General Information about Azithromycin
Azithromycin's effectiveness towards respiratory infections is due to its capacity to penetrate into the tissues and fluids of the lungs. This allows it to fight micro organism which have settled in these areas and may be inflicting signs corresponding to coughing, congestion, and difficulty breathing. In addition, azithromycin has anti-inflammatory properties, which may help relieve symptoms and speed up restoration time.
In conclusion, azithromycin is a broadly used and efficient antibiotic for the therapy of varied bacterial infections, particularly these affecting the respiratory system. Its handy dosing routine and low risk of unwanted effects make it a popular alternative among healthcare providers and patients alike. However, as with all drugs, it may be very important use azithromycin solely as directed and underneath the supervision of a healthcare skilled.
Azithromycin is generally well-tolerated and has a comparatively low danger of side effects. The most typical unwanted aspect effects reported embody abdomen upset, diarrhea, and nausea. These signs are usually delicate and resolve rapidly. In uncommon circumstances, azithromycin may cause allergic reactions, which might vary from delicate rashes to severe anaphylaxis. It is necessary to hunt medical attention if any concerning side effects occur while taking this medication.
Aside from its use as an antibiotic, azithromycin has additionally been found to have anti-inflammatory and immunomodulatory effects. This signifies that it might possibly help cut back inflammation and increase the physique's immune response to infections. This may be significantly helpful for sufferers with continual respiratory situations, similar to asthma, who are at the next risk of developing infections and experiencing extra extreme symptoms.
Another common use for azithromycin is within the remedy of pneumonia. Pneumonia is a severe an infection of the lungs that can be brought on by various bacteria, viruses, and fungi. Azithromycin is especially effective towards Mycoplasma pneumoniae and Legionella pneumophila, two frequent bacterial causes of pneumonia, and is usually prescribed as a first-line remedy for these infections.
Azithromycin can be generally used to deal with infections of the pores and skin and gentle tissue, such as cellulitis and impetigo. It could be prescribed as a standalone remedy or in combination with different medications, relying on the severity and kind of infection. Its efficacy against skin infections is as a result of of its ability to target and kill the micro organism that generally cause these situations, similar to Staphylococcus aureus and Streptococcus pyogenes.
One of the commonest uses of azithromycin is for infections of the higher and decrease respiratory tract. It is a first-line treatment for common circumstances similar to ear infections, sinusitis, and bronchitis. These infections may be attributable to a variety of micro organism, together with Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis, all of that are susceptible to azithromycin.
Azithromycin, generally identified by its brand name Zithromax, is a generally prescribed macrolide antibiotic used to deal with a wide selection of infections. It is effective against each gram-positive and gram-negative micro organism, making it a flexible and broadly used treatment.
One factor that sets azithromycin apart from other antibiotics is its convenient dosing routine. It is often prescribed in a once-daily dose, for a shorter length than different antibiotics, making it a convenient possibility for sufferers who have hassle sticking to a more frequent dosing schedule. This additionally reduces the risk of developing antibiotic resistance, which may occur when a medication is taken for a chronic time frame.
Some practitioners place all of the drug at one point antimicrobial beer line buy 250 mg azithromycin overnight delivery, and others distribute the dose evenly among three points. Typical doses range from 1018 units of Botox or 2530 units of Dysport depending on the estimate of muscle mass and activity. Great care must be taken to make the injections into the skin only, raising wheals or blebs that can be gently massaged down. Intramuscular injection in this area will reliably produce unwanted bruising because of the rich venous plexus underlying the skin in this region. The toxin will readily diffuse from the blebs into the underlying orbicularis muscle, relaxing the grip on the overlying skin and smoothing out the wrinkles. As previously mentioned, care must be taken to avoid injecting too low down onto the malar eminence, where diffusion may affect the zygomaticus major muscle and disrupt the symmetrical movement of the corner of the mouth in smiling. It prevents the problem of rhytides being readily reformed by repeated squinting during the postoperative healing period; in which case, the resurfacing may give rise to more noticeable lines than existed before the resurfacing. These agents provided the first new directions in cosmetic therapy since the introduction of solubilized bovine collagen in the mid-1970s. The ability to control both muscles of expression and their secondary lines and folds, and to repair age-related volume changes in subcutaneous tissue has revolutionized minimally invasive cosmetic techniques. Many patients have eagerly embraced simultaneous treatment with both fillers and botulinum toxin to achieve a natural look and forego more traditional incisional surgery. The pattern of intradermal botulinum toxin injections is shown with the starch-iodine material in place to highlight the injection points (middle panel). One week later the treated axilla shows a negative result on the starch-iodine test (bottom panel). Approximately, 100150 units of Botox are needed to treat a single palm, divided into 5060 intradermal injections of 23 units each. Onset of anhidrosis peaks in 57 days and is accompanied by minor weakness of the intrinsic muscles of the hand, which makes tasks requiring strength and stability. The weakness usually subsides within 3 weeks, whereas the anhidrosis persists for several months. There is wider variation in response to palmar treatment than to axillary treatment, with anhidrosis lasting from 412 months, which probably reflects the technical difficulties in achieving even dispersion of the toxin through the palmar skin. Anesthesia may be achieved with a eutectic mixture of local anesthetics but is usually not needed due to the relative insensitivity of the axillary skin. Reliable anhidrosis is produced within 72 hours and will last for 812 months with doses of 50100 units of Botox per axilla. The duration of effect appears to be dose related, and doses of up to 200 units (Dysport) per axilla have been reported to produce dryness for up to 29 months. The right hand received 100 units of intradermal Botox 1 week before the photograph was taken. Minor discomfort can be made more tolerable in some patients by pretreating the injection site areas with topical anesthetic and using sterile saline with preservative as a diluent, which greatly reduces the sensation of injection. The more problematic complications to consider are eyelid ptosis, which can occur after injections in the glabellar brow. Antibody-mediated resistance appears to be an exceedingly rare event and of little clinical consequence in cosmetic dermatologic uses of botulinum toxin. Although millions of doses have been given to date, there is no well-documented evidence of the development of immunologic resistance in patients treated with cosmetic doses. Resistance continues to be observed in patients treated for cervical dystonia, albeit at much lower rates than in the early years, probably due to the lower protein content of current formulations. Eyelid ptosis is thought to be best avoided by carefully placing the midbrow injections at a minimal distance of 1 cm from the superior orbital rim, keeping the injection rate slow and gentle, and having the patient avoid prone positions and sleeping for 2 hours after injection. Restricting injections to the upper two-thirds of the frontalis and reducing doses to the minimum necessary to produce the desired clinical effect may minimize brow ptosis. Headaches as a rebound phenomenon after facial injections of botulinum toxin may be triggered by unopposed muscle groups, but their etiology is unclear. In hyperhidrosis, palmar weakness is a predictable consequence of injecting the palms. There is no similar effect of any clinical significance in either the axillae or the feet. Further evolution will occur as new serotypes come to market and greater therapeutic synergies evolve as developers of soft-tissue augmentation systems strive to achieve similar effect and elegance. The high degree of efficacy and safety in the use of botulinum toxins in cosmetic dermatology has produced a great level of satisfaction in patients and physicians alike. Carruthers J, Carruthers A: the evolution of botulinum neurotoxin type A for cosmetic applications. Ascher B et al: A multicenter, randomized, double-blind, placebo-controlled study of efficacy and safety of 3 doses of botulinum toxin A in the treatment of glabellar lines. Clin Dermatol 22:45, 2004 41 Chapter 256:: Hair Transplantation and Alopecia reduction:: Walter P. In women, this corresponds to the frontal area and the part-line, which is usually a 5-mm-wide anteroposterior corridor. The thickened hair in these areas can then be styled in a way that camouflages untreated areas. When this is done, the cosmetic improvement is significant, and patient satisfaction is high. Most often, hairs grow in small groupings of two to five hairs, as shown in the above photo. Commonly, each transplant session treats one of the three major areas, plus adjacent evolving areas. Occasionally, the treat- ment of evolving areas of hair loss is deferred to later sessions in order to transplant a larger proportion of obvious areas of hair loss.
If the vial form is used antibiotics for uti sepsis buy generic azithromycin 100 mg line, it is necessary to use a U100-insulin syringe or tuberculin syringe to measure doses. Species Source Human analog Human analog Human analog Human Human Human Human analog Human analog Human analog Human Human analog Human analog Human analog Human analog Concentration U100, U200 U100 U100 U100, U500 - U100 U100, U300 U100 U100, U200 U100 U100 U100 U100 U100 All insulins are now made by recombinant technology; they should be refrigerated and brought to room temperature just before injection. The physician should then carefully note dosages in both units and volume to avoid overdosage. The disposable pen avoids this conversion issue and dispenses the regular U500 insulin in 5-unit increments. Intravenous infusions of regular insulin are particularly useful in the treatment of diabetic ketoacidosis and during the perioperative management of insulin-requiring diabetics. Rapidly acting insulin analogs-Insulin lispro (Humalog) is an insulin analog in which the proline at position B28 is reversed with the lysine at B29. Insulin aspart (Novolog) is a single substitution of proline by aspartic acid at position B28. Insulin glulisine (Apidra) differs from human insulin in that the amino acid asparagine at position B3 is replaced by lysine and the lysine in position B29 by glutamic acid. When injected subcutaneously, these three analogs quickly dissociate into monomers and are absorbed very rapidly, reaching peak serum values in as little as 1 hour. The amino acid changes in these analogs do not interfere with their binding to the insulin receptor, with the circulating half-life, or with their immunogenicity, which are all identical to those of human regular insulin. Clinical trials have demonstrated that the optimal times of preprandial subcutaneous injection of comparable doses of the rapid-acting insulin analogs and of regular human insulin are 15 minutes and 45 minutes before the meal, respectively. Although the more rapid onset of action has been welcomed as a great convenience by patients with diabetes who object to waiting as long as 45 minutes after injecting regular human insulin before they can begin their meal, patients must be taught to ingest adequate absorbable carbohydrate early in the meal to avoid hypoglycemia during the meal. Another desirable feature of rapidly acting insulin analogs is that their duration of action remains at about 4 hours for most commonly used dosages. This contrasts with regular insulin, whose duration of action is significantly prolonged when larger doses are used. In a double-blind crossover study comparing insulin lispro with regular insulin in insulin pumps, persons using insulin lispro had lower HbA1c values and improved postprandial glucose control with the same frequency of hypoglycemia. However, the concern remains that in the event of pump failure, users of the rapidly acting insulin analogs will have more rapid onset of hyperglycemia and ketosis. While insulin aspart has been approved for intravenous use (eg, in hyperglycemic emergencies), there is no advantage in using insulin aspart over regular insulin by this route. A U200 concentration of insulin lispro is available in a disposable prefilled pen. The only advantage of the U200 over the U100 insulin lispro preparation is that it delivers the same dose in half the volume. Individual insulin molecules slowly dissolve away from the crystalline depot and provide a low, continuous level of circulating insulin. Separate syringes must be used to minimize the risk of contamination and subsequent loss of efficacy. The absorption pattern of insulin glargine appears to be independent of the anatomic site of injection, and this drug is associated with less immunogenicity than human insulin in animal studies. Insulin detemir-In this insulin the terminal threonine is dropped from the B30 position and myristic acid (a C-14 fatty acid chain) is attached to the B29 lysine. These modifications prolong the availability of the injected analog by increasing both self-aggregation in subcutaneous tissue and reversible albumin binding. The duration of action for insulin detemir is about 17 hours at therapeutically relevant doses. It is recommended that the insulin be injected once or twice a day to achieve a stable basal coverage. Insulin Degludec-In this insulin analog, the threonine at position B30 has been removed and the lysine at position B29 is conjugated to hexadecanoic acid via a gamma-l-glutamyl spacer. In the vial, in the presence of phenol and zinc, the insulin is in the form of dihexamers but, when injected subcutaneously, it self-associates into large multihexameric chains consisting of thousands of dihexamers. The chains slowly dissolve in the subcutaneous tissue, and insulin monomers are steadily released into the systemic circulation. Its onset of action is in 3090 minutes, and its duration of action is more than 42 hours. Insulin degludec is available in two concentrations, U100 and U200, and dispensed in pre-filled disposable pens. Consequently, over time, the soluble component becomes a mixture of regular and rapidly acting insulin analog at varying ratios. A similar 70% insulin aspart protamine/30% insulin aspart (NovoLog Mix 70/30) is now available. The main advantages of these new mixtures are that (1) they can be given within 15 minutes of starting a meal and (2) they are superior in controlling the postprandial glucose rise after a carbohydrate-rich meal. Insulin glargine or insulin detemir cannot be acutely mixed with either regular insulin or the rapid-acting insulin analogs. Insulin degludec, however, can be mixed and is available as 70% insulin degludec/30% insulin aspart and is injected once or twice a day. Alternatively, the meal or snack dose algorithm (grams of carbohydrate covered by a unit of insulin) and insulin sensitivity or blood glucose correction factor (fall in blood glucose level in response to a unit of insulin) can be preprogrammed into the pump. If the user enters the carbohydrate content of the food and current blood glucose value, the insulin pump will calculate the most appropriate dose of insulin.
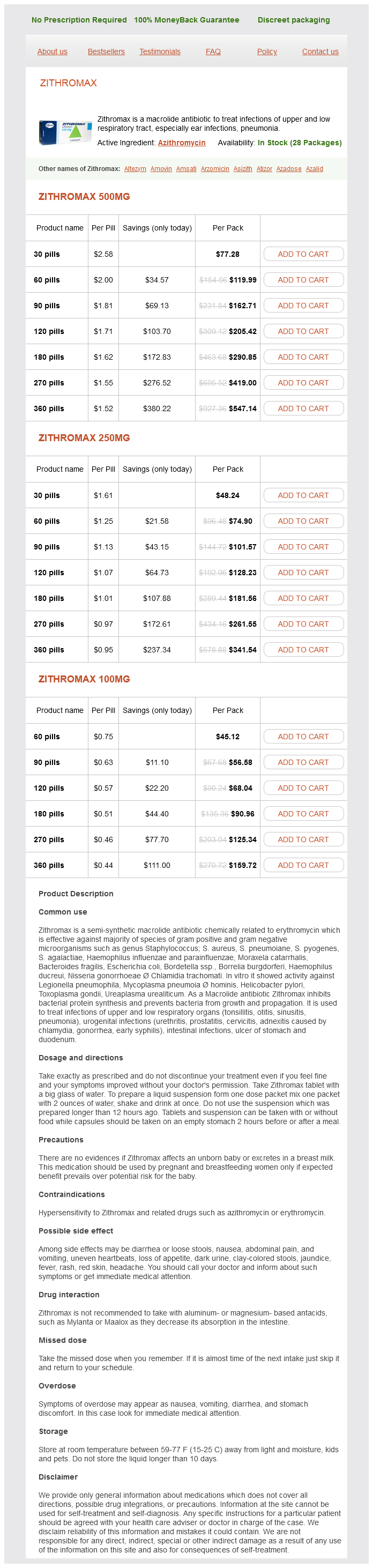
Azithromycin Dosage and Price
Zithromax 500mg
- 30 pills - $77.28
- 60 pills - $119.99
- 90 pills - $162.71
- 120 pills - $205.42
- 180 pills - $290.85
- 270 pills - $419.00
- 360 pills - $547.14
Zithromax 250mg
- 30 pills - $48.24
- 60 pills - $74.90
- 90 pills - $101.57
- 120 pills - $128.23
- 180 pills - $181.56
- 270 pills - $261.55
- 360 pills - $341.54
Zithromax 100mg
- 60 pills - $45.12
- 90 pills - $56.58
- 120 pills - $68.04
- 180 pills - $90.96
- 270 pills - $125.34
- 360 pills - $159.72
The drug is administered at a dosage of 810 mg/kg/d in three divided doses with meals for 6090 days virus definition update cheap azithromycin online american express. Adverse effects include nausea, vomiting, abdominal pain, fever, rash, headache, restlessness, insomnia, neuropathies, and seizures. Miltefosine may also have a role in the treatment of cutaneous leishmaniasis; the drug was noninferior to meglumine antimoniate for this indication in South American children. Liposomal amphotericin has shown excellent efficacy at a dosage of 3 mg/kg/d intravenously on days 15, 14, and 21. Other regimens that have shown good efficacy in India include 4 doses of 5 mg/kg over 410 days and a single dose of 15 mg/kg. With single-dose therapy, an amphotericin lipid emulsion had similar efficacy to that of the liposomal formulation. Nonliposomal amphotericin (1 mg/kg intravenously every other day for 30 days) is more toxic, less expensive, also efficacious, and widely used in India. The use of amphotericin, and especially liposomal preparations, is limited in developing countries by difficulty of administration, cost, and toxicity. In initial studies, paromomycin was well tolerated, with common mild injection pain, uncommon ototoxicity and reversible liver enzyme elevations, and no nephrotoxicity. Paromomycin has also shown good efficacy when topically applied, alone or with gentamicin, for the treatment of cutaneous leishmaniasis. It was also recently shown to be effective in regimens including a single dose of liposomal amphotericin followed by 714 days of miltefosine. The drug should Drug Combinations Used in the Treatment of Visceral Leishmaniasis the use of drug combinations to improve treatment efficacy, shorten treatment courses, and reduce the selection of resistant parasites has been an active area of research. In a trial in East Africa, compared to a standard 30-day course of sodium stibogluconate, similar efficacy was seen with a 17-day course of sodium stibogluconate plus paromomycin. Rehman K, et al: Haemolysis associated with the treatment of malaria with artemisinin derivatives: a systematic review of current evidence. Bukirwa H et al: Artesunate plus pyronaridine for treating uncomplicated Plasmodium falciparum malaria. Ben Salah A et al: Topical paromomycin with or without gentamicin for cutaneous leishmaniasis. Burza S et al: Five-year field results and long-term effectiveness of 20 mg/kg liposomal amphotericin B (Ambisome) for visceral leishmaniasis in Bihar, India. Lutje V, Seixas J, Kennedy A: Chemotherapy for second-stage human African trypanosomiasis. Rassi A Jr, Rassi A, Marcondes de Rezende J: American trypanosomiasis (Chagas disease). Sundar S et al: Comparison of short-course multidrug treatment with standard therapy for visceral leishmaniasis in India: An open-label, non-inferiority, randomised controlled trial. Sundar S et al: Efficacy and safety of amphotericin B emulsion versus liposomal formulation in Indian patients with visceral leishmaniasis: a randomized, open-label study. Sundar S, Singh A: Recent developments and future prospects in the treatment of visceral leishmaniasis. Sundar S et al: Single-dose liposomal amphotericin B for visceral leishmaniasis in India. She should be hospitalized and treated urgently with intravenous artesunate or, if this is unavailable, intravenous quinine or quinidine. His father and sister have undergone resection of abdominal masses, but details of their diagnoses are unavailable. More than 1 billion people are infected with intestinal nematodes, and many millions are infected with filarial nematodes, flukes, and tapeworms in other organs. In other cases, complete elimination of parasites is the goal of therapy, although this goal can be challenging with certain helminthic infections, because of both limited efficacy of drugs and frequent reinfection after therapy in endemic areas. Table 531 lists the major helminthic infections and provides a guide to the drug of choice and alternative drugs for each infection. It reaches variable maximum plasma concentrations about 3 hours after a 400-mg oral dose, and its plasma half-life is 812 hours. Benzimidazoles are thought to act against nematodes by inhibiting microtubule synthesis. Ascariasis, trichuriasis, and hookworm and pinworm infections-For adults and children older than 2 years with ascariasis and pinworm infections, the treatment for ascariasis is a single dose of 400 mg orally (repeated daily for 23 days for heavy infections and in 2 weeks for pinworm infections). For hookworm infections and trichuriasis, albendazole at 400 mg orally once daily for 3 days is now recommended, with albendazole showing improved efficacy over mebendazole. It is more active against Echinococcus granulosus than against Echinococcus multilocularis. Neurocysticercosis-Indications for medical therapy for neurocysticercosis are controversial, since antihelminthic therapy is not clearly superior to therapy with corticosteroids alone and may exacerbate neurologic disease. Corticosteroids are usually given with the antihelminthic drug to decrease inflammation caused by dying organisms. Albendazole is now generally considered the drug of choice over praziquantel because of its shorter course, lower cost, improved penetration into the subarachnoid space, and increased drug levels (as opposed to decreased levels of praziquantel) when administered with corticosteroids. Albendazole combined with praziquantel improves efficacy in patients with multiple brain cysts. Other infections-Albendazole is the drug of choice in the treatment of cutaneous larva migrans (400 mg daily for 3 days), visceral larva migrans (400 mg twice daily for 5 days), intestinal capillariasis (400 mg daily for 10 days), microsporidial infections (400 mg twice daily for 2 weeks or longer), and gnathostomiasis (400 mg twice daily for 3 weeks). It also has activity against taeniasis (400 mg daily for 3 days), trichinosis (400 mg twice daily for 12 weeks), and clonorchiasis (400 mg twice daily for 1 week).