment for healthcare professionals in numerous medical settings. Its capacity to deal with infections in oncology sufferers has also made it an essential tool in the battle against serious diseases. If prescribed by a well being care provider, Baycip can successfully eliminate infections and assist sufferers on their street to restoration.
Endoscopic retrograde cholangiopancreatography cholangiogram shows a gallstone noted in a gallbladder remnant in this patient who had a history of a difficult cholecystectomy symptoms 24 baycip 500mg order on-line. However, many studies have more recently reported the safety and efficacy of endoscopic or percutaneous balloon dilation and/or stenting as a less invasive means of treating such problems (Gouma, 2007; Kassab et al, 2006; Vitale et al, 2008) (see Chapters 27, 29, and 30). Although safe and reasonably effective, these methods do generally require prolonged courses with repeated stent changes. Surgery remains the mainstay for treatment of major duct transections, ligations, many sizable strictures, and in cases where endoscopic/percutaneous approaches are unsuccessful. More detailed discussion of both benign and malignant strictures can be found elsewhere in this text. When constricted, this sphincter impairs forward flow of both bile and pancreatic juices. The sphincter of Oddi has three main functions: regulation of flow into the duodenum, prevention of reflux from the duodenum into the bile duct and pancreatic duct, and filling of the gallbladder. However, this test is invasive and does carry risk of complication, especially in the setting of a normal-caliber bile duct (Freeman et al, 1996; Maldonado et al, 1999; Sherman et al, 1990). There are noninvasive techniques that are reproducible but less accurate (Cicala et al, 1991, 2002; Corazziari et al, 1994; Madacsy et al, 2000; Sostre et al, 1992; Thomas et al, 2000). Because no clear etiology is derived from serology, imaging, or history, pancreatitis in this setting is often labeled idiopathic. The diagnosis should be considered in patients presenting with recurrent, biochemically proven episodes of pancreatitis without any alternative etiology. In patients with this presumed diagnosis, one prospective cohort study has shown that operative division of the sphincter of Oddi prevented recurrent episodes of pancreatitis in a large majority of patients (Toouli et al, 1996). Whether endoscopic approaches can provide similar efficacy is questionable (Behar et al, 2006; Elton et al, 1998; Tarnasky et al, 1998). All patients must have moderate to severe pain in the epigastrium and/or right upper quadrant abdominal that lasts 30 minutes or longer, recurs at different intervals, builds to a steady level, and is not relieved by bowel movements, postural change, or antacids. These are the baseline criteria for functional gallbladder or sphincter of Oddi disorder. Ultrasound carries the potential to distinguish between obstructive and nonobstructive pathologies in as many as 95% of patients and can establish the cause of an obstruction in as many as 85% (Baron et al, 2002; Eisen et al, 2001; Gandolfi et al, 2003). In the early postoperative period, ultrasound is particularly useful in identifying fluid collections such as bilomas, abscesses, or hemorrhage. If fluid collections are large, ultrasound-guided aspiration and culture is then performed. If the character of the collection is bilious or purulent, drainage catheters are left in place. Bile leaks can be managed conservatively or via endoscopic techniques with high rates of success as described earlier. In this way, ultrasound allows early triage of postcholecystectomy intraabdominal collections. Visualizing the pancreatic duct is also quite difficult with ultrasound, because overlying gas from the stomach or intestines often obscures the acoustic windows. The prevalence appears to be 1% to 20%, with the wide discrepancy in quoted frequencies likely attributable to heterogeneity in populations and in study conduct. First, continuous flux of bile into the duodenum can result in increased amount of bile acids entering the colon, leading to a secretory diarrhea (Arlow et al, 1987). Bile acid malabsorption may also be involved and may synergize with this effect in promoting diarrhea (Ford et al, 1992; Merrick et al, 1985; Sauter et al, 2002; Sciarretta et al, 1992; Suhr et al, 1988). Second, shortened gut transit time due to accelerated passage of contents through the colon may be involved (Fort et al, 1996). Psychological and psychosomatic factors may also play a role (Hearing et al, 1999; Ros & Zambon, 1987; Stefaniak et al, 2004). As expected given the heterogenous etiology, bile acidbinding agents have had variable effect in the literature (Arlow et al, 1987; Fromm et al, 1987; Sciarretta et al, 1986). Although there is no therapeutic value, it provides a reliable, noninvasive, nonsedating method to evaluate various biliary and pancreatic processes. Further, the images generated can serve as a roadmap for interventional procedures. The test is also valuable in delineating a variety of postcholecystectomy issues beyond retained stones. Furthermore, differentiation between a stenotic and spasmodic papilla is difficult. It carries a sensitivity and specificity of greater than 95% in the detection of obstruction; when pathology is seen, therapeutic sphincterotomy, stent placement, and/ or tissue collection for presumed cancer are possible (Buscarini et al, 2003; Palazzo et al, 1995; Prat et al, 1996; Snady et al, 1992). Acute pancreatitis is the most common complication and occurs in 5% to 40% of low- and high-risk patients, respectively. Additionally, pancreatic necrosis, duodenal or biliary tree perforation, multiorgan failure, and death may also occur, albeit less than 1% of the time (Barthet et al, 2002; Dancygier & Nattermann, 1994; Lieb & Draganov, 2007; Masci et al, 2001). Hepatobiliary Scintography In patients who have undergone cholecystectomy, nuclear scanning reveals rapid flow of intravenously administered technetium-99m hepatobiliary radiopharmaceuticals. In patients with a suspected bile leak, biliary scintigraphy has a sensitivity of as high as 70%. First, the study does not evaluate extrabiliary structures and thus has little to no ability to diagnose complications beyond bile leak. Third, biliary scintigraphy is less sensitive in the setting of hepatic dysfunction. Postcholecystectomy complications such as dropped stones, abscesses, hematomas, or hernias can also be readily detected.
Tanaka K symptoms week by week generic baycip 500mg, et al: Portal vein obstruction accompanied by intrahepatic stones, Angiology 47:11511156, 1996. Tashiro S, et al; Committee for Registration of the Japanese Study Group on Pancreaticobiliary Malfunction: Pancreaticobiliary malfunction: retrospective and nationwide survey in Japan, J Hepatobiliary Pancreat Surg 10:345351, 2003. Tocchi A, et al: Late development of bile duct cancer in patients who had biliary-enteric drainage for benign disease: a follow-up study of more than 1,000 patients, Ann Surg 234:210214, 2001. Trauner M, et al: Molecular pathogenesis of cholestasis, N Engl J Med 339:12171227, 1998. Tsuchida Y, et al: Development of intrahepatic biliary stones after excision of choledochal cysts, J Pediatr Surg 37:165167, 2002. Tsunoda T, et al: Long-term results of surgical treatment for intrahepatic stones, Jpn J Surg 15:455462, 1985. Tsuyuguchi T, et al: Ten-year long-term results after non-surgical management of hepatolithiasis, including cases with choledochoenterostomy, J Hepatobiliary Pancreat Sci 21:795800, 2014. Uchiyama K, et al: Indication and procedure for treatment of hepatolithiasis, Arch Surg 137:149153, 2002. Uchiyama K, et al: Reducing residual and recurrent stones by hepatectomy for hepatolithiasis, J Gastrointest Surg 11:626630, 2007. Uenishi T, et al: Outcomes of hepatic resection for hepatolithiasis, Am J Surg 198:199202, 2009. Uno K, et al: Development of intrahepatic cholelithiasis long after primary excision of choledochal cysts, J Am Coll Surg 183:583588, 1996. Vetrone G, et al: Surgical therapy for hepatolithiasis: a Western experience, J Am Coll Surg 202:306312, 2006. Watanabe Y, et al: Bile duct cancer developed after cyst excision for choledochal cyst, J Hepatobiliary Pancreat Surg 6:207212, 1999. Yamakawa T, et al: Intrahepatic stones and postoperative choledochoscopy, Gastroenterol Jpn 15:577583, 1980. Yamashita N, et al: Composition of intrahepatic calculi-etiological significance, Dig Dis Sci 33:449453, 1988. Yang T, et al: Hepatectomy for bilateral primary hepatolithiasis: a cohort study, Ann Surg 251:8490, 2010. Yarmuch J, et al: Result of surgical treatment in patients with Western intrahepatic lithiasis, Hepatogastroenterology 36:128131, 1989. Zen Y, et al: Different expression patterns of mucin core proteins and cytokeratins during intrahepatic cholangiocarcinogenesis from biliary intraepithelial neoplasia and intraductal papillary neoplasm of the bile duct: an immunohistochemical study of 110 cases of hepatolithiasis, J Hepatol 44:350358, 2006. Zhou F, et al: Laparoscopic hepatectomy is associated with a higher incident frequency in hepatolithiasis patients, Surg Today 43:1371 1381, 2013. The disease may involve any or all portions of the extrahepatic biliary system and causes a progressive obstruction of the biliary tree, leading to cholestasis, cirrhosis, and, ultimately, death within the first several years of life if left untreated. To date, however, no identified mutation has been shown to cause biliary atresia in animal models, thereby underscoring the importance of the interplay between genes and environment. Although the production and effects of these cytokines are predominantly within affected tissues, serum levels of these and other inflammatory markers have been studied to identify possible biomarkers of disease severity. This hypothesis has been supported by work that has identified polymorphisms in genes that regulate the metabolism of inflammatory cytokines as well as contribute to the development of biliary fibrosis (Garcia-Barcelo et al, 2010). Whether maternal liver grafts fare better due to tolerogenesis secondary to maternal microchimerism or paternal allografts fare worse because of specific rejection of paternal antigens remains an active area of investigation. It is most commonly observed in East Asian countries, with a reported incidence as high as 1 in 5,000 to 10,000 live births (Shim et al, 1974; Nio et al, 2003; Tiao et al, 2008). Currently, causative genetic mutations and clear inheritance patterns that would explain these racial and geographic variations have yet to be discovered. The nature of that specific antigen, has for some time been a source of considerable debate, with some researchers proposing a primary autoimmune response to antigens within the biliary epithelium, whereas others suggest infection with a hepatotropic virus, such as cytomegalovirus, reovirus, or rotavirus, as the instigating event. Although these theories have found support in animal models in which inoculation with viruses, such as rotavirus and reovirus, early in life produces biliary inflammation, studies in humans have been less clear-cut, with the identification of an instigating virus found in some, but not all, series (Mack, 2007). Without timely intervention, all patients go on to experience liver fibrosis and cirrhosis, with associated symptoms such as ascites and splenomegaly (see Chapters 76 and 78). Due to the lack of bile flow, fat and fat-soluble vitamin malabsorption often develops in patients, leading to vitamin K deficiency, coagulopathy, and death from intracranial or gastrointestinal hemorrhage. In as many as 50% of patients, initial stools are normal appearing, with the development of acholic stools only occurring several weeks later as biliary obstruction becomes progressively worse. Despite these advancements in noninvasive imaging of hepatobiliary anatomy, intraoperative cholangiography remains the gold standard for diagnosing biliary atresia. Preoperative liver biopsy has become an increasingly safe and used method to help exclude other causes of neonatal jaundice (Balistreri, 1985). Aminotransferases (aspartate aminotransferase and alanine aminotransferase) are frequently only moderately elevated, with albumin, total protein, white blood cell, and hemoglobin levels all within normal range. Notably, infants with severe cases of hepatitis may exhibit impaired radiotracer uptake and thus have limited excretion into the bowel. Additionally, given the progressive nature of biliary atresia, some infants with the condition may initially demonstrate some flow of radiotracer into the duodenum with the gradual obliteration of this tract later in the disease. Currently, there is no evidence to support preoperative bowel preparation, and although used by some surgeons, this is not a widely accepted practice. In this procedure, the extrahepatic biliary tree is excised, and the fibrous portal plate at the hilum of the liver is transected and anastomosed to a Roux-en-Y limb, thereby allowing drainage of bile from the small ductules located within the portal plate. The operation may be performed through a small incision in the right upper abdomen. Upon entry, the abdomen is grossly inspected to identify any evidence of associated anomalies, such as intestinal malrotation or abnormalities of the spleen and portal vein, before turning attention to the liver and biliary tract.
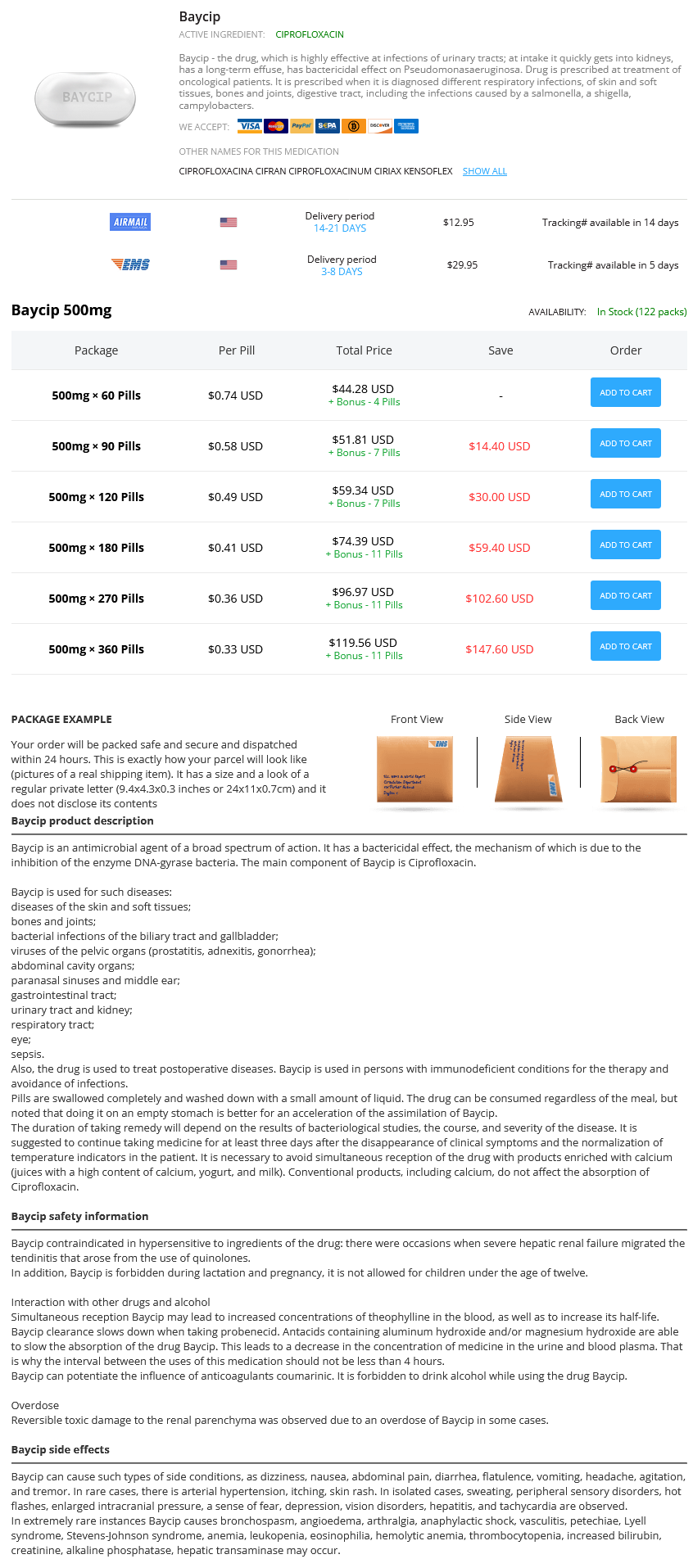
Baycip Dosage and Price
Baycip 500mg
- 60 pills - $44.28
- 90 pills - $51.81
- 120 pills - $59.34
- 180 pills - $74.39
- 270 pills - $96.97
- 360 pills - $119.56
The distal end of the indwelling guidewire can be grasped with forceps or snare medicine woman generic baycip 500mg line, withdrawn through the accessory channel, and a cannulation catheter backloaded over the guidewire and readvanced to the papilla. Alternatively, biliary cannulation can be accomplished in the standard retrograde fashion adjacent to the indwelling wire. In aggregate, success and complication rates reported from small case series are 77% and 5%, respectively (Iwashita et al, 2014). Whether it is through an intrahepatic or extrahepatic approach, a therapeutic linear echoendoscope is used to visualize the bile duct from the stomach or small intestine. A, Cholangiogram showing complete distal bile duct obstruction with diffuseupstreamdilation. The diagnostic yield of brush cytology for biliary strictures is low, with most studies reporting poor sensitivity of 27% to 56% (Victor et al, 2012). Neither longer cytology brush designs nor prebrushing stricture dilation have conclusively shown improvement in sensitivity (de Bellis et al, 2003; Fogel et al, 2006). The poor sensitivity of brush cytology has often been attributed to sampling error and low cellular yield due to the scirrous nature of cholangiocarcinoma, and due to the fact that pancreatic adenocarcinomas frequently cause only extrin sic compression of the distal bile duct, rather than frank invasion. The technique involves advancing the sheathed cytology brush over a guide wire into the bile duct. The brush is advanced beyond the end of the sheath and multiple to and fro movements are performed with the brush across the stricture. A variety of flexible forceps are available in adult (7 Fr) and pedi atric (5 to 6 Fr) calibers. A prior sphincter otomy may facilitate this process, although it is not essential in the presence of an indwelling guidewire in the biliary system (Lin et al, 2003). Although previous studies have suggested that tissue sampling with forceps provides the highest yield for Chapter 29 Interventional endoscopy: technical aspects 523 detection of malignancy (de Bellis et al, 2003), a recent meta analysis indicates that both brushings and biopsy are compa rable (pooled sensitivity of 45% and 48%, respectively) (Navaneethan et al, 2015). Molecular Analysis of Tissue Samples Chromosomal abnormalities are typically seen in malignant biliary strictures (see Chapter 9C). Furthermore, flow cytometric analysis requires large cellular samples, which can be challenging with current endoscopic tissue sampling techniques. It should be stressed that a multidisciplinary review of the indication for intrabiliary tissue sampling is of critical importance. Some stric tures do not require biopsy if surgery is indicated on clinical and radiologic grounds, and other biopsy approaches may be more appropriate. Advanced Endoscopic Biliary Imaging Peroral Cholangioscopy Peroral cholangioscopy is a technique that permits direct endo scopic visualization of the bile ducts by using miniature endo scopes and catheters inserted through the accessory port of a duodenoscope. In the endoscopebased ("motherdaughter") system, a small, thin endoscope (daughter) is inserted through the accessory channel of the duodenoscope (mother). The main limitation of this system is the requirement of two separate endoscopists to operate each scope during the procedure. In this system, an independent instrument with a fourlumen catheter and an operator interface that allows four way tip deflection is attached at the shaft of the duodenoscope. A biliary sphincterotomy is often required to allow passage of the catheter into the duct. Peroral cholangioscopy has been primarily used for the man agement of refractory choledocholithiasis (discussed earlier in this chapter) and for the evaluation of indeterminate biliary strictures. In a prospective multi center study, cholangioscopy was able to distinguish malignant from benign biliary lesions in 92% of cases by visualization alone (Osanai et al, 2013). Furthermore, direct visualization during cholangioscopy also permits selective targeted tissue sampling, with studies showing adequate biopsies in 72% to 97% of cases (Chen et al, 2011; Draganov et al, 2011) and an accuracy for malignant lesions as high as 87% (Kalaitzakis et al, 2012). Peroral cholangioscopy has also been used for the diagnosis of malignancy in primary sclerosing cholangitis (Tischendorf et al, 2006) and evaluation of biliary complica tions following liver transplantation (Balderramo et al, 2013). Overall, cholangioscopy represents an evolving novel technol ogy for the evaluation of undifferentiated biliary strictures, exclusion of occult malignancy, and management of biliary stones. This advantage is hindered by the limited depth of penetration and ability to examine more distal sites. Imaging is achieved by the projection of a lowpower laser light passed through a confocal aperture. The focused beam targeted on a specific layer of tissue is then captured by a pho todetection device and transformed into electrical signals pro cessed into grayscale images (Nakai et al, 2014). The lack of contrast uptake by neoplastic tissue results in a contrasted dark appearance compared with adjacent normal structures. The laser (488 nm, blue light) is transmit ted through thousands of optimal fibers within the probe (cholangioflexprobe is 9 mm in diameter), and subsequent confocal image data are collected at a frame rate of 12 frames/ second with a limited field of vision of 325 µm. The middle hypoechoic layer corresponds to the discontinuous fibromus cular layer, whereas the outermost hyperechoic layer represents the subserosal fat plane (Tantau et al, 2008). These criteria include the presence of a hypoechoic mass, disruption of the normal bile duct structure, abnormal stricture borders (asymmetry, notching), or the pres ence of suspicious lymph nodes (>1 cm, hypoechoic, round with smooth borders). Balderramo D, et al: Prospective evaluation of singleoperator peroral cholangioscopy in liver transplant recpients requiring an evaluation of the biliary tract, Liver Transpl 19(2):199206, 2013. Barkun A, et al: Update on endoscopic tissue sampling devices, Gastrointest Endosc 63:7177, 2006. Cahen D, et al: Longterm results of endoscopic drainage of common bile duct strictures in chronic pancreatitis, Eur J Gastroenterol Hepatol 52:5563, 2005. Choudhary A, et al: Effect of precut sphincterotomy on postendoscopic retrograde cholangiopancreatography pancreatitis: a systematic review and metaanalysis, World J Gastroenterol 20(14):40934101, 2014.